CASO CLÍNICO
DOI 10.25176/RFMH.v19i3.2152
1 Edgardo Rebagliati Martins Hospital, Emergency Department, EsSalud, Lima-Peru.
aEmergency Physician.
bSurgeon.
ABSTRACT
Patient used for 82 years. Emergency service to present a time of illness of 15 days with hyporexia, dysarthria, rigidity of upper and lower limbs, general condition, periodic with edema, skin lesions and sensory disorder, bradycardia. sustained Therefore, at the beginning, it presents as a problem of respiratory insufficiency, sensory disorder to rule out a stroke. Patient worsens with greater sensory and hemodynamic compromise refers to myxedema coma by applying the Clinical Score of Coma Mixedematoso, treatment is started, patient dies.
Keywords: Mixedematous coma, hypothyroidism and sensory disorder. (Source: MeSH NLM)
RESUMEN
Paciente varón de 82 años que ingresa al Servicio de Emergencia por presentar un tiempo de enfermedad de 15 días con hiporexia, disartria, rigidez de miembros superiores e inferiores, en mal estado general, pícnico con edema, lesiones en piel y trastorno del sensorio, bradicardia sostenida; por lo cual al inicio se plantea como problema de insuficiencia respiratoria, trastorno del sensorio a descartar un accidente cerebro vascular. Paciente empeora con mayor compromiso del sensorio y hemodinámico se plantea diagnóstico de Coma Mixedematoso aplicando el Score Clínico de Coma Mixedematoso, se inicia tratamiento, paciente fallece.
Palabras clave:Coma mixedematoso; Hipotiroidismo; Trastorno del sensorio. (Fuente: DeCS BIREME)
INTRODUCTION
Myxedema coma (MC) is an endocrine emergency, of rare presentation, potentially fatal, that represents severe hypothyroidism, which can lead to hemodynamic instability and multisystemic complications1,2. The estimated incidence is 0.22 per million people / year3, the mortality rate is around 40%, but currently, with the advances of intensive therapy have decreased to 20 - 25%; It mainly affects women with a ratio of 8: 1, especially older women in 80% of cases4,5.
A Myxedema coma may be associated with a wide range of systemic abnormalities, with cardiovascular disorders being one of the most frequent, including increased levels of cardiac enzymes and bradycardia1,5.
We present the case of an 82-year-old male patient with myxedema coma with undiagnosed hypothyroidism who presents with dysarthria, the rigidity of limbs and bradycardia, with a 15-day evolution time and with progressive deterioration of consciousness level during the internment. This case report was prepared following the Case Report6.
CASE REPORT
Information of the patient
An 82-year-old male, a native of Lima, retired, with a history of diffuse interstitial lung disease (DILD) without treatment, hypertension (HTA) both diagnosed a year ago, receives valsartan 80mg / day orally and furosemide 40mg / day conditional to edema of lower limbs. Family member states that he starts the condition 15 days before admission to the hospital, with hyporexia, difficulty speaking, knee pain, stiffness in the upper and lower limbs that makes walking difficult until bed rest, 3 days before his admission he emits incomprehensible words; so he goes to Emergency.
Clinical findings
At physical examination awake patient, does not collaborate, no cyanosis, with blood pressure 163 / 83mmHg, heart rate of 39x min, respiratory rate of 22 x min, oxygen saturation 92%, in poor general condition; pyknic biotype, bloated facial appearance, symmetrical lower limb edema, ecchymosis on forearms, with dry skin and signs of desquamation, hypochromic lesions on face, forehead, chest, hands and pretibial region; with hypoventilation in bases, not audible rattles; regular low-pitched heart sounds, bradycardic; globular abdomen, audible hydro-aerial noises, soft depressible, not painful on palpation; Glasgow coma scale 12 points (ocular aperture = 4, verbal response = 2, motor response = 6), reactive isochoric pupils, negative Babinski.
Diagnostic evaluation
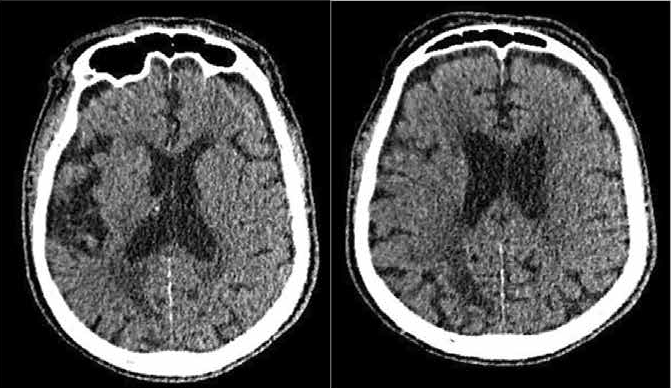
A Patient who entered the emergency service with the problems of altered consciousness, hypoxemic acute respiratory failure - hypercapnic, severe sinus bradycardia; therefore, the diagnosis of ischemic cerebrovascular accident, metabolic encephalopathy, exacerbated EPID associated with an infection of the lower respiratory tract, sinus node dysfunction secondary to an acute coronary syndrome was raised. Laboratory tests are performed (Table 1) and brain tomography without contrast, no ischemic or hemorrhagic lesions are evident (Figure 1). It is evaluated by cardiology and neurology, where it is suggested to add atropine to therapeutics and investigate other causes of the alteration of consciousness.
Interveción terapéutica
Water replacement was initiated with crystalloids at 80cc / Kg, omeprazole 40 mg intravenously, atorvastatin 40 mg, and atropine 0.5 mg intravenous (EV) conditional. At 17 hours of admission to the emergency room, he presents hypotension, deterioration of neurological status and worsening of respiratory distress, so the central venous line initiates dopamine 10ug / kg/min and endotracheal tube (ETT) is placed to provide support with mechanical ventilation invasive (VMI) with pulmonary protective strategy. When there is suspicion of myxedematous Coma intravenous hydrocortisone 100mg is added every 8 hours and levothyroxine 300ug by nasogastric tube (SNG) because we did not have levothyroxine presentation in ampoules. Later, 2 mg EV every 24 hours and metronidazole 500 mg every 8 hours were added to the antibiotic therapy, with suspicion of infection with the abdominal starting point (intestinal obstruction). At 48 hours after admission, noradrenaline was added at 0.5ug /, and dopamine was exchanged for dobutamine 0.5ug/kg/min, methylprednisolone 500 mg was added every 12 hours and antibiotic coverage was rotated to intravenous meropenem 1g every 12 hours. Intravenous vancomycin 1g every 24 hours, doses adjusted to its glomerular filtration rate, but despite everything, it evolves unfavorably and dies on the fourth day of hospitalization.
Monitoring and results
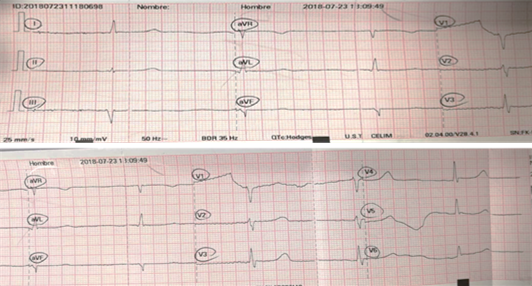
Patient at 17 hours after admission, he presented with hypotension and deterioration of his neurological state, with a decrease in the Glasgow Scale of 12 to 6 points (with brain tomography without images of ischemia or hemorrhage). He was evaluated by cardiology for persistent bradycardia (Figure 2) with hypotension due to suspicion of cardiogenic shock and/or sinus node dysfunction, so dopamine 10ug / kg/min is initiated. After the negative troponin results (0.097 pg/dl), the need for a pacemaker is ruled out. Due to the deterioration of the neurological state, endotracheal intubation is started, and invasive mechanical ventilation (IMV) is initiated. But in addition the patient also presents abdominal distension; In view of such clinical presentation, the possibility of a myxedematous Coma is raised; so it is decided to apply to the patient the Clinical Score of Coma Mixedematoso88, (Table 2) giving a score of 90 points, being the diagnosis of MC high probability, for which thyroid hormones are requested.
The laboratory results indicate severe pancytopenia, leukopenia, 2730 K / ul, anemia (Hb: 9.4 g / dl) and low platelet count of 66,000 K / ul. Additionally, he studied sodium electrolytes (Na) 130 mmol / L, CPK (Creatine phosphokinase) 4135 U / L, CPK-MB 266.42 ng/ml, ProBNP 276 pg/dl and Troponin I: 0.097 pg / dl, in the chest tomography and abdomen (Figure 3), there was bilateral mild pleural effusion, interlobular septal interstitial thickening and ground glass area in upper and middle lobes, colonic frame with great dilatation and pneumatosis at the level of its walls, little free perihepatic and perisplenic fluid, no evidence of open air.
These results in general terms are not indicative of any particular pathology. The results of troponin and the electrocardiogram are not compatible with that of cardiac infarction, and that of ProBNP is also not related to that of decompensated cardiac insufficiency; on the contrary, each of these results is present in the myxedema coma.
Thyroid hormone results were obtained at day 3: TSH 26.2 Uul / ml free T4 <0.30 ng/dl (Table 1), confirming the diagnosis of myxedema coma, after 5 days of admission it did not respond adequately to the hemodynamic and ventilatory support, dying on the fourth day of internment.
| Biochemistry | UM | Reference Value | |
| PCR | 1.5 | mg/dL | 0 – 1 |
| Creatinine | 1.41 | mg/dL | 0.6 – 1.1 |
| Urea | 76.3 | mg/dL | 22 – 55 |
| Glucose | 83 | mg/dL | 74 - 106 |
| Hemogram | |||
| Leukocytes | 2730 | k/ul | 4 – 11 |
| Neutrophils | 83.90% | % | 40 – 74 |
| Abashed | 1% | % | 22 – 55 |
| Hemoglobin | 9.4 | g/dl | 14 – 18 | VCM | 92.1 | fl | 80 – 99 |
| HCM | 33.8 | pg | 27 – 31 |
| Hematocrit | 25.6 | % | 42 – 52 |
| Platelets | 66 | k/ul | 130 - 400 |
| Coagulation Profile | |||
| TP | 14.38 | seg | 11 – 13.5 |
| TTPa | 58.98 | seg | 25 – 37 |
| INR | 1.23 | 0.95 – 1.15 | |
| Fibrinogen | 288.62 | mg/dl | 200 - 400 |
| Electrolytes | |||
| Sodium | 130 | mmol/L | 132 – 146 |
| Potassium | 3.93 | mmol/L | 3.5 – 5.5 |
| Chlorine | 93.5 | mmol/L | 99 – 109 |
| Magnesium | 2.42 | mg/dl | 1.3 – 2.7 |
| Calcium | 9.1 | mg/dl | 8.3 – 10.6 |
| Phosphorus | 4.5 | mg/dl | 2.4 – 5.1 |
| Hormonal profile | |||
| TSH | 26.200 | uUl/ml | 0.4-4.0 |
| Free T4 | < 0.30 | ng/dl | 0.8-1.9 |
| ACTH | 20.20 | pg/ml | 46 |
| Cortisol | 18.00 | ug/dl | 5.0-25.0 |
| Cardiac Profile | |||
| CPK – Creatine phosphokinas | 4135 | U/L | 32 – 294 |
| CPK-MB | 266.42 | ng/ml | 0 – 5 |
| Troponin I | 0.096 | ng/ml | 0.02- 0.06 |
| LDH | 627 | U/L | 120 - 246 |
| Pro-BNP | 267.09 | pg/ml | |
| Liver Profile | |||
| Total Bilirubin | 0.41 | mg/dl | 0.3 – 1.2 |
| Direct Bilirubin | 0.12 | mg/dl | |
| Indirect Bilirubin | 0.29 | mg/dl | |
| Total Proteins | 7.29 | g/dl | 5.7 – 8.2 |
| Albumin | 3.84 | g/dl | 3.2 – 4.8 |
| Globulin | 3.45 | g/dl | 2 – 3.5 |
| Alkaline phosphatase | 72 | U/L | 45 – 129 |
| TGO | 182 | U/L | <34 |
| TGP | 61 | U/L | 10 – 49 |
| Arterial Gases | |||
| PaO2 | 60.3 | mmHg | 60 – 95 |
| PaCO2 | 57.5 | mmHg | 36 – 44 |
| HCO3 | 27.6 | mequival/L | 22 – 26 |
| PH | 7.3 | 7.35 – 7.45 | |
| Lactate | 0.7 | mmol/L | <1 |
| Urine Test | |||
| Leukocytes | 1-2 | X campo | |
| Red blood cells | 0-1 | X campo | |
| Epithelial cells | 1-2 | X campo | |
| Density | 1.014 | ||
| Nitrites | neg | ||
| Thermoregulation Dysfunction (Temperature, °C) | Cardiovascular Dysfunction | ||
| >35 | 0 | Bradycardia | |
| 32-35 | 10 | Absent | 0 |
| <32 | 20 | 50-59 | 10 |
| Central Nervous System Condition | 40-49 | 20 | |
| Absent | 0 | <40 | 30 |
| Somnolent | 10 | EkG changes | 10 |
| Obnubilated | 15 | Pleural / pericardial effusion | 10 |
| Sopor | 20 | Pulmonary edema | 15 | Coma | 30 | Cardiomegaly | 15 |
| Gastrointestinal findings | Hypotension | 20 | |
| Anorexia / abdominal pain / Constipation | 5 | Metabolic disorders | |
| Decreased intestinal motility | 15 | Hyponatremia | 10 |
| Paralytic ileus | 20 | Hypoglycemia | 10 |
| Precipitating events | Hypoxemia | 10 | |
| Missing | 0 | Hypercarbia | 10 |
| Present | 10 | FG decrease | 10 |
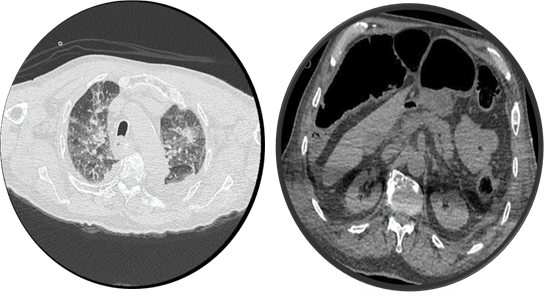
CT chest: Pleural effusion of location in posterior segments of both pulmonary fields and associated scarce component of passive atelectasis of the adjacent lung parenchyma. Rest of pulmonary parenchyma presents interlobular septal interstitial thickening and ground-glass area in upper and middle lobes. Mediastinum diverted to the right. Tracheobronchiosclerosis Digestive tube in the gastric chamber. Endotracheal tube. There is no evidence of significant adenomegalias in the mediastinum. The prominence of the pulmonary artery trunk up to 31 mm atherosclerosis.
TAC abdomen: Liver of morphology and preserved density. Parenchymal calcifications of secular aspect versus granulomatosis. Vesicular not visible, probably collapsed. Bazo, pancreas, adrenals of aspect preserved. Both kidneys are hypodense and with marred edges. The colonic frame is shown with great dilatation and pneumatosis at the level of their osseous structures shows spondylosis changes. It is free perihepatic and perisplenic fluid. Large dilation of thick loops with pneumatosis and free perisplenic and perihepatic fluid.
DISCUSSION
EMC is a clinical entity with the infrequent presentation, it is estimated that the incidence per year is 0.22 / 1000,000 people per year7; due to which it can become a diagnostic problem since its infrequency makes the initial evaluator may not pose it as a diagnosis from the beginning.
In the past, the overall mortality rate from myxedema was 60 to 70% of cases; early recognition and advances in intensive care support have reduced the mortality rate to 20-25%8; that is still high.
Cheng and colleagues, in one study, noted that making an early diagnosis of obvious primary hypothyroidism in the emergency department is challenging: only 21% of patients admitted with a correct initial diagnostic impression9. Perhaps most worrying was that 50% of the patients in the study who were finally diagnosed with myxedema were not diagnosed in the emergency department. This study indicates that the emergency physician does not well recognize the hypothyroid crisis. In the case of our patient, it took 24 hours to consider the diagnostic possibility of myxedema Coma.
Patients with myxedema coma usually present in the winter months, which suggests that external cold may be an aggravating factorsup>10. It coincides with the case of our patient who showed up in July, which is the winter season and one of the coldest months of this city.
The epidemiology of myxedema crisis follows the same pattern as in hypothyroidism and is more common in women and the elderly11. Hypothyroidism is about ten times more frequent in women than in men12. In the case report, the patient was male, 82 years of age, a fact that could have contributed to the delay of the approach as a probable diagnosis.
The hypothyroid patient presents mostly in the emergency department with multiple vague complaints of insidious onset, and they have a nonspecific physical examination, circumstances that can make the diagnosis elusive even for the diligent doctor. The present signs and symptoms often vary with age and gender and the severity of these clinical characteristics vary greatly13. A typical case of the patient in the discussion who had a completely nonspecific clinical evolution since the little information obtained through an indirect anamnesis did not allow to have the patient's background, and the lack of data in his registry did not contribute to an adequate approach. Hypothyroidism should always be considered in patients who present with nonspecific symptoms of the suggestive disease, including weakness, intolerance to cold, and alterations in mental status, and of receiving drugs that impair thyroid function or treatment of advanced cancer of the head and/or neck. Additionally, patients with stable chronic heart failure or unexplained pericardial effusion justify serum thyroid tests9.
Infections and septicemia are the main precipitating factors8. Diseases typically include pneumonia, urinary tract infections, and cellulitis. Cerebrovascular accidents, congestive heart failure, traffic accidents, gastrointestinal bleeding, and several sedative groups can play an important role in the precipitation of myxedema crisis11. A background factor commonly ignored in the myxedema crisis is the discontinuation of thyroid supplementation in critically ill patients. In the case presented, at least the patient had no history of suffering thyroid disease.
The diagnosis of Coma myxedema is mainly clinical. The presence of marked stupor, confusion or coma, and hypothermia in a patient with findings of hypothyroidism is strongly suggestive of myxedema coma. The physical examination is indicative of hypothyroidism: dry, thick and scaly skin, thin or rough hair; edema of the skin and soft parts, macroglossia, hoarse voice and delayed deep tendon reflexes. Other important clinical features of myxedema coma include hypoventilation, bradycardia, decreased cardiac contractility, decreased intestinal motility, paralytic ileus and megacolon12. The highlight of the presented case is that it surprisingly presented all these clinical characteristics when performing the physical examination; cold skin, edema, preserved blood pressure that evolved to hypotension; bradycardia; distended abdomen (paralytic ileus), a non-optimal neurological state: Glasgow Coma Scale (ECG) at admission of 12 points, which then decreased to 7 points, which made necessary the need for endotracheal intubation and ventilatory support due to hypoxemia and hypercapnia.
Reinhardt and Mann reported hypoxemia in 80%, hypercapnia in 54%, and hypothermia with a temperature lower than 34.5 ° C in 88% of all patients with myxedema crisis14.
Likewise, sinus bradycardia, low voltage complexes, branch block, complete heart block, and nonspecific ST changes in the electrocardiogram were recorded in the myxedema crisis10. Our patient presented sinus bradycardia with a prolonged QT.
An important practical aspect may be the identification of pericardial effusion and myocardial infarction in a myxedema crisis scenario. Low-voltage complexes and nonspecific ST changes can be seen in pericardial effusion. Cardiac enzymes should be performed in case of suspected infarction11. Bilateral pleural effusion plus non-pericardial effusion was found, and there was a suspicion of cardiac infarction, so troponin was requested, which was negative. In a second moment, sinus node dysfunction was proposed, which after evaluation by cardiology discarded it and considered of metabolic origin.
Elevated TSH and very low serum concentrations of T4, FT4, and T3 confirm the diagnosis of myxedema Coma. Other laboratory findings include anemia, hyponatremia, hypercholesterolemia, elevated serum lactate dehydrogenase, high CPK concentrations. Arterial blood gases can reveal hypoxemia, hypercapnia, and acidosis12. Each of these mentioned results was presented by our patient; in relation to the thyroid profile it is important to emphasize that in our emergency we do not count as a routine test and to do it we must have the authorization of an endocrinologist or the clinical pathologist in charge of the laboratory and the results are issued on the third day of the sample taken.
Patients with myxedema coma should be managed in an intensive care unit, under continuous monitoring, special attention should be given to ventilatory support in these patients, and mechanical ventilation should be given if required. Hypothermia and hypotension should be corrected. Metabolic disturbances such as hyponatremia, hypoglycemia, and hypercalcemia, which can aggravate the altered mental state, should be corrected. It should be investigated for all precipitating factors of myxedema coma. Likewise, cultures should be extracted, and chest x-rays are taken to rule out infections, if they are present, they should be treated aggressively with an appropriate antibiotic treatment12. Our patient was admitted to the Shock Trauma Unit from where he was referred to the area of EICU (Emergency Intermediate Care Unit) where he received invasive ventilatory support and support of relevant active vasoactive drugs. We could not corroborate an infectious factor of myxedema Coma infection: negative urine culture, negative chest tomography for pneumonia, no evidence of skin lesions. A disease with an abdominal starting point was considered due to the significant dilatation of thick intestinal loops with pneumatosis and free perihepatic fluid.
The practical use of glucocorticoids should be part of the initial therapeutic protocol, which indicates that severe hypothyroidism induces a lower adrenal response to stress, regardless of whether or not there is simultaneous adrenal insufficiency. Since the thyroid hormone accelerates the metabolism of cortisol, glucocorticoids should always be administered before thyroid replacement, as otherwise, it could precipitate an adrenal crisis. Hydrocortisone will be administered in a dose of stress, 50-100 mg intravenously (IV) every 6-8 h, for 7 to 10 days or until the patient is hemodynamically stabilized3. Our patient received hydrocortisone 100 mg e/8 hours.
High doses of levothyroxine (LT4) should be given to replace the deficit and saturate the circulating thyroid hormone deposits. The ATA (American Thyroid Association) recommends starting with 200-400 μg in bolus EV in the first 48 hours, followed by a more physiological dose of 50-100 μg EV daily until it can be administered orally. Although some propose to start with dosages higher than 300-500 μg, it would be prudent to avoid them in the elderly, malnourished, or with arrhythmias or myocardial infarction. To prevent the risk of cardiac complications, perform continuous cardiac monitoring, with a reduction of the thyroid hormone dose, if ischemic changes or arrhythmias are observed3. Switching to the oral route is possible when patient conditions have improved12. In the case under discussion, levothyroxine 300 ug was administered by nasogastric tube for two days and then 100 ug per day (since our institution does not have the presentation of levothyroxine in an ampoule and Peru it is not in the national essential medication request.of MINSA-2015). Its administration was developed followed by strict cardiological monitoring, due to the risks of arrhythmia or infarction that this administration can cause, although our patient did not present at the time acute coronary ischemic pathology or arrhythmia
Certainly, the myxedema coma brings with it gastrointestinal alterations: as ileus and intestinal wall edema, since there is no other alternative, it was decided to administer it through the digestive tract because there is no presentation in ampoules for intravenous administration. Some reviews conclude that oral absorption of L-T4 is variable, but the clinical response occurs rapidly even in myxedema ileus15.
Certainly, the myxedema coma brings with it gastrointestinal alterations: as ileus and intestinal wall edema, since there is no other alternative, it was decided to administer it through the digestive tract because there is no presentation in ampoules for intravenous administration. Some reviews conclude that oral absorption of L-T4 is variable, but the clinical response occurs rapidly even in myxedema ileus8,16.
The etiology of hypothyroidism (primary vs. secondary) and the route of administration of L-T4 (oral versus intravenous) did not influence the results of myxedema coma10.
Most sources, due to this, recommend EV treatment or oral levothyroxine, since the evidence does not seem to indicate a significant difference between the two13.
Most sources, due to this, recommend EV treatment or oral levothyroxine, since the evidence does not seem to indicate a significant difference between the two.
In the presented case, the highlight of all is that the patient presented all the clinical characteristics and laboratory findings "typical" of a decompensated hypothyroid patient, as mentioned in all the literature reviews. Nevertheless, what must be emphasized is the fact that, being a disease very infrequently, it is hardly posed at the beginning. Unless the evaluating physician has seen a similar case before; this will become more difficult if the patient does not have a history of thyroid disease and if the anamnesis is not the most appropriate, although it should be added that the previous symptomatology can be very erratic and not orientate to any specific pathology. Another problem to consider is the fact that thyroid profile laboratory tests are not performed routinely and that the results are usually issued two to three days later. On the other hand, not having the drug in presentation for parenteral administration could be harmful, although some publications report that there is no more significant difference with enteral administration despite the digestive alterations that may exist in this pathology.
Acknowledgment
We thank the Institute of Health Technology and Research Evaluation (IETSI) of EsSalud for the support for the development of this manuscript through its Mentoring Program.
Authorship Contributions: FRC, RHP and RAG have participated in the conception and design of the article and approval of the final version of the manuscript. FRC prepared the first draft of the article. FRC, RHP and RAG have performed data collection and critical content review.
Financing: Self-financed.
Interest conflict: At the time of conception of the publication of the article the authors worked in EsSalud.
Received: April 23, 2019.
Approved: May 13, 2019.
Correspondence: Fanny Elizabeth Ramírez Calderón.
Address: Servicio de Emergencias Hospital Rebagliati Seguro Social, EsSalud. Domingo Cueto N°120, Jesús María. Lima, Perú.
Telephone: +1945460084
E-mail: racaelifa@hotmail.com
