ARTÍCULO ORIGINAL
DOI 10.25176/RFMH.v19i3.2160
1 Skin clinic, Lima-Peru.
2 Peruvian Institute of Cellular Engineering and Tissue Manufacturing - INGECEL, Lima-Peru.
3 Research Institute in Biomedical Sciences INICIB - URP, Lima-Peru.
a Medical Director.
b Plastic surgeon.
c Surgeon doctor.
ABSTRACT
Introduction: The treatment with carbon dioxide (CO2) laser fractionated in high skin phototypes, can result in pigmentation disorders, persistent erythema, edema, appearance of acne outbreak, among others. Due to this, it is necessary to apply complementary techniques that minimize these adverse effects. Objetive: To identify the safety, efficacy and satisfactory synergistic effects after the application of platelet-rich plasma (PRP) after application of fractionated CO2 laser in the face with high phototypes, in order to diminish the adverse effects. Methods: Clinical experimental study - open clinical trial - randomized with a universe of 32 hemies with phototypes IV and V of Fitzpatrick. A fractionated CO2 (CO2RE-Syneron Candela) laser was used and immediately autologous PRP was applied in the case hemifields. In controls, betamethasone and petrolatum. The photographic results were compared by showing them to 3 expert doctors without previous information so that they could determine the short, medium and long term findings in a simple scale. This was done at the skin clinic between July 2017 and September 2018 in Lima - Peru. Results: In the short term, satisfactory results were observed in the hemies treated with PRP. There was a decrease in the presence of post-inflammatory hyperpigmentation, erythema, edema and the appearance of acne, as well as an increase in the effect of facial tightening, attenuation of naso-genital grooves and expression lines in the hemias treated with PRP. However, in the long term, these last improvements are not significant in relation to the other control midfaces. Discussion: The fractionated CO2 laser generates histopathological changes similar to the wounds, so that the PRP absorbed at transepidermic level accelerates healing and reduces the possibility of side effects. Important results are seen in the prevention of dyschromias in these phototypes. Laser therapy combined with PRP is associated with greater satisfaction with laser monotherapy. The expected results are in early stages of recovery, while in the long term, there are no significant differences between the two midfaces. Conclusion: These results, in our population of high phototype, suggest that the immediate use of PRP post laser fractionated CO2 is an effective method to improve rehabilitation and healing, reducing the patient's downtime and decreasing the risks of adverse effects - secondary, It should be considered as an effective therapeutic alternative as post laser treatment. The small series of cases presented, leaves open the door to work with greater population and it would be very useful to be able to contrast the results obtained with those of future authors.
Key words: Fractionated CO2 laser; Platelet rich plasma; Complications; Side effects; High phototypes. (source: MeSH NLM
RESUMEN
Introducción: El tratamiento con láser de Dióxido de Carbono (CO2) fraccionado en fototipos altos de piel, puede traer como consecuencia trastornos de pigmentación, eritema persistente, edema, aparición de brote de acné, entre otras. Debido a ello, se hace necesario aplicar técnicas complementarias que minimicen estos efectos adversos. Objectivo: Identificar la seguridad, eficacia y efectos sinérgicos satisfactorios de la aplicación de plasma rico en plaquetas (PRP) después de la aplicación de láser de CO2 fraccionado en la cara con fototipos altos, para disminuir los efectos adversos. Métodos: Estudio clínico experimental - ensayo clínico abierto – randomizado con un universo de 32 hemicaras con fototipos IV y V de Fitzpatrick. Se utilizó un láser de CO2 (CO2RE-Syneron Candela) fraccionado e inmediatamente se incluyó PRP autólogo ramdomizado en las hemicaras de casos. En los controles, betametasona y vaselina. Se compararon los resultados fotográficos mostrándolos a 3 médicos expertos sin información previa para que determinen en una escala sencilla los hallazgos a corto, mediano y largo plazo. Este se realizó en la clínica de la piel entre Julio del 2017 y Septiembre del 2018 en Lima – Perú. Resultados: A corto plazo se observó resultados satisfactorios en las hemicaras tratadas con PRP. Hubo una disminución en la presencia de hiperpigmentación pos inflamatoria, Eritema, edema y aparición de acné, así como un aumento en el efecto de tensado facial, atenuación de surcos naso genianos y líneas de expresión en las hemicaras tratadas con PRP. Sin embargo a largo plazo, estas últimas mejoras no son significativas en relación a la otra hemicara control. Discusión: El láser de CO2 fraccionado genera cambios histopatológicos similares a las heridas, por lo que el PRP absorbido a nivel transepidermico acelera la curación y reduce la posibilidad de aparición de efectos secundarios. Se aprecian resultados importantes en la prevención de discromías en estos fototipos. La terapia láser combinada con PRP se asocia con una mayor satisfacción frente a la monoterapia con láser. Los resultados esperados, se encuentran en etapas tempranas de recuperación, mientras que a largo plazo, no hay diferencias significativas entre ambas hemicaras. Conclusión: Estos resultados, en nuestra población de fototipo alto, sugieren que el uso inmediato del PRP post laser Co2 fraccionado, es un método eficaz para mejorar la rehabilitación y cicatrización, reduciendo el tiempo de inactividad del paciente y disminuyendo los riesgos de efectos adversos – secundarios, debiéndose considerar como una alternativa terapéutica eficaz como tratamiento post laser. La serie pequeña de casos presentada, deja abierta la puerta a trabajos con mayor población y seria de mucha utilidad poder contrastar los resultados obtenidos con los de futuros autores.
Palabras clave: Láser CO2 fraccionado; Plasma rico en plaquetas; PRP; Complicaciones; Efectos secundarios; Fototipos altos. (fuente: DeCS BIREME)
INTRODUCTION
Skin aging is a biological process complex that is characterized by the appearance of: Ritidosis, atrophy, thickening, pigmentation, spots and laxity. All caused by factors intrinsic and extrinsic, including inheritance genetics, the photo aging acquired by the exposure or acquired pathologies such as sequels of acne1.
Non-surgical facial rejuvenation, corresponds to one of the most requested treatments to improve these imperfections2. There are several techniques to treat facial rejuvenation (Table 1), between we have the lights and more specifically ablative laser systems, known since some years. But all "non-surgical" technique also It has its limitations due to its side effects and complications, appearing more frequently when applied in high phototypes (contraindicated in many cases).
The introduction of fractional application systems has allowed access to treat facial rejuvenation with fewer side effects and complications, especially in patients with high skin phototype. Yet thus, the risk of their occurrence persists, although to a lesser extent.

The rejuvenation, refresh or facial resurfacing with light systems, is based on the capacity of regeneration of the skin by controlled damage on the cutaneous surface generated by the systems ablatives, as it happens with mechanical systems and chemicals. In fact, facial rejuvenation with fractional CO2 laser seems to be currently one of the most valuable treatments for imperfections facial2. In the case of fractionated CO2 laser, We are starting a controlled process of damage tissue to stimulate the repair and renewal of skin. This leads to limitations due to its effects adverse events (including sick leave, which will be variable, according to the treatment conditions).
The fractionated carbon dioxide (CO2) aser is considered a conservative, safe treatment, precise and effective for facial rejuvenation and skin imperfections3. These energies are used in anti-aging due to its characteristics minimum invasion, simple operation, high tolerance and favorable effect4. Fractional rejuvenation causes a minimal disruption of the epidermis and generates macro columns of coagulated tissue that they extend deep into the dermis3, causing the hardening of the tissues and the remodeling of the collagen from the start until about 3 to 6 months later of the treatment5.
Under the mechanism of selective photothermolysis, the fractionated CO2 laser acts promoting the production of fibroblasts, synthesis, regeneration and change of connective tissue reorganizing the collagen fibers. As a result, tissue recovery improves accelerating the skin's metabolism directly by vaporizing the pigment or cells that contain it, improving slight to moderate wrinkles, texture and skin color, open pores and flaccidity4. It is therefore has been considered as the Gold standard for the non-surgical facial rejuvenation treatment6. But, even the responsible use of this energy in expert hands, can produce prolonged erythema, can last up to six weeks with risk of hyper and / or permanent hypo pigmentation accompanied in occasions of hypertrophic scarring7. In those skin phototype patients high, adverse effects mentioned extend the recovery time greatly affecting his personal life, family and work, since the increase in melanin increases the inflammatory effects8.
Previous studies on the use of PRP together with the Fractionated CO2 Laser, show an improvement statistically significant in the presence of erythema and less post-inflammatory hyperpigmentation in the treatment sites one with a higher production of collagen with respect to the controls. All these changes are probably due to the presence of at least seven different factors of growth in the PRP that can improve soft tissue repair9. The treatment of high phototypes with systems ablatives is a challenge, so it was agreed to introduce split systems, for their greater efficiency, but with more adverse effects that should be controlled10 .
Because of that, we sought to apply techniques complementary activities that will diminish these effects secondary and complications. Among the techniques of complementary types used are pharmacological, physical or biological as are the creams regenerating, depigmentation, sunscreen, laser or light at low power density (LLLT), factors of growth, among others, and more recently the PRP11. All of them have helped to diminish the effects adverse effects mentioned with an improvement in the result end of treatment. The PRP has become today very popular day in the field of plastic surgery and dermatology for the restoration of injuries12.
Consequently, the present study has as objective to contrast and assess safety, efficacy and the satisfactory synergistic effects in short, medium and long term after the application of the PRP after application of fractionated CO2 laser in the face, due to its known properties of tissue regeneration with the intention of diminishing the adverse effects like initial erythema, post-inflammatory pigmentation, edema, appearance of Acne, as well as work downtime.
METHODS
An experimental clinical study was conducted – trial open clinical - randomized with a universe of 32 hemi faces from 16 patients, 10 women and 6 men, with photo types IV and V of Fitzpatrick, (see graph No. 1) with an average age of 41.7 years with mixed skin each face was divided into hemi faces, a side was assigned for the case and the other side for control per patient, all of them accepted the consent informed by the ethics committee of the institutions involved.

A fractional CO2 laser was used in all patients (CO2RE-Syneron Candela) by established parameters - (Table 2) and were prepared the faces previously with 70% Alcohol, anesthetic topical EMLA (Lidocaine 25mg / g and Prilocaine 25mg / g) immediately after the autologous PRP was applied topical form (sprayed) in the corresponding hemi fields to the cases and in the control hemi faces, cream was applied topical of Betamethasone 0.5mg and Vaseline.
The open clinical trial consisted of showing 3 expert doctors, without prior information, records photographic works with the same intensity of light and background, to determine, on a simple scale, the short, medium and long term findings. For this, I use a data collection card and a camera camera Canon EOS Rebel T3, EFS lens 18-55 mm, 12 megapixels, with a resolution of 4272 x 2848. This data record was made in the "skin clinic" between July 2017 and September 2018.
• Obtaining process and isolation of PRP.
For the taking of blood we use sterile syringes disposable of different volumes and sterile tubes of vacuum of 3.5 cc, mixed with 3.2% sodium citrate, as an anticoagulant. Once the samples have been obtained we proceeded to its centrifugation using centrifuge LABOFUGE 200, from Thermo Cientific, german brand, Calibrated and programmed at 1600 RPM for 8 minutes. After centrifugation, the PRP content is extracted in the autologous serum, to proceed to the activation of the platelets in order to help the release of growth factors, 10 ml ampoules were used of 10% calcium gluconate. After this process and after the application of the fractionated CO2 laser in the patient's face, we proceed to spray the autologous serum already activated, massaging gently to favor the distribution and absorption of serum in the skin.
• Fractional CO2 laser session
After the preparation, wait for 30 minutes, and proceed to clean the anesthetic with distilled water. The parameters used in the equipment were (Table 2):

The shooting pattern applied on all faces was hexagonal, following the voltage vectors, completing with an Overlap of around 20-30%. (Figure N ° 1).

We divide the treated units by issues academics in:
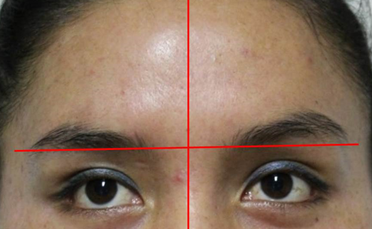
o Group 1: Patients who received fractionated laser and the PRP is applied topically in a hemi-face randomly chosen (Figure No. 2 A, A1).

o Group 2: Patients who received fractionated laser and usual treatment. (Figure N ° 3 A, B)

Both groups were given the indications for the use of photo protection, and you are told that for questions of study will be taken photographic record on days 0, 1, 2, 3, 4, 5, 6, 7, 15, 30 and 90 after the procedure.(Figure N ° 4)

For the evaluation of the results, we showed the iconography to 3 doctors with experience in different laser wavelengths (fractionated CO2, erbium yag, pulsed dye, alexandrite, q-switched NdYag, KTP, etc.) who did not know the areas of application of PRP / usual treatment, writing his findings in a form simple for each case-patient of appreciations and these were contrasted.
RESULTS
Divided Sixteen face-study patients were considered, considering that there were 3 doctors the evaluators, for which a total of 48 surveys in the study. In 46 surveys, considered that there was a significant difference among the treated hemi-faces, 45 of them were correctly, and only 1 was wrong about the hemi-face to which the PRP is additionally applied. The remaining 2 polls saw no differences between both hemif-faces.
Regarding the favorable evolution in the laser hemi-face CO2 and PRP with respect to the one that did not receive PRP (Table N ° 3).
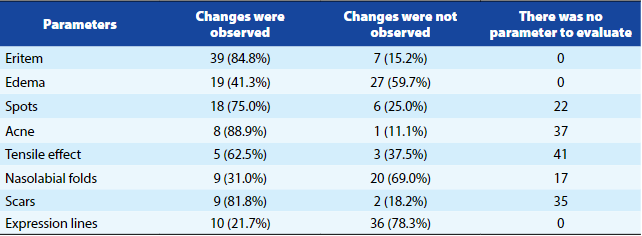
• REDNESS
Regarding erythema, 39 (84.78%) showed change in the side corresponding to the PRP becoming more evident in the first 4 days after treatment, compared to 7 (15.22%) that they did not show it. It did not influence the skin phototype, the sex, or the type of skin. (Figure N ° 5).

• EDEMA
Regarding the edema, 19 (41.30%) noticed difference in the hemi-face corresponding to the PRP and 27 (58.70%) did not they noticed. It did not influence the sex, the skin phototype, or the type of skin (Figure N ° 6).

• STAINS
Regarding stains or dyschromias, 18 (75%) of the cases show improvement on the side corresponding to the topical PRP application, while 6 (25%) not. Being the most obvious results from the third week of treatment. Here if a relationship between the higher skin phototype, with the highest possibility of pigmentation. The same as the relatively frequent greater in women in relation to men. The type of skin It was not decisive. (Figure N ° 7).

• ACNE
Regarding acne, in 8 (88.9%) of the cases presented the difference is evident, while in 1 (11.1%) not. Patients with mixed skin were more predisposed to the appearance, also coincides with the areas where the cream with Vaseline and betamethasone. Does not influence the phototype or sex. (Figures N ° 8).

• TENSOR EFFECT
Regarding the tensor effect, 5 (62.5%) of the cases in the that was evident was manifested on the side that received PRP while 3 (37.5%) does not. (Figure N ° 9)
• NASOGENIAN WINCKLES
Regarding the naso-genian furrows, 9 (31%) show favorable changes on the side where PRP is applied, while that 20 (69%) does not. (Figure N ° 10). It is not dependent on phototype, type of skin or sex.

• SCARS
Regarding scars (sequelae of acne or chicken pox), it was positive the improvement on the side where there was scars were applied PRP 9 (81.8%) compared to 2 (18.2%) that did not, however, it was not dependent on skin phototype, sex, or type of complexion. The measurement is made after 90 days that tissue recovery and changes in injuries deep, take longer. However, the number of cases where there were scars to evaluate was not significant.
• EXPRESSION LINES
Regarding the lines of expression, although at the beginning there could be a slight difference, after 30 days of treatment, the comparable changes were much minors, appreciating in 10 (21.7%) the difference while in 36 (78.3%) not in the first week of evolution. And practically undifferentiated at 30 days. The changes are not dependent on sex either, phototype, or skin type.
DISCUSSION
The application of fractionated CO2 laser in the skin facilitates transepidermal penetration of the PRP through of the micro channels left by the laser in the tissue4. It has been proven in other studies, with staining of Hematoxylin and eosin biopsy of treated sites with fractional CO2 laser and PRP at day 28, epidermis thicker with a stratum corneum better organized and better quality of collagen fiber bundles7.
The process of wound healing depends mainly from the formation of new vessels blood The fractionated CO2 laser generates histopathological changes similar to those of the wounds, so the PRP absorbed at epidermal trans level accelerates healing and reduces the possibility of effects secondary11. Coinciding with other authors, it was not observed persistent adverse effects during the study (Hyper / hypo pigmentation or scarring hypertrophic or permanent stains).
In the scars areas of acne or chicken pox, improvement is seen where PRP is applied. This could be attribute to the synergistic effect of both modalities through various mechanisms, such as the release of the alpha granules that contain numerous Growth factors such as PDGF, TGF, or Vascular endothelial growth factors, growth factor insulin, fibroblastic growth factor, of epithelial growth factor, and growth factor of keratinocytes7,11. No other effects found side effects such as petechiae, pigmentation, effusion, infection, appearance of aberrant scar, blisters and contact dermatitis after treatment, coinciding with related studies4. Prevention of facial pigmentation persists with time.
An additional finding was the sense of relief immediately after the topical application of PRP, in relation to the hemi-face where cream was applied. While the combination therapy of fractionated CO2 laser and autologous topical PRP, were successful in the first days regarding the improvement of facial tightening, last this time, the differences between both hemi-faces was minimal. The same thing happened with the lines of expression and the results of facial rejuvenation type.
Consequently, having an evident difference in patients receiving autologous PRP immediately after the laser, in relation to thethat only receive lasers; and considering that the erythema and edema, as well as the fall of scabs, occurs in minor time, it follows that there is a decrease in the downtime required by the patient.
Important results are seen in the prevention of the steins or dyschromias in skin high phototypes, most likely due to the shortening of the inflammatory process in the skin.
At the same time, laser therapy combined with PRP is associated with greater patient satisfaction with the treatment and with a significant satisfaction greater with the appearance of pigmentation after treatment versus laser monotherapy. The hemi-faces where topical autologous PRP was placed fractionated CO2 laser, they had a recovery faster, less possibility and duration of effects adverse to the hemie-faces where PRP was not placed.
The improvements were evidenced mainly in the erythema and edema, which were significantly reduced in the days after the application of the laser and PRP. In relation to the tension of the skin, the attenuation of the naso-genian winckles, and the scar sequels, there is not significant result to medium and long term, not having as a consequence a justification for its use for these purposes.
CONCLUSION
In general, our findings suggest that autologous PRP application topically, later to the application of fractional CO2 laser, is a method effective to improve rehabilitation, healing and reduction of adverse and secondary effects such as erythema, edema, spots and acne outbreak, reducing the patient's downtime and decreasing the risks that patients sometimes choose for not doing the fractionated laser procedure.
he use of PRP post laser fractional CO2, is a safe and effective tool that does not have effects secondary because it is an autologous component, atoxic and natural, in addition to being a procedure highly reproducible. That is why it is necessary studies with greater population and other weapons of measurement to place the PRP and its derivatives within of the usual therapeutic arsenal in this type of disciplines.
THANKS
The authors thank the Instituto Peruano de Ingeniería Celular y Manufactura Tisular A.C. – INGECEL - and the INICIB, Instituto de Investigación en Ciencias Biomédicas of the Universidad Ricardo Palma, both in Lima, Perú, for good development and the support.
Authorship Contributions: The authors participated in the genesis of the idea, project design, data collection and interpretation, analysis of results, preparation of the manuscript of this research paper.
Financing: Self-financed.
Interest conflict:The authors declare no conflict of interest in the publication of this article.
Received: May 10, 2019.
Approved: June 10, 2019.
Correspondence: Edmundo Saco Mera
Address: Jirón Monterrey 341, Santiago de Surco 15038
Telephone: +51 934 459 843
E-mail: edmundosm@yahoo.com
