ORIGINAL ARTICLE
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2019 - Universidad Ricardo PalmaDOI 10.25176/RFMH.v19i4.2344
PROGNOSTIC FACTORS ASSOCIATED WITH BAD EVOLUTION IN PATIENT OPERATED HIP FRACTURE OVER 65 YEARS OLD
FACTORES PRONOSTICOS ASOCIADOS A MALA EVOLUCION EN PACIENTES OPERADOS DE FRACTURA DE CADERA MAYORES DE 65 AÑOS
Renee Flor Vento Benel1,a
Jhony A. De la Cruz-Vargas2,b
Cecilia Salinas Salas1,e
1 1. Institute of Research in Biomedical Sciences (INICIB) Lima, Peru.
2 2. Director-General of INICIB, Ricardo Palma University, Lima, Peru.
a Surgeon.
b Specialist in medical oncology.
c Master's degree in clinical research.
d Doctorate in medicine.
e Specialist in geriatrics.
>
ABSTRACT
Introduction: Hip fracture in the elderly is the most common cause of hospitalization in the trauma department, causing repercussion in several clinical areas, affecting its independence. Objective: To determine the prognostic factors of poor evolution in the study population. Methods: Ambispective, correlational and non-experimental study was designed. The population consisted of all patients over 65 years of age who underwent surgery for hip fracture between January 2014 and July 2015 at the Central Hospital of the Pruvian Air Force (F.A.P). The magnitude of the association was quantified using the odds ratio, and a multivariate analysis was performed on the significant variables and a 6-month follow-up was performed. Results: The variables identified with a strong association with poor evolution were: age greater than 75 years (OR = 3,750 CI: 1,275-11,026 p = 0,016), high comorbidity (OR = 4.00 CI: 1.58 -10.08 p = 0.003), hemoglobin <10 (OR 6,545 CI: 1.17-36.6 p = 0.0032), respiratory complication (OR 6.00 CI: 1.55-22.94 p = 0.000) patients in the 6-month follow-up. The previous fracture was strongly related to mortality (OR 3,665 CI: 1,366 - 9,821 p = 0,010). Conclusion: The poor evolution in hip fracture is associated with high comorbidity, age greater than 75 years, residence (institutionalized patient), postoperative respiratory complication with significant limitations in gait capacity and the functional status of the patients. Finally, the antecedent previous fracture showed high association with an increased mortality of patients at 6 months follow-up
Key Words: hip fracture, prognostic factors (MeSH/NLM)
RESUMEN
Introducción: La fractura de cadera en el adulto mayor es la causa más común de hospitalización en el servicio de traumatología, ocasionando repercusión en distintas áreas clínicas y afectando su independencia. Objetivo: Determinar los factores pronósticos de mala evolución, en la población de estudio. Métodos: Se diseñó un estudio ambispectivo, correlacional y no experimental. La población estuvo constituida por todos los pacientes mayores de 65 años intervenidos quirúrgicamente por fractura de cadera, entre enero de 2014 hasta julio 2015 del Hospital Central de la Fuerza Aérea del Perú (F.A.P). Se cuantificó la magnitud de la asociación utilizando el odds ratio, posteriormente se hizo un análisis multivariado para las variables significativas. Resultados: Las variables identificadas con un fuerte grado de asociación a mala evolución (grado funcional desfavorable) a los 6 meses de seguimiento fueron: edad mayor de 75 años (OR= 3,750 IC: 1,275-11.026 p= 0,016), alta comorbilidad (OR= 4,00 IC: 1,58-10.08 p= 0,003), hemoglobina <10 (OR 6,545 IC: 1,17-36.6 p= 0,0032), complicación respiratoria (OR 6,00 IC: 1,55-22.94 p= 0,000). La fractura previa mostro ser factor pronostico asociado a mortalidad (OR 3,665 IC: 1,366- 9.821 p= 0,010). Conclusión: La mala evolución en fractura de cadera está asociada a una elevada comorbilidad, edad mayor de 75 años, residencia, complicación respiratoria postoperatoria con importantes limitaciones en la capacidad de la marcha y el estado funcional de los pacientes. Finalmente, el antecedente de fractura previa mostró alta asociación a mayor mortalidad de los pacientes a los 6 meses de seguimiento
Palabras Clave: Fractura de cadera, factores pronósticos (Decs/Bireme)
Hip fracture is a prevalent entity in the elderly age group, and is one of the most frequent causes of hospital admission in people over 65 years of age; because the population of older adults has been growing in recent decades, this pathology has acquired great importance. About 1.5 million hip fractures occur each year.1. The World Health Organization has estimated that by 2050, a total of 6 million hip fractures will occur worldwide per year, and in the European Community, it will be more than 1 million fractures2. In the United States, the total number of hip fractures in people aged 50 and older will increase from 238,000 to 512,000 by 2040, with a concomitant increase in avoidable deaths, disability, and medical costs3.
In Peru and Latin America, there are no exact figures related to this pathology. However, it is estimated that by 2050, this type of injury will increase worldwide and 70% will correspond to Latin America4 and in Peru, EsSalud (the national health insurance provider for public workers) estimates that 12-16% of Peruvian women over 50 will suffer a hip fracture per year. Population statistics project that there will be 7.5 million Peruvian women aged 50 or over in 20505. Therefore, more than 500,000 hip fractures could be expected in 2050, so some authors have called it the silent epidemic in Peru6.
In-hospital mortality oscillates between 4 and 8%, and it is considered that around 40-50% of patients regain functionality before the fracture, although only 30% will become independent again for the activities of daily living7. In studies carried out in the USA, it was found that close to 30% of patients operated for a hip fracture will die8. Hip fracture alone is capable of decreasing life expectancy by almost two years, and one in five patients who suffer from it will require permanent socio-sanitary assistance9.
It has been described multiple factors that influence perioperative morbidity and mortality: some of the patient's own factors (age, sex, lack of autonomy, comorbidity, dementia, polypharmacy, anaemia, type of fracture, place of residence or geriatric asylum, etc.)10, other intrahospital factors (surgical delay, type of surgery, anaesthetic treatment, start of wandering and rehabilitation, etc.)11 and others related to the patient's discharge (rehabilitation, support, fall prevention, osteoporosis treatment, etc.)12.
It is necessary to optimize the state of health before surgery, prevent complications, and offer the most appropriate hospital treatment throughout the process to reduce hospital stay and postoperative morbidity and mortality11.
For all these reasons, hip fracture is a problem of great importance both for the area of care and for proper hospital management.
The main objective of this study was to determine the prognostic factors associated with weak evolution (unfavorable functional grade) in patients over 65 years of age with hip fracture and to identify the prognostic factors associated with postoperative mortality six months after surgery.
Methods
A study was carried out of an ambispective, correlational, non-experimental type, with a census sampling, where 99 patients over 65 years of age underwent surgery for hip fracture, between January 2014 and July 2015, at the Central Hospital of the Peruvian Air Force. Patients diagnosed with pathological fracture and those who were not subject to surgical treatment were excluded.
Hospital records of the Trauma and Orthopaedic Service were consulted for population identification. The sociodemographic, biological, clinical, and therapeutic information was obtained from the files in the clinical history.
Patients were monitored six months after discharge from the hospital, through outpatient care and home visits by geriatrics. The study variables were grouped into sociodemographic, biological, clinical, fracture and treatment data, postoperative complications, and presence of blood transfusions. Besides, functional and mortality parameters were evaluated six months after surgery.
Comorbidity was evaluated using the Charlson index (CI) (categorized for our study as low comorbidity = 2 points and high comorbidity > = 3 points)1.1For preoperative anemia, transfusion was indicated in patients with hemoglobin values of less than 8 g/dL; and in patients with cardiorespiratory disease and/or hemodynamic instability if hemoglobin values were 10 g/dL, according to the restrictive transfusion criteria set by the institution's Committee on Haemotherapy. In order to assess the functional status, the functional degree of the Red Cross was recorded2, according to the revised literature is broken down to functional grade 0.1 and 2 as favorable; and 3.4.5 as unfavorable 13.
In addition to the identification of prognostic factors associated with postoperative mortality and morbidity, baseline measure of functional status was performed, and also after surgery, at 6 months. Finally, survival and mortality rates were evaluated.
The Institutional Ethics Committee approved the study, and the Protocol was registered at the Faculty of Medicine of the University Ricardo Palma28 and approved by the Hospital Directorate of the Peruvian Air Forces.
Statistical analysis
There were elaborated frequency tables for qualitative variables, and, for continuous variables, there were obtained the mean and standard deviation.
Using Pearson's Chi-Square Test was performed the bivariate analysis for categorical variables. The multivariate analysis was performed using the logistic regression model. The outcome variables were baseline functional status and functional status six months after surgery, as well as mortality. The variables that were statistically significant in the bivariate analysis entered a multivariate analysis to obtain independent variables. There were calculated the odds ratios and their confidence intervals at 95%. It is considered, for all results, a significance of p <0.05. Survival analysis was performed using the Kaplan-Meier method. Comparison of survival curves was performed using the log-rank test.
It was used the statistical package SPSS for Windows v.23.0 for statistical analysis.
Results
Of the 99 patients included, it was found the mean age of 83.51 +- 9.2 years (65 - 103). 64.6% were women. 100% of the patients were classified as ASA II-III. table 1 describes the general characteristics of the study population, considering as "institutionalized" those patients residing in asylums and shelters, and as "non-institutionalized" those living in a private home.
| Variable | N = 99 |
| Age | 83.51 +- 9,2 |
| Sex | |
| Female | 64(64,6%) |
| Male | 35(35,4%) |
| Home | |
| Institutionalized with Company | 14 (14,1%) |
| Institutionalized without Company | 32 (32,3%) |
| Not institutionalized with Company | 32 (32,3%) |
| Not institutionalized without Company | 21 (21,3%) |
| ASA | |
| I | 0 |
| II | 65 (65.7%) |
| III | 34 (34,3%) |
| IV | 0 |
| Charlson comorbidity index | |
| Absence of comorbidity (0-1) | 3 (3%) |
| Low comorbidity (2) | 43 (43,4%) |
| High comorbidity (3 or more) | 53 (53,5%) |
| Hemoglobin on admission | 10.1 +- 1,9 |
| Hb < 10 gr/dl | 57(57,6%) |
| Hb > 10 gr/dl | 36(36,4%) |
| Surgery delay time | |
| >2 days | 78 (78,8%) |
| <2 days | 42 (42,4%) |
| Surgical technique | |
| Total prosthesis | 20 (20,2%) |
| Partial prothesis | 17 (17,2%) |
| DHS board | 22 (22,2%) |
| Endomedular nail | 29 (29,3%) |
| Others | 11 (11,1%) |
| Blood transfusion | |
| Yes | 45 (45,5%) |
| No | 54 (54,4 %) |
| Operating Time | |
| < 45 minutes | 28 (28,3%) |
| >45 minutes | 71 (71,7 %) |
In the postoperative period, the presence of some complications was high, with cognitive complications being the most frequent, followed by renal disorders, cardiovascular complications, respiratory complications, and infections, taking into account that a patient may have more than one difficulty (table 2). During hospitalization, 45.5% of patients received a blood transfusion. Overall mortality was 22.5%; in-hospital mortality was 4.05%; at three months, it was 11.12%, and, at six months follow-up, it was 7.08%. The basal functional grade: 27 (27.3%) fend for themselves, 26 (26.3%) wander with some difficulty, 19 (19.2%) are independent with a cane, 11 (11.1%) walk with a walker or require little help from one person, 10 (10.1%) need help from two people or have habitual incontinence, while 6 (6.1%) do not walk, have total incontinence or nursing care. On the other hand, at 6 months, 5 (6.49%) are on their own, 16 (20.8%) wander with some difficulty, 15 (19.5%) are independent with a cane, 19 (24.68%) walk with a walker or require little help from one person, 13 (16.9%) need help from two people or have habitual incontinence, and 9 (11.7%) do not walk, have total incontinence or require nursing care.
| Variable | N = 99 |
| Cardiocirculatory | |
| Acute myocardial infarction | 3 (3,0%) |
| Arrhythmias | 12 (12,1%) |
| Acute Pulmonary Edema | 4 (4,0%) |
| PULSE | 5 (5,1%) |
| AVC | 1 (1,0 %) |
| Respiratory | 32 (32,3%) |
| Hypoxia | 4 (4,0%) |
| COPD decompensation | 18 (18,2%) |
| Respiratory superinfection | 4 (4,0%) |
| Other | 1 (1,0%) |
| Major bleeding | 15 (15,2%) |
| Renal | |
| Oligoanuria | 14 (14,1%) |
| Acute renal failure | 9 (9,1%) |
| Infections | |
| Wound | 1 (1,0%) |
| Urinary tract | 9 (9,1%) |
| Systemic | 7 (7,1%) |
| Cognitive disorders | |
| Disorientation | 16 (16,2%) |
| Agitation | 1 (1,0%) |
| Surgical reintervention | 7 (7,1%) |
| Other (minor complications) | 16 (16,2%) |
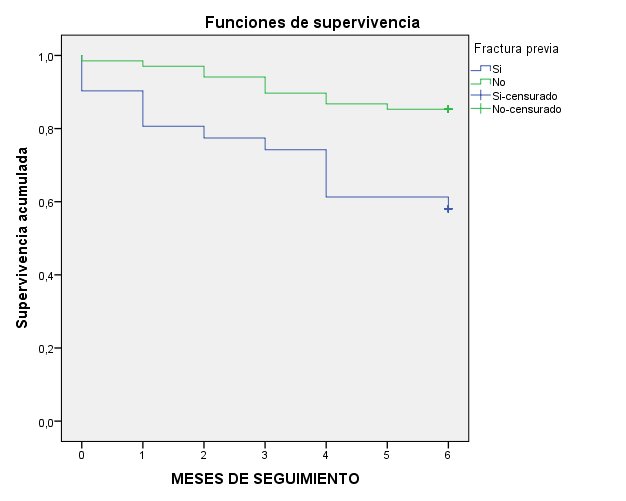
In the multivariate survival analysis, only the previous fracture variable maintained its association with mortality at six months. While age, hemoglobin less than 10, high comorbidity, and presence of respiratory complications were found associated with unfavorable functional grade. Survival was analyzed using the Kaplan-Meier curve with and without previous fracture (figure 1)
It could be observed that those patients who had a previous fracture had a higher mortality rate than those who did not have this antecedent.
It was then decided to analyze the previous fracture stratified by sex (Figure 2)
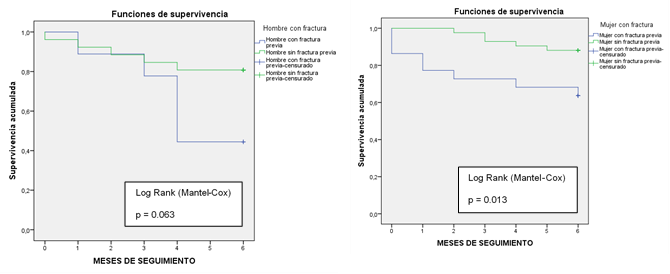
Figure 3. Survival in relation to previous fracture by sex was analyzed. (Figure 3 a and b).
3a Survival in men with and without previous fracture
3b Survival in women with and without fracture
In our work, the population group studied is made up of patients over 65 years of age, who are divided into two groups with a cut-off point of 75 years, so it is to be expected that, as indicated in the literature consulted, the risk of suffering a hip fracture from the fifth decade of life doubles every five years. Our population would be eight times more at risk14. The average age presented by the patients in the study was 83.5 years. This figure corresponds to that of the published series that include patients considered to be elderly15.
Concerning sex, we found that 64.6% were female, with a female/male ratio of 2:1. The incidence of hip fracture in our country is similar to that one of the other countries in the Mediterranean area and is below that those of Nordic countries. It is more frequent in the female sex than in the male sex, with a ratio that can be as high as 3 to 116.
When evaluating the favorable functional status (0.12), when comparing the basal (72.8%) with the one found at six months (46.73%), the reduction in the favorable functional grade was 40%, or, seen in another way, the recovery of the functional grade was 60%. When we included all patients and excluded the last two functional grades, we found that 83.9% had a baseline state in which they did not need help with all activities of daily living. However, at six months, those with this functional grade were 71.4%, which means that there was a recovery of 73.1%.
If each functional group is taken into account, it is observed that of 27 patients who were previously totally independent, after 6 months of the event, only 5 patients are able to recover total independence, in contrast to functional groups 3 and 4 (21 patients) that show an increase of 32 patients after 6 months of the fracture. Compared to Reguant16, study, of 86 patients who walk normally before the fracture, only 33 (38.4%) had regained their previous walking ability one year after surgery, 47 patients (54.6%) needed some form of walking aid, and six patients (7%) did not walk.
In terms of patient residence, being in an institution or asylum was found to be a risk factor (OR= 4.89, CI= 1.95 - 12.28, p= 0.001) for unfavorable functional status (3, 4, or 5 on the Red Cross scale), coinciding with literature17.
The previous state of health of the populations under study is a factor that will determine the evolution of a series of possible events after a hip fracture. In general, it is observed in other published studies that surgery could be delayed due to the poor clinical conditions of patients compared to those who underwent surgery before18. In our study population, we found that 3% of patients did not have any comorbidity. 43.7% had some comorbidity, and the remaining 53% had three or more comorbidities. We have found the existence of statistical association in the study population concerning the referred comorbidity (OR= 6.01, CI= 2.19 - 16.60, p= 0.000), coinciding with other published series16,17.
It was also found that, since the patient is institutionalized, he or she has a higher risk of bad evolution, which coincides with the study carried out by Homero et al.19, since this type of patient presents a higher risk of falls. Falls, in turn, are the leading cause of accidents in this age group. Although falls do not often have fatal consequences, they do affect people's health and quality of life20.
On the other hand, the results of this study show that the intervened population of hip fracture, in our hospital, during the year 2014, had similar characteristics to other published series 8,16,21. Our results show an intrahospital mortality of 4.05% and accumulated mortality at 3 and 6 months of 18.20%, figures lower than those published by other groups17,21,22.
We found no significant difference in mortality between patients operated on before or after 48 hours of admission. There is much controversy in the literature regarding the relationship between surgical delay time and postoperative mortality. Several authors support that early treatment is associated with a reduction in mortality in the short and medium-term. In the study conducted at the Hospital Cayetano Heredia, it was found that a surgical delay greater than 48 hours was associated with urinary complications and pneumonia6. However, in our study, we observed a higher number of complications with greater surgical delay, reaching significance only for respiratory complications. In the meta-analysis of Shiga et al.23, a surgical delay of more than 48 hours was associated with increased mortality in the short and medium-term in elderly patients with femoral fractures and early surgery with increased benefit in low-risk and younger patients. We associated surgical delay with mortality at six months, but, unlike Shiga et al.23, we found no association with surgical waiting time.
With respect to hemoglobin as a prognostic factor, our study shows a high association with respect to an unfavorable functional grade (OR: 5.26; p= 0.022 ; CI = 1.20 - 3.69) which coincides with other published series in which severe anemia is a factor associated with a decrease in independence and an increase in mortality; however, with respect to this last variable, our results disagree with studies carried out most probably due to the sample number24.
The prognostic factors related to postoperative mortality described in the literature are the following: advanced age, male sex, an ASA III and IV, having three or more comorbidities associated with admission, dementia, cardiocirculatory, and postoperative respiratory complications, and living in a residence or asylum25. Our data after bivariate analysis coincide with the literature regarding advanced age and having three or more associated comorbidities, but not concerning sex; however, when comparing patients with the previous fracture according to sex, there is higher survival in female patients (p = 0.013).
In the multivariate analysis model, only the previous fracture (p= 0.007) remained an independent prognostic factor of mortality. Unlike the study by Roche et al.25, we found no association between postoperative respiratory infections and mortality. Sex did not influence, perhaps because it was a limited sample.
The results obtained corroborate the high morbidity and mortality of the patients intervened for hip fracture, the important limitations in walking capacity, and the functional state of the patients six months after surgery. Regarding unfavorable functional grade, in the multivariate model, it was obtained that advanced age, low hemoglobin, high comorbidity, and respiratory complications are associated factors, which would constitute the profile of an elderly patient with a poor prognosis.
Recommendations
Prospective and more statistically powered studies are recommended to confirm the association of prognostic factors related to postoperative complications, causes of surgical delay, the impact of anemia and surgical delay, and transfusion rate; and to consider the time elapsed for initiation of rehabilitation and patient mobilization. Also, it is necessary to pay special attention to those elderly patients who have high comorbidities to avoid postoperative complications that lead to a decrease in the patient's functional grade, applying a risk stratification strategy according to our study. Finally, we recommend prior comprehensive geriatric evaluation of all older adult patients in order to implement a prior multidisciplinary plan of action, with particular attention to patients with hip fractures before, during, and after surgery, focusing on reducing complications and morbidity and mortality.
That is why knowing the forecasts on the evolution of hip fracture is an issue of great importance and goes beyond the health field.
Conclusion
The prognostic factors of poor evolution in hip fracture (unfavorable functional grade) at six months were: age, residence (institutionalized patient), high comorbidity (Charlson Comorbidity Index more than three comorbidities), and respiratory complication. Finally, the history of the previous fracture showed a high association with higher mortality of patients at six months of follow-up.
Financing: Self-financed
Conflict of Interest: The authors declare that they have no conflict of interest.
Correspondence: Renee Flor Vento Benel
Address: Avenida Benavides 5440, Surco. Lima, Perú.
Cell: 923453756
E-mail: ventobnel@hotmail.com
BIBLIOGRAPHIC REFERENCES