CLINICAL CASE
JOURNAL OF THE FACULTY OF HUMAN MEDICINE 2020 - Universidad Ricardo PalmaDOI 10.25176/RFMH.v20i2.2516
FOX - FORDYCE DISEASE, A CASE REPORT
PRURITO VULVAR Y ENFERMEDAD DE FOX – FORDYCE, UN REPORTE DE CASO
Katherine Luisa Contreras Gala1,a
1María Auxiliadora General Hospital, Lima-Peru
aResident Physician of Pathological Anatomy.
ABSTRACT
Fox-Fordyce disease is a non-infectious, infrequent inflammatory dermatosis of apocrine glands, isolated by a pruritic papular rash that usually begins frequently at puberty, and which may involve vulva, armpit and perianal region. It affects women more frequently, approximately in a 9 to 1 ratio, compared to men. In the presentation of the case of a female patient, 53 years old, in consultation of Gynecology-Obstetrics, of the General Maria Auxiliadora Hospital, for presenting for 5 months, papular eruption in vulvar area, associated with intermittent pruritus. A biopsy of the lesion was requested, and it was sent to the Pathological Anatomy Service, receiving a fragment of dark brown tissue, 0.3 x 0.2 x 0.1cm, which was automatically processed, obtaining a histological sheet, in which evidence dilated apocrine glands, which show a thick secretion made up of mucin, in its light. The patient met the histopathological criteria for the diagnosis of Fox - Fordyce disease. Consider the case presentation because of the infrequent nature of this disease.
Key words: Fox-Fordyce Disease, Pruritus Vulvae , Sweat Gland Diseases, Sweat glands (source: MeSH NLM).
RESUMEN
Se presenta un caso infrecuente de enfermedad de Fox-Fordyce en region vulvar, una dermatosis inflamatoria no infecciosa, infrecuente, de glándulas apocrinas, caracterizada por una erupción papular pruriginosa que involucra vulva, axila y región perianal, a predominio del sexo femenino, del cual no hay reportes nacionales. Se presenta una paciente de 53 años de edad, evaluada en consulta de Gineco-Obstetricia, por presentar desde hace 5 meses, erupción papular en zona vulvar, asociado a prurito intermitente. Se tomó una biopsia de la lesión, y se envió al Servicio de Anatomía Patológica, recibiéndose un fragmento de tejido de color pardo oscuro, de 0.3 x 0.2 x 0.1cm, en la cual se evidenció glándulas apocrinas dilatadas, con secreción espesa constituida por mucina, en su luz. Cumpliendo con los criterios histopatológicos se estableció el diagnóstico de Enfermedad de Fox – Fordyce.
Palabras clave: Enfermedad de Fox-Fordyce, Prurito Vulvar, Enfermedades de las Glándulas Sudoríparas, Glándulas Sudoríparas . (fuente: DeCS BIREME).
Fox-Fordyce disease was first described in 1902 by George Henry Fox and John Addison Fordyce is an uncommon, inflammatory non-infectious dermatoses of apocrine glands(1). It is characterized by chronic processes and manifested by very itchy skin-colored papules, in parts of the body where the apocrine glands are concentrated(2). Its etiopathogenesis is little known and affects the areas with apocrine glands: the armpits, the groins, the pubic region, the perineum, the labia majora, the areolas and the umbilicus. It occurs mainly in postpubertal women, between 13 and 35 years old, although prepubertal and postmenopause(3,4) cases have been reported; without racial predilection and with an incidence not yet established(2). It mainly affects women in a ratio of 9 to 1; occasionally some cases have been reported in men(1) Due to emotional or physical stimulation of the apocrine glands, paroxysmal exacerbations are observed. Its treatment is discussed. Different therapeutic regimens have been used with disparate and not always satisfactory results(3,4,5).
The cause is an intraepidermal obstruction of the apocrine gland duct. The hypothesis is determined by hormonal and genetic factors, with histopathological criteria that include hyperkeratosis(2), obstruction of the follicular infundibulum(2), chronic inflammatory changes in the dermis1, and acinar dilation of the apocrine glands(1), which show a thick secretion of eosinophilic mucin in lumen(1). Treatment is not simple, as some treatment regimens can have annoying side effects and relapses are common(2). Other reviews do not specify a definitive treatment1, but describe some treatment options such as combined oral contraceptives to treat and reduce the symptoms of women of childbearing age(1). Even Isotretinoin has been used once in the treatment of this condition2, with variable results.
This aim of this study is to present a clinical case of Fordyce-Fox disease. It was decided to present this case because of the rare occurrence of this disease.
CASE PRESENTATION
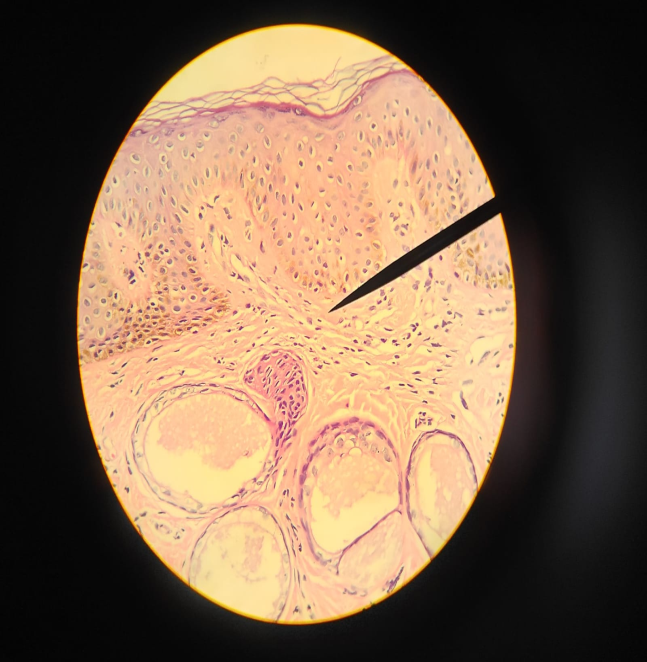
It is presented the case of a postmenopausal 53-year-old female patient, with five years as date of her last period and negative Papanicolaou in 2019, which was evaluated in a gynaecological-obstetric consultation at the General Hospital Maria Auxiliadora, in November 2019, due to a papular eruption in the vulvar region, associated with sporadic itching that she had for 5 months. A biopsy of the lesion was taken and sent to the Pathological Anatomy Service, receiving a dark brown-colored tissue fragment, 0.3 x 0.2 x 0.1 cm, which was properly processed, obtaining a histological sheet, in which dilated apocrine glands were evidenced. Those showed a thick secretion constituted by mucin in lumen; associated with mild inflammatory changes in the dermis (Figure 1 y 2). The patient met histopathological criteria for the diagnosis of Fordyce-Fox disease.
It was diagnosed as Fordyce-Fox disease. No medication has proven to be sufficiently effective, so it was decided to keep the patient on a symptomatic treatment.
DISCUSSION
The biopsy of the lesion exposed dilated apocrine glands, which showed a thick secretion of eosinophilic mucin in lumen. Histopathological criteria for the diagnosis of Fordyce-Fox disease include hyperkeratosis(2), obstruction of the follicular infundibulum(2), chronic inflammatory changes in the dermis(1), and acinar dilation of the apocrine glands(1), which show a thick eosinophilic secretion of mucin in its lumen(1). This case meets two of the four criteria mentioned, which in association with the clinical characteristics of the patient, allowed us to make the final diagnosis of Fordyce-Fox disease, discarding differential diagnoses such as lichen amyloidosis, lichen nitidus, eruptive syringomas, infectious folliculitis, follicular mucinosis, Darier's disease and so on(6,7).
Etiology has not yet been clarified. No genetic alterations or associated polymorphisms(3) have been described; however, Rubio and colleagues involve genetic, endocrine, metabolic or environmental elements with no evidence in favor of any of them(3,4,5).
As a first-line therapeutic option, some authors propose the use of calcineurin inhibitors, specifically pimecrolimus. This medication was developed to treat inflammatory processes, such as those characteristic of the disease after the rupture of the glandular duct, and by an unknown mechanism, it inhibits hyperkeratosis and follicular obstruction(8). However, other literature does not specify a definitive treatment(1); but some treatment options are described, such as combined oral contraceptives to treat and reduce the symptoms of women of childbearing age(1), which together with a symptomatic one, is a proposal to start the patient's treatment. The patient received only symptomatic treatment, which was a restriction in the evolution of the clinical condition.
CONCLUSION
It is important to emphasize the use of vulvar biopsy in cases of pruritus vulvae of uncertain etiology and the report the first nationwide case of Fordyce-Fox disease in vulva.
Acknowledgments: To Dr. Sigrid Abril Santos Laurente, for her teachings and guidance, in this case.
Authorship contributions: The author carried out the genesis of the idea, project design, data collection and interpretation, analysis of results and preparation of the manuscript of this research work.
Financing: Self-financed
Conflict of interest: The author declares that he has no conflict of interest in the publication of this article.
Received: December 8, 2019
Approved: March 17, 2020
Correspondence: Katherine Luisa Contreras Gala.
Address: Jr. Trinidad Morán 275. El Retablo-I Etapa Urbanization. Commas.
Telephone: 979483818
Email: katycl9@hotmail.com
BIBLIOGRAPHIC REFERENCES