ARTICLE ORIGINAL
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2019 - Universidad Ricardo PalmaDOI 10.25176/RFMH.v20i1.2548
ASSOCIATION BETWEEN CHARACTERISTICS OF MAMMOGRAPHIC CALCIFICATIONS AND MALIGINE NEOPLASIA IN A NATIONAL HOSPITAL, 2017
ASSOCIATION BETWEEN CHARACTERISTICS OF MAMMOGRAPHIC CALCIFICATIONS AND MALIGINE NEOPLASIA IN A NATIONAL HOSPITAL, 2017
Víctor Arteaga-Huanca1,a,
María Loo1,2,b,
Haylin Looc,
Lucy Cedillo-Ramirez1
1 Ricardo Palma University. Lima, Peru.
2 Pediatric Cardiology Unit. Edgardo Rebagliati Martins National Hospital. Lima, Peru.
a Medical student.
b Pediatrician doctor.
c Occupational Doctor.
ABSTRACT
Introduction: The presence of calcifications may be useful for the diagnosis of breast neoplasia. Objective: To determine the association between the characteristics of mammographic calcifications and malignant neoplasia. Methods: Observational, analytical, retrospective of cases and controls. Developed in the Gynecology Breast Pathology Unit. Female patients with mammogram suggestive of malignant neoplasm with a positive malignancy biopsy were included as cases, and 67 patients without histological evidence of malignancy as controls. Results: The average age of the cases was 54.12 years, in the controls 50.34. 50.9% (59) are older than or equal to 50 years, OR 2,399 95% CI (1,125-5,114) p = 0.022, of these 52.5% (31) had breast cancer. 9.5% (11) had calcifications suspicious of malignancy, the most frequent, the amorphous and the pleomorphic fine. 37.1% (43) of the total cases have the BI-RADS 0 category, 6.9% (8) BI-RADS 1, 8.6% (10) BI-RADS 2, 7.8 % (9) BI-RADS 3, 28.4% (33) BI-RADS 4, 8.6% (10) BI-RADS 5 and 2.6% (3) BI-RADS 6. 72, 7% (8) of patients with calcifications suspected of malignancy presented breast cancer. In the bivariate analysis, an OR of 4,163 was obtained. 95% CI (1,043-16,606) p = 0,031. In the multivariate analysis the association remained unchanged regardless of age and BI-RADS. Conclusions: Age 50 years or older and mammographic calcifications suspected of malignancy are associated factors for breast cancer.
Key words: Breast cancer; Mammography; Malignant neoplasm (source: MeSH NLM).
RESUMEN
Introducción: La presencia de calcificaciones puede ser útil para el diagnóstico de neoplasia de mama. Objetivo: Determinar la asociación entre las características de las calcificaciones mamográficas y neoplasia maligna. Métodos: Estudio observacional, analítico, retrospectivo de casos y controles. Desarrollado en la Unidad de Patología Mamaria de ginecología. Se incluyeron como casos a pacientes mujeres con mamografía sugerente de neoplasia maligna con biopsia positiva a malignidad y como controles a 67 pacientes sin evidencia histológica de neoplasia. Resultados: La edad media de los casos fue de 54,12 años, en los controles 50,34. El 50,9%(59) son mayores o iguales a 50 años, OR 2,399 IC 95% (1,125 – 5,114) p=0,022, de estos el 52,5% (31) tenían cáncer de mama. El 9,5%(11) presentaron calcificaciones sospechosas de malignidad, las más frecuentes, la amorfa y la fina pleomórfica. El 37,1% (43) de los casos totales correspondieron a la categoría BI-RADS 0, el 6,9% (8) a BI-RADS 1, el 8,6% (10) a BI-RADS 2, el 7,8% (9) a BI-RADS 3, el 28,4% (33)a BI-RADS 4, el 8,6% (10) a BI-RADS 5 y el 2,6% (3) a BI-RADS 6. El 72,7% (8) de pacientes con calcificaciones sospechosas de malignidad presentó cáncer de mama. En el análisis bivariado se obtuvo un OR de 4,163. IC 95% (1,043 – 16,606) p = 0,031. En el análisis multivariado la asociación permaneció inalterada independientemente de la edad y BI-RADS. Conclusiones: La edad mayor o igual de 50 años y las calcificaciones mamográficas sospechosas de malignidad son factores asociados para el cáncer de mama.
Palabras Clave: Cáncer de mama; Mamografía; Neoplasia maligna. (fuente: DeCS BIREME).
Breast cancer is the most common cancer in women worldwide(1,2). In Peru, the number of cases ranks second in frequency among the neoplasms reported(3).
The breast cancer guide of the National Comprehensive Cancer Network (NCCN), states that mammography and physical examination are the tools that enable breast cancer screening, in other words, the identification of the nosological entity(4). Screening detects the breast cancer cases early and makes it possible to cure it.
The task of the radiologist is to identify the mammographic characteristics that have positive predictive value for malignancy and to translate this percentage to an international scale called Breast Imaging Reporting and Data System (BI-RADS). Industrialized countries reduce the breast cancer mortality rate by 2.2% per year by screening and early treatment(4). However, in Peru, the lack of specialized equipment and the lack of a culture of prevention do not allow the establishment of an effective national screening program, which implies that cancer is detected in late stages, reducing its chances of healing(5).
The purpose of this work is to generate knowledge so that the imaging support allows the identification of lesions with positive predictive value to malignancy in the Peruvian population.
METHODS
We conducted an observational, analytical, retrospective study of cases and controls female patients with mammography and anatomopathological diagnosis treated at the Breast Pathology Unit of the Hipolito Unanue Hospital in 2017. We reviewed the clinical histories of 46 female patients (cases) with mammography suggestive to malignancy with biopsy positive to malignancy and 67 (controls) with mammography suggestive to malignancy with biopsy negative to malignancy. The cases were defined as those patients with diagnosis of breast cancer; while controls were those with diagnosis not corresponding to malignancy. Four potentially associated variables were evaluated: age at risk, calcifications suspected of malignancy, breast composition and BI-RADS categories.
Numerical variables were presented as mean or median and standard deviation or interquartile range according to their distribution. Categorical variables were presented as frequencies and percentages. Crude and adjusted odds ratios were obtained using multiple logistic regression to evaluate the association of the type of calcifications with the presence of neoplasia demonstrated histologically.
RESULTS
We included a total of 116 patients who had mammography and anatomopathological report performed in the hospitalization of Hipolito Unanue during 2017. From the total population, 57.2% (67) did not develop breast cancer and 42.2% (49) were diagnosed with breast cancer, of this group 49.1% (57) were under 50 years and 50.9% (59) were the same age or over 50 years. Calcifications suspected of malignancy were present in 9.5% (11) of patients.
Figure 1, 1 shows two boxes. The box of breast cancer patients is more variable than the box of patients without breast cancer. Both boxes and whiskers are asymmetrical to the right. The minimum and maximum age values for cancer patients are 29 and 73 respectively. The median age of these patients was 54 years with an interquartile range of 45.5 to 64 years. For patients without cancer, age ranged from 25 to 72 years. The median age was 50 years with an interquartile range of 43 to 58 years.
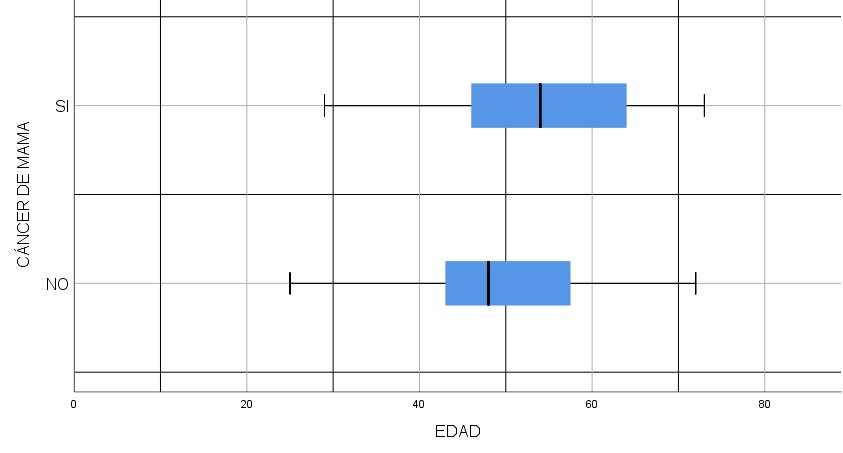
Figure 1. Age distribution according to breast cancer in patients of the Breast Pathology Unit.
The 37.1% (43) of the total cases have category BI-RADS 0, 6.9% (8) BI-RADS 1, 8.6% (10) BI-RADS 2, 7.8% (9) BI-RADS 3, 28.4% (33) BI-RADS 4, 8.6% (10) BI-RADS 5 and 2.6% (3) BI-RADS 6.
The composition of the breast was: almost entirely adipose tissue 8.6% (10), with scattered sectors of fibroglandular density 39.7% (46), heterogeneously dense 37.9% (44) and very dense 13.8% (16).
| Age | BIR-RADS Grade | Diagnosis | Calcification |
| 58 | 4c | Infiltrating ductal carcinoma | Fine pleomorphic |
| 55 | 4b | Infiltrating ductal carcinoma and ductal carcinoma in situ | Grouped amorphous |
| 54 | 4c | Infiltrating ductal carcinoma and ductal carcinoma in situ | Fine pleomorphic |
| 62 | 5 | Infiltrating ductal carcinoma | Fine pleomorphic |
| 50 | 5 | Infiltrating ductal carcinoma | Fine branching and fine pleomorphic |
| 42 | 4c | Infiltrating lobular carcinoma | Amorphous |
| 72 | 5 | Infiltrating ductal carcinoma and ductal carcinoma in situ | Amorphous |
| 45 | 0 | Ductal carcinoma in situ | Coarse heterogeneous |
| 49 | 4a | Fibrocystic breast disease | Suspicious microcalcifications |
| 47 | 4b | Fibroadenoma | Fine pleomorphic |
| 43 | 5 | Fibroadenoma | Grouped amorphous |
We detected 8 cases of breast cancer with suspicious calcifications and 3 controls detected with suspicious calcifications without malignancy. The histological strains found are infiltrating ductal carcinoma, ductal carcinoma in situ, and infiltrating lobular carcinoma. The suspicious calcifications found were: amorphous, coarse heterogeneous, fine branching, fine pleomorphic and no specified. In relation to the BI-RADS they were classified in grades 0, 4b, 4c and 5.
| Suspicious calcification | Infiltrating ductal carcinoma | Infiltrating lobular carcinoma | Ductal carcinoma in situ | Total |
| Amorphous | 2 | 1 | 0 | 3(37,5%) |
| Coarse heterogeneous | 0 | 0 | 1 | 1(12,5%) |
| Fine pleomorphic | 3 | 0 | 0 | 3(37,5%) |
| Fine branching | 1 | 0 | 0 | 1(12,5%) |
| Total | 6 (75%) | 1 (15%) | 1 (15%) | 8 (100%) |
The most frequent suspicious calcifications in breast malignancy were amorphous and fine pleomorphic, both with 37.5% of cases.
| Age at risk | Breast cancer | No breast cancer | P value | OR | 95% CI |
| Under 50 years | 18 (31,6%) |
39 (68,4%) |
0,022 | 2,40 | 1,1-5,1 |
| Over 50 years | 31 (52,5%) | 28 (47,5%) |
Of those over 50 years 52.5% (31) had breast cancer and 47.5% (28) did not are carries of cancer. The odds ratio was 2.40 95 % CI (1.13-5.11) with p = 0.022.
| Calcifications suspected of malignancy | Breast cancer | No breast cancer | P value | OR | 95% CI |
| No | 41 (39%) |
64 (61%) |
0,031 | 4,16 | 1,04-16,60 |
| Yes | 8 (72,7%) | 3 (27,3%) |
The 72.7% (8) of patients with calcifications suspected of malignancy developed breast cancer, and 27.3% (3) did not have breast cancer. An odds ratio of 4.16 95% CI (1.04-16.61) and p = 0.031 were obtained, a significant association was found.
| Grade of BI-RADS | Breast cancer | No breast cancer | P value | OR | 95% CI |
| Low risk | 8 (29,6%) |
19 (70,4%) |
0,041 | 2,83 | 1,03-7,76 |
| High risk | 25 (54,3%) | 21 (45,7%) |
Patients with high-risk BI-RADS (categories 4, 5 and 6), 54.3% (25) had breast cancer, compared with 29.6% of patients with low risk (categories 1, 2 and 3). An odds ratio of 2.83 95% CI (1.03-7.76) and a p value= 0.041 were obtained, a significant association was found.
In the multivariate analysis, the BI-RADS risk presented an OR of 1.21 95% CI (0.72-2.02) and p = 0.469, which was not significant. The over 50 years presented an OR of 2.54 95% CI (1.16-5.56), p = 0.020, while calcifications suspected of malignancy presented an OR of 4.44 (1.07-18.37) and p = 0.040.
DISCUSSION
Breast cancer is the most common cancer in women worldwide(1). In Peru it is a public health problem since it has a high burden of disease and also generates high costs for its treatment(6). For this reason, knowing the factors that allow accurate diagnosis is of vital importance. In our study, we found that the mean age of breast cancer patients was 54 years. Patients aged 50 years or older with breast cancer represented 63.3% of the total. This endorses and supports the American Cancer Society's recommendations for breast cancer screening. This suggests that women between the ages of 45 and 54 should have a mammogram annually(7). The incidence of this cancer in women in Peru is 40 per 100,000 inhabitants; However, the incidence between 45 and 54 years is 95 per 100 000(8). The association between age and breast cancer is widely known and the trend is that the older the patient, the greater the cancer(8). Regarding this variable, the study found that 52.5% of those older than 50 years were found inside breast cancer cases, which resulted in an odds ratio of 2.40 95% CI (1.13-5.11) and p = 0.022 (< 0.05). This contrasts with the trend demonstrated by S. Eve Singletary(9) in "Rating the Risk Factors for Breast Cancer", where the incidence is extremely low in those under 30 years (incidence less than 25 per 100,000). But it increases linearly until the age of 80 years. The relative risk for women older than 65 years compared to those younger than 65 years is 5.8 in this study. Regarding the grade of BI-RADS, in the present study 54.3% of patients with high-risk BI-RADS (categories 4, 5, and 6) were found to be inside breast cancer cases. An odds ratio of 2.827 (95% CI (1.03-7.758) and p = 0.041 were obtained, which reveals that having a high-risk BI-RADS (categories 4, 5 and 6) confers a risk of 2.8 times in relation to having a low-risk BI-RADS (categories 1, 2, 3), was not considered grade 0 because by definition it requires another more specialized mammographic test (amplification) or ultrasound to catalog it properly. The BI-RADS classification is developed by the American College of Radiology and, as mentioned, is the currently used tool to inform mammography(10). Its importance lies in the fact that through the description of lesions, the presence of malignancy in the patient is predicted, being a very useful tool for indicating biopsy. In the study by Chris Bent and colleagues(11), entitled: “The Positive Predictive Value of BI-RADS Microcalcification Descriptors and Final Assessment Categories”, it is found that the risk of malignancy according to BI-RADS categories increases progressively, the difference between each category (p< 0.001) and each subcategory (p< 0.001) are statistically significant, demonstrating that the radiologist can satisfactorily stratify the malignancy potential with BI-RADS. The positive predictive values for malignancy according to BI-RADS system were the following: category 2: 0%, category 3: 0%, category 4: 13%, category 4B: 36%, category 4C: 79%; And category 5, 100% in contrast to our work agrees that the higher the BI-RADS, the higher the risk of malignancy; However, due to statistical limitations, the logistic regression of BI-RADS categories and subcategories was not significant in the multivariate analysis. The most common malignancy in our study is infiltrating ductal carcinoma (75%), followed by infiltrating lobular carcinoma (15%) and ductal carcinoma in situ (15%). Similar to this, it is observed in the result of the descriptive epidemiological study carried out from 1987 to 1999 by Christopher Li and colleagues(12), entitled “Trends in Incidence Rates of Invasive Lobular and Ductal Breast Carcinoma”, where it was established that the most common histological type in breast cancer is the infiltrating ductal carcinoma type (72.8%) followed by infiltrating lobular carcinoma (7.6%) and infiltrating ductal carcinoma and infiltrating lobular carcinoma (4.7%) of a population of 190 458 cases. In relation to the composition of the breast, it was found that those constituted by scattered sectors of fibroglandular density are the most frequent, followed by heterogeneously dense breasts. This contrasts with the study by Madiha Naseem and colleagues(13), in which are significantly associated (p = 0.031), after evaluating 937 women, the calcifications suspected of malignancy with heterogeneous breast density to fibroglandular predominance. Our study found no statistical association with breast cancer or mammographic calcifications. Increased breast density is known to be a risk factor for breast cancer because it prevents the visualization of mammographic findings by decreasing sensitivity(14). Calcifications suspected of malignancy are grouped in this study and are shown to have a significant association with malignancy. It is observed that 72.7% of patients with calcifications suspected of malignancy are inside breast cancer cases. With p = 0.031 95% CI (1.04-16.61). Having this type of calcifications represents a risk about 4 times higher compared to the group that does not have them. The characteristics of the calcifications are described according to the fifth edition of BI-RADS(15); However, one of the controls was described as suspicious calcifications, a term partially correct, because the fact that it is suspicious does not mean that the type of calcification should not be described. In turn, the correlation of the presence of any type of suspicious calcification conditions a BI-RADS grade ranging from 4 to 5, and it is not coherent in the BI-RADS system to define a case with a suspicious calcification (coarse heterogeneous) as BI-RADS 0, an event that occurs in one of the controls of this study(16). The calcifications associated with malignancy were found in order of frequency: fine pleomorphic (37.5%), amorphous (37.5%), fine branching (12.5%) and coarse heterogeneous (12.5%). In the study, entitled “Mammographic microcalcifications and breast cancer tumorigenesis: a radiologic-pathologic analysis” associate the morphology with risk of malignancy (p <.001), being the fine branching the one that has greater risk of malignancy with 70%, followed by fine pleomorphic (28%), coarse heterogeneous (20%), and amorphous (20%)(11).
CONCLUSION
Mammographic calcifications suspected of malignancy were a factor strongly associated with the presence of breast cancer regardless of age and BI-RADS classification.
Authorship contributions: The authors participated in the conception, drafting and final approval of the original article, as well as VAH in data collection.
Financing: Self-financed.
Conflict of interest: The authors declare no conflict of interest in the publication of this article.
Received: July 20,2019
Accepted: November 10, 2019
Correspondence: Víctor Gabriel Arteaga Huanca
Address: Avenida Perú 1680 San Martín de Porres, Lima-Perú.
Telephone: +993819417
Email: victor_arteaga92@hotmail.com
BIBLIOGRAPHIC REFERENCES
