CLINIC CASE
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2019 - Universidad Ricardo PalmaDOI 10.25176/RFMH.v20i2.2912
ULNAR NERVE INJURY AFTER RADIAL EXTRACORPOREAL SHOCK WAVE THERAPY IDENTIFIED WITH HIGH–RESOLUTION ULTRASONOGRAPHY: CASE REPORT
LESIÓN DEL NERVIO CUBITAL SECUNDARIO A TERAPIA DE ONDAS DE CHOQUE EXTRACORPÓREAS RADIALES IDENTIFICADA CON ULTRASONOGRAFÍA DE ALTA RESOLUCIÓN: REPORTE DE CASO.
Paul Terán Vela1,
Walter Insuasti Abarca2,
Diana Martínez Asnalema3,
Tania Platero-Portillo4,
Sebastián Ramos Rosas5,
Sussan Llocclla Delgado6
1Orthopedic surgeon, Orthopedic Specialties Center, Quito-Ecuador.
2Internal Medicine Department, Orthopedic Specialties Center, Quito-Ecuador.
3Physical Medicine and Rehabilitation Department, Luis Dávila General Hospital, Tulcan-Ecuador.
4Medical School, University of El Salvador, San Salvador - El Salvador.
5Medical Reviewer, Salud S. A., Quito - Ecuador.
6Biomedical Research Institute. Ricardo Palma University, Santiago de Surco-Peru.
ABSTRACT
A 49-year old woman was evaluated for developing bilateral acute medial elbow pain, numbness, and tingling sensation in the fourth and fifth fingers after receiving radial extracorporeal shock wave therapy (rESWT) for bilateral medial epicondylitis. Neurologic examination revealed the presence of Tinel’s sign, paresthesia and impaired two-point discrimination testing over the ulnar side of the fourth and fifth fingers bilaterally. High-resolution ultrasonography demonstrated findings of nerve injury, such as hypoechogenicity and increased diameter of both ulnar nerves. After conservative treatment, the patient improved her condition demonstrating an apparently acute compressive nerve injury as a result of the therapy. ESWT is used as a promising alternative for the treatment of various musculoskeletal disorders; however, there is limited evidence regarding its side effects, in particular peripheral mononeuropathy. To the authors’ knowledge, this is the first report demonstrating structural damage of a nerve after rESWT with the use of high-resolution ultrasonography.
Key words: Ulnar neuropathy; Extracorporeal shockwave therapy; Medial epicondylitis; Ultrasonography; Case report (source: MeSH NLM).
RESUMEN
Mujer de 49 años fue evaluada por desarrollar dolor súbito a nivel de los epicóndilos mediales conjuntamente con entumecimiento y sensación de hormigueo en el cuarto y quinto dedos después de recibir terapia de ondas de choque extracorpóreas radiales (rESWT) como tratamiento para epicondilitis medial bilateral. El examen neurológico reveló signo de Tinel positivo, parestesia y una prueba de discriminación de dos puntos alterada sobre la región cubital del cuarto y quinto dedos. La ultrasonografía de alta resolución demostró hallazgos de lesión nerviosa periférica tales como hipoecogenicidad y aumento del diámetro de ambos nervios cubitales. La paciente mejoró únicamente tras recibir tratamiento conservador, demostrando así una aparente neuropatía compresiva bilateral aguda como resultado de la terapia. ESWT se utiliza como una alternativa prometedora para el tratamiento de diversos trastornos musculoesqueléticos; sin embargo, existe evidencia limitada con respecto a sus efectos secundarios, en particular la mononeuropatía periférica. Según el conocimiento de los autores, este es el primer reporte que demuestra un daño nervioso estructural después de rESWT con el uso de ultrasonografía de alta resolución.
Palabras clave: Neuropatía cubital, terapia de ondas de choque extracorpóreas, Epicondilitis medial, Ecografía, Reporte de Caso (fuente: DeCS BIREME)..
Medial epicondylitis is a common disorder affecting the upper limb. Despite an overall prevalence of <1%, medial epicondylitis can affect between 3.8% and 8.2% of patients in occupational settings.(1)
Although non-surgical therapy and open surgical treatment are the pillars of treatment for this pathology, recent studies have evaluated the impact of non-traditional therapies such as extracorporeal shock wave therapy (ESWT) showing promising results(1,2); however, there is limited evidence regarding their side effects, particularly peripheral mononeuropathy. According to the authors' knowledge, this is the second case reporting a peripheral nerve injury after the application of extracorporeal shock wave therapy for medial epicondylitis(3), and the first which demonstrates structural nerve damage with the use of high-resolution ultrasonography. In addition, this report seeks to clarify the possible pathophysiological mechanisms involved in ulnar nerve injury due to radial extracorporeal shock wave therapy (rESWT).
CLINICAL CASE
A previously healthy 49-year-old woman came to our clinic for having pain at the level of the medial epicondyles in both arms of one-year progress. The patient is a cook and usually moves heavy objects from side to side. Initially, she was treated in another medical facility and diagnosed with bilateral medial epicondylitis, so she was prescribed several physiotherapy sessions that did not improve her condition. After a second evaluation at the same center, he was prescribed seven sessions of radial extracorporeal shock wave therapy (rESWT) at an interval of one per week. According to the patient, after the third session of rESWT, she felt numbness and tingling sensation in the fourth and fifth fingers bilaterally, symptoms that were not perceived before. In addition, the intensity of the pain increased to the point that prevented her from extending her elbows, so she decided not to receive any more rESWT sessions.
Three months after the last rESTW session, the patient was referred to our clinic. On physical examination, she was unable to extend her elbows beyond 90 degrees of flexion due to unbearable pain (10/10 on the Visual Analogue scale). Pain and swelling over the medial epicondyle muscles were evident. Neurological examination revealed the presence of the Tinel sign, paresthesia and an altered two-point discrimination test on the ulnar side of the fourth and fifth fingers bilaterally. Simple radiographs of both elbows were normal. Ultrasound elastography showed inflammation and fibrosis on the insertion of common flexor tendons in the medial epicondyle (Figure 1). High resolution ultrasonography showed hypoechogenicity and an increase in the diameter of both ulnar nerves (Figure 2). Finally, electrodiagnostic studies showed no evidence of ulnar or median nerve alterations, and blood tests showed mild dyslipidemia.
The first therapeutic attitude was to advise the patient to limit the repetitive activities of wrist flexion and forearm pronation, as well as to avoid lifting and handling heavy objects. Analgesics, lifestyle changes, diet and physiotherapy modalities such as ultrasound, TENS, exercises that improve range of motion and stretching were also prescribed.
In addition, we applied 10 sessions of high intensity laser (HIL) with the following protocol: Analgesia: dose: 10 J / cm2 in an area of 10cm2 and power of 5.00 W. Biostimulation: dose 60 J / cm2 in an area of 10cm2 and power of 5.00 W.
After two months, the patient significantly improved her symptoms. The patient was able to extend her elbows and the pain was almost gone (2/10 on the Visual Analogue Scale). Neurological examination and motor function tests were normal.
The Disabilities of the Arm, Shoulder and Hand (DASH) questionnaire measured before and after conservative management were A: 60.34, B: 50, C: 81.25 and a: 12.06, B: 25, C: 25, respectively. The patient continued to receive physiotherapy with graded introduction and progression of eccentric strength exercises.
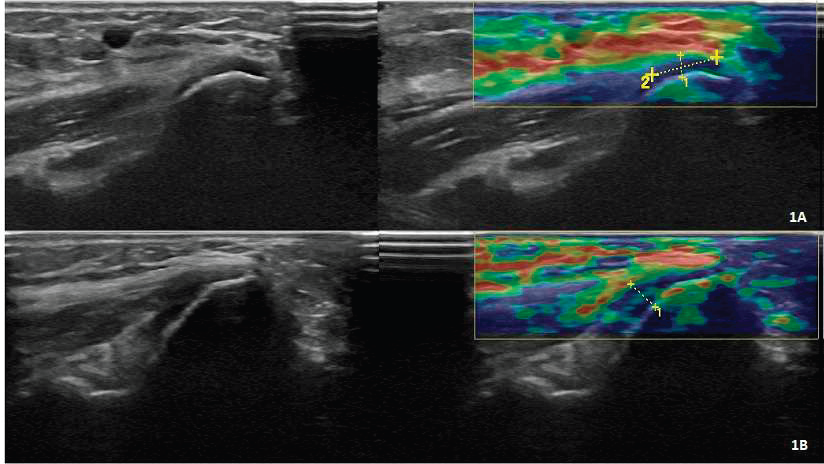
Figure 1. La elastografía por ultrasonido muestra inflamación y fibrosis sobre la inserción de los tendones flexores comunes en los epicóndilos mediales derecho (1A) e izquierdo (1B).
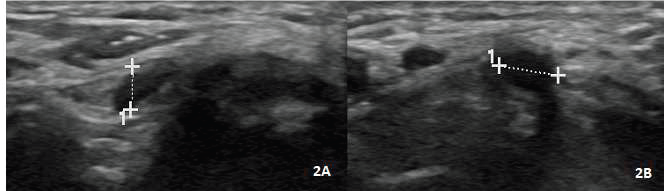
Figure 2. La ultrasonografía de alta resolución muestra hipoecogenicidad y un diámetro aumentado (4,5 mm) de los nervios cubitales derecho (2A) e izquierdo (2B).
DISCUSSION
Multiple evidence supports the use of extracorporeal shock wave therapy (ESWT) as effective and safe in the treatment of various musculoskeletal disorders(4) , and although no definitive recommendations can be made for the use of ESWT for medial epicondylitis at this time,(1,5), the International Society for Medical Shockwave Treatments (ISMST) has recognized its clinical use in this tendinopathy(6). In addition, Lee et al.(7) demonstrated the effectiveness of ESWT for newly diagnosed patients with lateral or medial epicondylitis compared to the local steroid injection. Their results confirmed that the ESWT group improved as much as the local steroid injection group; therefore, the study concluded that ESWT may be a useful treatment option in patients for whom local steroid injection is problematic. Similarly, Turhan et al.(8), in a retrospective analysis of 36 patients diagnosed with isolated medial epicondylitis refractory to conservative measures, found that ESWT was a good conservative management option by significantly improving VAS and Q-DASH scores (p <0.001) after 1 and 12 weeks after treatment.
On the other hand, regarding the side effects of ESWT, in the context of a randomized, placebo-controlled, single blind and multicenter study to evaluate the effectiveness of ESWT in lateral epicondylitis, Haake et al.(9) systematically recorded side effects of therapy. Overall, 399 cases of ESWT were analyzed, and the most common side effects included transient redness of the skin (21.1%), pain (4.8%) and small bruises (3.0%). Similarly, a literature review involving 631 patients who underwent ESWT for the nonunions treatment showed that the most common side effects associated with therapy included mild ecchymosis, petechiae, bruising, mild inflammation and temporary redness of the skin and, most importantly, all of these side effects could generally be avoided with precise guidance, proper positioning and strict adherence to the treatment protocol.(10)
Therefore, it is worth mentioning that, in addition to the common side effects mentioned above, ESWT could be associated with nerve damage as seen in this patient. Apparently, nerve injuries due to ESWT are extremely rare and rarely reported. A literature review notes only one case of ulnar neuropathy in the elbow with severe axonotmesis after local ESWT(3). In this case report, ESWT was applied at the elbow level showing clinical and electrodiagnostic evidence of direct nerve injury, which partially improved three months after the release of the ulnar tunnel with medial epicondylectomy.
Although concomitant ulnar neuritis can be observed in up to 20% of patients with medial epicondylitis(11), the history and evolution of this patient's disease lead the authors to hypothesize a possible direct injury of the ulnar nerve as a result of rESWT.
As described in the medical record, after the third session of rESWT, the patient experienced unbearable pain, as well as a numbness and tingling sensation in the fourth and fifth fingers that were not perceived before. Initially, our treatment protocol for the patient consisted exclusively of analgesia and rest, which gradually improved her symptoms. These findings support the hypothesis that an acute compressive nerve injury occurred, since, if it were the case of a concomitant chronic ulnar neuropathy, the patient would not have developed acute symptoms, much less there would have been a spontaneous recovery(12,13). Chronic nerve compressions are generally conditions of progressive deterioration that persist without proper intervention. Symptoms may begin with paresthesia and distal numbness, but unlike acute compressions, they often progress over time to muscle weakness and emaciation(12), which was certainly not the case with this patient.
In addition, it is worth mentioning that, since most peripheral nerve compressions are considered neuropraxia, the authors expected a spontaneous recovery of the patient in a prudential period, which was finally evidenced.
The etiology of acute nerve compression injuries is often evident as they are the result of a single traumatic episode(13).
In addition, it is important to note that the mechanisms by which ESWT could cause nerve damage are still uncertain. Hausdorf et al.(14) observed selective destruction of unmyelinated nerve fibers within the rabbit femoral nerves of post-high-energy ESWT. Similarly, Schelling et al.(15) showed in an in vitro study of frog sciatic nerves that the biological effects of shock waves on nerve tissue appear to be the result of cavitation. As a result, as Shim et al.(3) hypothesized, a possible mechanism of nerve injury could be the transmission of precipitated shock wave energy by the cavitation effect produced by fluid accumulation in medial epicondylitis.
Another mechanism for ulnar nerve injury after rESWT could be acute nerve compression due to adjacent soft tissue inflammation as seen regularly in elbow trauma.(16). To summarize, the recognized side effects of ESWT include swelling and small bruises(9,10); consequently, ESWT could have triggered or exacerbated regional inflammation around the medial epicondyle and thus compressing the adjacent ulnar nerve(3).
Normally, the effect of ESWT in any other application area would have been harmless. However, since the site of application of ESWT to the medial epicondylitis is an area of high risk of entrapment for the ulnar nerve, as it travels deep under the Osborne's ligament(17), swelling and underlying inflammation could have led to an acute injury compression and initiated a biological response. Such response includes thickening of the endoneurium walls and perineural microvessels, thickening of the endoneurium as a result of the edema, an increase in the amount of connective tissue; and later, thickening of the epineurium and perineurium due to fibrosis and edema. Finally, these pathophysiological characteristics that led to affect action potentials and axonal transport(18,19,20,21) were evidenced by ultrasonography.
Several studies have validated the importance of neuromuscular ultrasound for the diagnosis of peripheral nerve disorders(18,19,20,21). Since nerve thickening is the most reliable diagnostic indicator of an abnormal nerve, measurement of nerve size is critical.(20). Ultrasound findings in this patient revealed a nerve diameter of 4.5 mm. In relation to this, Beekman et al.(19) showed that patients with ulnar neuropathy in the elbow had a larger diameter of the ulnar nerve than the controls (p <0.0001). Reference values for ultrasound measurements showed that a diameter of the ulnar nerve greater than 2.5 mm at the level of the medial epicondyle was considered abnormal. Additional signs of compressive nerve injury consist of local thickening, hypoechogenicity with loss of fascicular pattern, a characteristic that was also evidenced in this patient, and intraneural hypervascularization in Doppler color or power(20,21).
Finally, it is imperative to mention the fact that the electrodiagnostic studies in this case were negative. Electrodiagnosis remains the gold standard for ulnar nerve neuropathy(18). However, diagnostic performance is lower, and data interpretations are often more difficult(22), as their sensitivity varies from 37% to 86%(19). Therefore, different studies(18,19,20,23) have suggested a multidisciplinary approach to the diagnosis of the ulnar nerve compression syndrome, through the analysis of clinical signs in combination with electrodiagnostic and imaging studies, as even in patients with evident clinical compression of the ulnar nerve, electromyography and nerve conduction studies may obtain false-negative results in up to 10% of the pacientes(24).
To explain the high incidence of false-negative results, the evidence supports technical errors as the main source of misdiagnoses.(25). Another possible explanation of a false-negative result in this case could be related to the time elapsed from the nerve injury to the time when the electrodiagnostic study was performed.
Consequently, it is important to highlight the use of ultrasound in this case. First, the increased cross-sectional area or diameter sensitivity of the ulnar nerve in the elbow is more than 80% in ulnar neuropathy. In addition, ultrasound can sometimes identify the entrapment site in patients with suspected ulnar neuropathy in the elbow, who attend with normal results on electrodiagnostic tests(20,26,27).
CONCLUSION
This case demonstrates the potentially harmful effects of rESWT application for medial epicondylitis. As indicated above, it is evident that different pathophysiological mechanisms could have been involved in the development of an acute injury of the ulnar nerve in this patient.
One limitation to consider is the retrospective nature of this report. As the patient received rESWT at another medical facility, we were unable to collect valuable information about the treatment protocol, including the dose of energy used, or the precise site of rESWT application. In addition, the therapy was apparently applied by professionals who were not certified by the International Society for Medical Shockwave Treatments (ISMST) or by the Ibero-American Federation of Shockwave Societies and Associations in Medicine (ONLAT). As a result, some specific requirements, necessary to ensure an appropriate application technique, minimize possible side effects and improve patient safety may not have been met.
Finally, it is imperative to highlight the use of high-resolution ultrasonography in this case as it allowed us to corroborate the diagnosis of ulnar neuropathy due to rESWT in the context of negative electrodiagnostic findings.
Authorship contributions: The authors participated in the genesis of the idea, project design, data collection and interpretation, analysis of results and preparation of the manuscript of the present research work.
Financing: Self-Financed.
Conflict of interest: The authors declare there is no conflict of interest.
Received: February 21, 2020
Approved: March 17, 2020
Correspondence: Walter Insuasti.
Address: Av.Miguel Angel y Calle de Las Avellanas, Ecuador.
Telephone: Ph: 593 (02)4503252 - 2267490 – 2267491
E-mail: walter_insuasti@hotmail.com
BIBLIOGRAPHIC REFERENCES
