ARTICULO DE REVISIÓN
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2020 - Universidad Ricardo PalmaDOI 10.25176/RFMH.v20i4.3034
THE USE OF CHEST COMPUTED TOMOGRAPHY SCAN IN THE CONTEXT OF THE SARS-COV-2 PANDEMIC
UTILIDAD DE LA RADIOGRAFÍA DE TÓRAX EN EL CONTEXTO DE LA PANDEMIA POR SARS-COV-2
Silvia Lucía Mayanga-Sausa1,2,a,b, Raúl Max Steve Guerra-Tueros1,2,a, Daniel Alcides Lira-Villasante1,3,a, Dayana Kim Pastor-Gutiérrez2,4,a
1Hospital Nacional Edgardo Rebagliati Martins-EsSalud, Lima-Perú.
2Clínica Internacional, Lima-Perú.
3Clínica Centenario Peruano Japonesa, Lima-Perú.
4Clínica Ricardo Palma, Lima-Perú.
aRadiologist.
bMaster in Education and Research in Health-UNMSM.
In the current SARS-COV-2 pandemic, the choice of an imaging modality to aid diagnosis is based on the patient's clinical conditions, laboratory tests, and the availability of imaging equipment in health facilities. Tomography (CT) and chest radiography (CXR) are the most widely used imaging modalities; CXR, with less sensitivity than CT, is an accessible method, less expensive and less exposure to health personnel, its use is recommended in emergencies and in hospital services. The objective of the article is to guide decision-making to choose an imaging modality according to scenarios, taking into account its potential benefits and deepening in the description of the radiographic characteristics of suspected SARS-COV-2 infection that may serve in emergencies and we assess disease progression using a scoring system.
Key words: Chest radiography; SARS-COV-2; Medical imaging (Source: MeSH NLM).
In the current situation of the SARS-COV-2 pandemic, Peru faces scenarios that change dynamically daily due to the increase in cases and the need to require health services. It is not supplied due to the over-demand of clinically serious patients and non-serious patients with the presence or absence of risk factors or associated comorbidities, who require medical attention and an imaging diagnosis if pneumonia is suspected(1).
From the beginning of the SARS-COV-2 pandemic to date, according to the published scientific literature, the pillars for the management of the patient suspected of SARS-COV-2 infection is based on the clinical characteristics and the availability of the tests laboratory, which confirm or rule out COVID-19. These two variables generate different action and decision scenarios for the correct and timely indication of imaging that corroborates the clinical diagnosis of suspected pulmonary involvement and that allows an objective assessment of the patient's evolution(2), such as computed tomography (CT) with an indication in hospitalized and symptomatic patients. However, CT is not affordable for all patients, nor is it available in all health facilities in the country. Other factors that must be considered are the availability of radiology equipment, the risk of contamination of personnel and the radiological diagnosis support room, as well as the use and availability of personal protective equipment (PPE)(3).
Therefore, in this article we propose management by scenarios to choose an imaging modality, focusing on the usefulness of chest radiography.
CHEST X-RAY IN THE CONTEXT OF ACTION SCENARIOS AGAINST THE SARS-COV-2 PANDEMIC
Chest radiography (CXR) is an imaging modality present in most health facilities and is the first imaging study to identify pulmonary pathology. In the 2003 SARS-VOC coronavirus epidemic, CXR helped to assess lung involvement and to predict the risk of mechanical ventilation or death(4,5). In the current coronavirus type 2 pandemic of 2019 (SARS-COV-2), The American College of Radiology (ACR) recommends the use of CXR in the portable modality(6) for hospitalized patients; however, in the United States emergency services, CXR is performed on all dyspneic patients with/without SARS-COV-2 infection(7,8).
The reported sensitivity for CXR is 69%(9) and for CT it is 97%(10); However, the CXR exceeds the results of the serological test to detect SARS-COV-2 infection applied in the first week of onset of symptoms (50% positive tests), which depends on the variability of producing antibodies in each individual(11). Despite the greater sensitivity of CT, the ACR does not recommend its use as a first-line test to diagnose SARS-VOC-2 lung involvement and should be reserved for hospitalized and symptomatic patients with specific clinical indications(6). Many health facilities prefer CT because it has a greater ability to detect pulmonary alterations in the presymptomatic and early symptomatic phase of COVID-19(12).
The greater diagnostic capacity of CT contrasts with the lower availability of CT scanners in health facilities, greater downtime of the CT environment due to the need for cleaning and disinfection after each patient, risk of transmission to health workers and other patients during the transfer, use of a greater number of personal protective equipment (PPE) and greater exposure to radiation for the patient(2,6).
It is known that CXR has a lower sensitivity to detect patients in the pre-symptomatic phase and the early symptomatic phase(9). Shi et al.(12), analyzed 81 CTs describing the chronology of the images in patients infected with SARS-COV-2. The ground-glass opacities were present in all phases of the infection, and as focal presentation and distribution in the periphery in the first week, they were later diffused and then disappeared as they appeared. During the course of the second week, the mixture of ground-glass opacities and multifocal consolidations was more evident and extensive, which were correlated with the moderate to severe clinical stage. Toussie et al.(7), analyzed the CXR of 338 patients infected with SARS-COV-2 who attended the emergency service, finding that the median number of days from the onset of symptoms to presentation in the emergency service was four days (2 to 5 days). These studies guide the usefulness of CXR in the emergency service in patients with symptoms of moderate to severe SARS-COV-2 lung disease, and there are sufficient criteria for the affected individual to have visible manifestations on radiography.
Murphy et al.(13), publish the preliminary results of an automated chest radiography reading system using artificial intelligence (AI) software programmed to identify characteristics of SARS COV-2. The results are encouraging, achieving performance comparable to six expert readers. In the first reports, the IA system reaches a sensitivity of 85% and a specificity of 61%.
While technology tries to demonstrate the usefulness of CXR in the SARS-COV-2 epidemic, health professionals must be prepared to use this imaging modality in the context of the reality of our health system, with shortage of EEP and laboratory tests, which pose daily challenges.
FINDINGS ON CHEST X-RAY IN THE SARS-COV-2 CONTEXT
In general, all imaging methods are not very specific to identify the etiology of pulmonary involvement; however, correlation studies of images and pathology have helped to establish patterns that guide us in the diagnosis(14).
Common findings in the lung parenchyma
The findings found in the CXR are described according to the glossary of terms of the Fleischner Society(15).
- Interstitial opacity: Small and innumerable linear opacities, focal or diffuse, are caused by the partial occupation of the airspace. Regarding interstitial thickening, it is due to fluid, cells or fibrosis, partial collapse of the alveoli, increased volume of capillary blood or a combination of them(16) (Figure 1A). They are seen as faint opacities on CXR, but with greater attenuation than pulmonary airspace. In SARS-COV-2 involvement, these images are present during the course of the disease, predominate in the periphery but can extend to the hilar region. The distribution is focal and unilateral in early stages, then it is bilateral and diffuse(12,17) (Figures 2A, 3,4).
- Alveolar opacity: It is caused by the total occupation of exudate in the pulmonary alveoli(15). In the X-ray it is seen as homogeneous opacities with greater attenuation than the interstitial ones, poorly defined and blurred margins, and they may present an air bronchogram(18) (Fig.1B). In SARS-COV-2 infections and in other viral pneumonias, alveolar involvement is multifocal, which differentiates them from bacterial pneumonias that generally involve a single segment or lobe(14,17,18) (Figure 5B).
- Interstitial alveolar opacities: It is a mixed image of interstitial infiltrate to which alveolar opacities are added in the same places(15) (Figure 1C). They have been described in the course of the evolution of the SARS-COV-2 viral pneumonia and they are correlated with moderate to severe disease(12) (Figures 5A, 5C).
Uncommon findings in the lung parenchyma
- Pleural effusion: Its appearance depends on the amount of fluid, the position of the patient and the presence of adhesions. In the standing position, the pleural effusion has a characteristic appearance, such as a homogeneous inferior opacity in the lateral costophrenic sinuses with a concave interface towards the lung(14). Pleural effusion is difficult to identify with the patient in the decubitus position, in poor general condition, and on mechanical ventilation, so a standing or semi-sitting chest X-ray is suggested whenever possible. In the context of SAR-COV-2 infection, initial reports suggested the absence of this finding; however, current studies with CT in larger populations have demonstrated the presence of pleural effusion in the 2nd week of evolution and in patients who became complicated, the pleural effusion was visualized at the end of the 3rd week(12).
- Hilar prominence: The causes of hilar prominence are due to lymphatic or vascular pathology such as pulmonary thromboembolism(14). Viral and bacterial pneumonic infections can cause lymph node hypertrophy; In patients with SARS-COV2 infection, these findings have been described on CT, but they are rare and generally present in late stages of infection in patients with unfavorable evolution(12). Pulmonary thromboembolism is another complication recently described in these patients. In CXR, prominence of the hila is observed due to dilation of the pulmonary arteries and vascular redistribution towards the upper lobes at the expense of vascular dilation(14); the examination of choice is CT angiography.
- Single focal consolidation: It is the alveolar pattern that occupies a segment or lung lobe, and it is caused by bacteria such as pneumococcus(14).
-
Nodules/masses: The presence of these findings is unlikely to be of infectious; however, they can cause differential diagnosis problems with consolidations and atelectasis(14).
In the evaluation of CXR, a diagnostic classification of high, intermediate, low/inconclusive suspicion is proposed, based on the presence of common findings. The presence of unusual findings should lead us to think about differential diagnoses. Some authors consider that these findings are more reliable in young patients under 50 years of age because they are less likely to be confused with images of pre-existing lung disease(7) (Table 1).
FLUXOGRAM OF ACTION BY SCENARIOS TO REQUEST IMAGE STUDIES IN THE SARS-COV-2 CONTEXT
Scenario 1(Figure 6)
Patient with moderate to severe pulmonary clinical picture and confirmed laboratory test for infection by SARS-COV-2.
-
Radiographic diagnosis - scenario 1:
- Lung involvement compatible with SARS-VOC-2 viral pneumonia
- Initial RALE Score (if it is the first X-ray): ___ / 8
- RALE Score (evolution): ___ / 8 (from the second radiograph)
Scenario 2 (Figure 6)
Patient with suspected SARS COV-2 infection, moderate to severe clinical picture, laboratory result is not available or a false negative is suspected or there is no availability of laboratory tests and there is no availability of tomography, then radiography could be useful with a probability diagnosis (sensitivity of the radiograph: 69%), and taking into account the time of evolution from the onset of symptoms.
-
Radiographic diagnosis - scenario 2: In this scenario, the radiographic diagnosis must be made based on probabilities of suspicion, this classification was proposed for the CT reports, which we have adapted for the radiographic diagnosis, adding the respective recommendations. See Table 1.
- Radiographic findings of high suspicion for atypical pneumonia due to SARS-COV-2: request confirmation with laboratory / CT test
- Radiographic findings of intermediate suspicion for atypical pneumonia due to SARS-COV-2: request confirmation with laboratory test / CT
- Radiographic findings of low suspicion / inconclusive for atypical pneumonia due to SARS COV-2: consider alternative diagnosis according to clinical picture and history, clinical follow-up is suggested
- Normal radiography, infection by SARS-COV-2 is not ruled out: request tests of laboratory / CT
RADIOGRAPHIC EVOLUTION AND SEVERITY SCALE
Scale of evolution
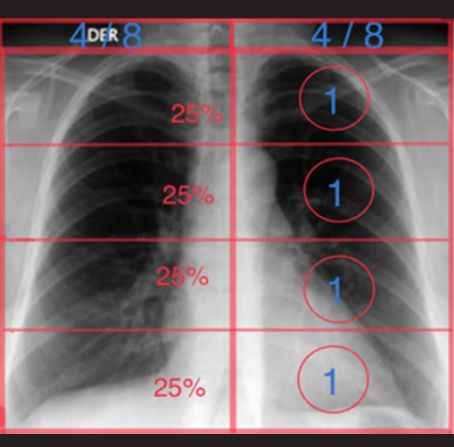
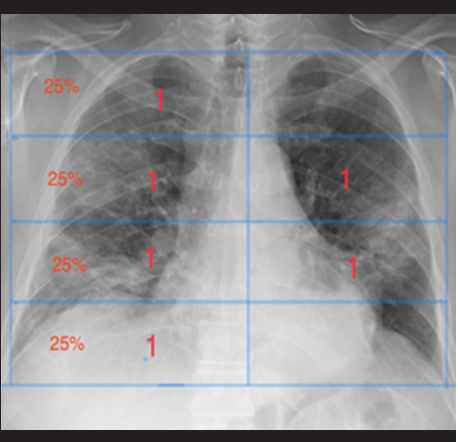
The most widely accepted scale to evaluate the evolution of radiographic images is the RALE Score proposed by Warren et al, to quantify pulmonary edema and adapted by Wong et al.(9) to evaluate quantitative progression of SARS-COV-2 infection. The scale consists of dividing the lung fields into 4 equal parts in such a way that 25% is assigned to each division and in each lung separately, with this procedure 8 equal parts are achieved (4 in the right and 4 in the left pulmonary field), to which 1 point is assigned to each area and a total score of 8 is achieved if all the segments were affected. The score is determined by adding the areas with suspicious images (Figure 7).Other authors prefer to assess lung involvement by assigning a score dividing the lung fields into thirds(7) as used in the 2003 coronavirus pandemic; we prefer to use the RALE Score proposed by Wong.
From a qualitative point of view, the appearance of alveolar opacities during the course of the disease(9,12,20) and pleural effusion after the 3rd week are considered unfavorable(12).
In the report: Radiographic evolution:
- RALE Score (1st. CXR)
- Favorable radiographic evolution due to decrease in the number of compromised lung area, RALE Score (../8)
- Stationary radiographic evolution since…. (date), RALE Score (../8)
- Unfavorable radiographic evolution due to greater involvement of the pulmonary areas and / or areas with alveolar infiltrate / pleural effusion are added or increased, tomography is suggested, RALE Score (../8)
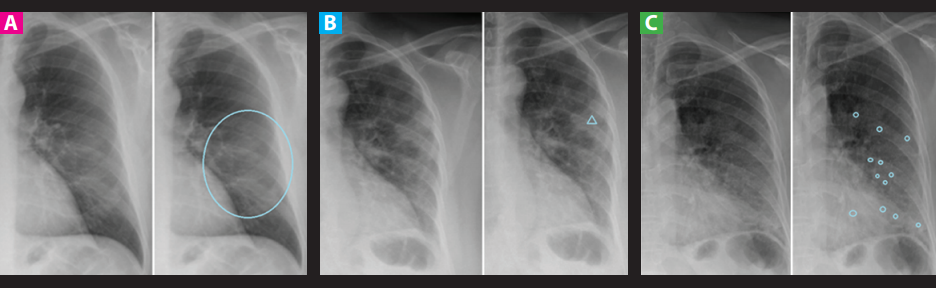
Figure 1. Common findings in CXR in the SARS-COV-2 context. A: Soft diffuse opacity. B: Alveolar opacity (∆). C: Alveolo-interstitial opacities (o).
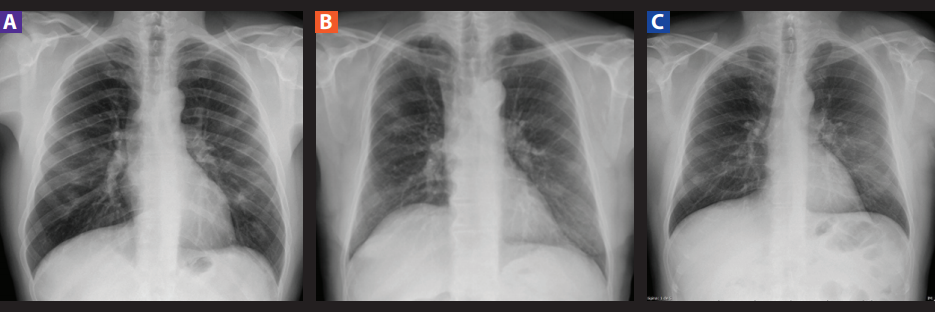
Figure 2. Common findings and lesions suggestive of SARS COV-2. A: Faint, multifocal peripheral opacities in bilateral middle third. B: Peripheral multifocal alveolo-interstitial opacities. C: Faint diffuse peripheral opacity in both pulmonary fields predominantly on the left.
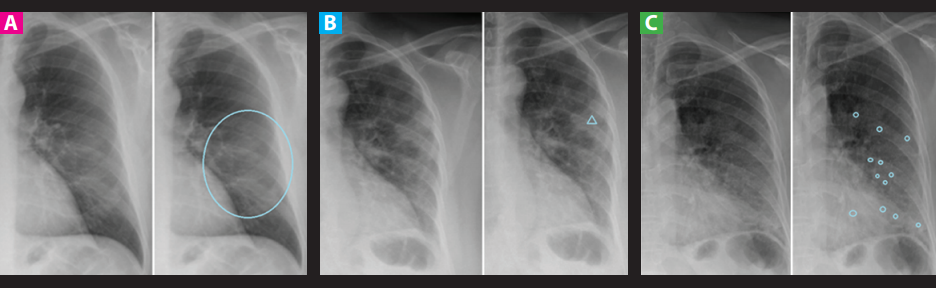
Figure 3. Location and distribution of the CXR findings in the SARS-COV-2 context. A: Location by segments in the RxT B: Focal distribution (★). C: Diffuse distribution (in the circle).
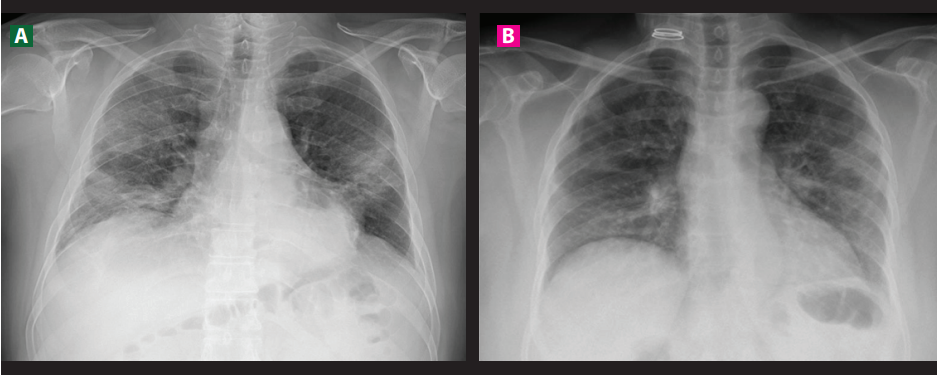
Figure 4. Location of the different types of lesions that conditions SARS COV-2, predominantly peripheral and bilateral.

Figure 5. Cases of high suspicion of SARS COVID-2. A: Diffuse bilateral alveolo-interstitial opacities of peripheral and basal distribution. B: Focal opacities in the right lung field with areas of peripheral parenchymal consolidation and left perihilar linear opacities. C: Faint bilateral peripheral opacities predominantly on the left, associating areas of alveolo-interstitial involvement.
Table 1. Diagnostic classification of SARS-COV-2 on chest radiograph.
| SARS-COV-2 classification Chest X-ray | Findings | Recommendations |
| High Suspicion ("Typical") Radiographic Findings for Atypical SARS COV-2 Pneumonia |
|
Request confirmation with laboratory tests and possibility of CT |
| Radiographic finding with intermediate suspicion ("Atypical") for atypical pneumonia due to SARS-COV-2 |
|
Request confirmation with laboratory tests and possibility of CT |
| Low suspicion / inconclusive radiographic findings for atypical SARS COV-2 pneumonia |
|
Request confirmation with laboratory tests and consider another alternative diagnosis according to the clinical picture and history |
| Normal X-ray (asymptomatic patients or with symptoms less than 5 days) | Absence of injuries | SARS-COV-2 infection is not ruled out. Request laboratory and / or CT tests |
Figure 7. Actual score. Determination by score assigned 1 point for every 25% of each lung.
CONCLUSION
- In laboratory-confirmed SARS-COV-2 infection with a moderate to severe clinical picture, the radiographic evaluation will be aimed at providing a scale of the degree of initial pulmonary involvement and for the evolution in hospitalization.
- In the suspicion of infection with a moderate to severe clinical picture, but with a negative or unavailable laboratory result, our radiographic evaluation will establish the degree of suspicion for SARS-COV-2 infection until confirmation with laboratory tests.
Author’s contributions: The authors participated in the genesis of the idea, project design, data collection and interpretation, analysis of results, and preparation of the final version of this research article.
Funding: Self-financed. .
Conflict of interest: The authors declare that they have no conflicts of interest in the publication of this article.
Recibido: May 20, 2020
Aprobado: June 07, 2020
Correspondence: Silvia Lucía Mayanga Sausa
Address: Calle J.J. Pardo 151 Urb. Astete la Perla–Callao, Lima-Perú
Telephone: 987800982
Email: lumaysa@gmail.com
REFERENCIAS BIBLIOGRÁFICAS