EDITORIAL
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2020 - Universidad Ricardo PalmaDOI 10.25176/RFMH.v20i4.3189
FEVER, COUGH AND COLD AND MORE. THE IMPACT OF THE SARS-COV-2 PANDEMIC ON THE CONSULTATION FOR RESPIRATORY DISEASES IN PEDIATRIC EMERGENCY
FIEBRE, TOS Y RESFRÍO ¿QUÉ MÁS TIENE? IMPACTO DE LA PANDEMIA POR SARS-COV-2 EN LA CONSULTA POR ENFERMEDADES RESPIRATORIAS EN LA EMERGENCIA PEDIÁTRICA
Viviana Pavlicich1,2,a
1Departamento de Urgencias. Hospital General Pediátrico Niños de Acosta Ñu, Asunción-Paraguay.
2Facultad de Medicina. Universidad Privada del Pacífico. Asunción-Paraguay.
aPediatrician, Pediatric Emergency Medicine
At the beginning of 2020, Sars-Cov-2 pandemic changed people's way of life. The health services underwent an organizational transformation to respond with the greatest possible security to the care of patients, trying to reduce the risk of contagion between them and the health personnel. The emergency services converted into the place of the first impact after the suspension of primary care and medical offices had to adapt to the new epidemiological situation.
As confirmed COVID 19 cases piled up and winter progressed, we were able to observe some notable changes. In May and June of this year, the monthly consultations in our service were reduced by 80% compared to the 12,000 consultations in 2018 and 2019. Although the “Stay at home” campaign and the fear of contagion could have influenced this decrease, I estimate that the decrease in disease burden due to the lack of viral transmission due to confinement also played an important role (Figures 1 and 2).
The magnitude of this global decrease in visits suggests that a combination of biological, psychological, and social factors influences the decisions of families to attend emergency and emergency services(1).
At the end of June, we observed a decrease of more than 50% in hospitalization since the PEM, but with a relative increase in the number of consultations. Fewer patients came, but with more urgent care needs. We corroborate this with the 4.5% increase in hospitalized children and a 5% increase in triage priority levels I, II, and III(2).
The burden of respiratory disease in May and June, (bronchiolitis, laryngitis, pneumonia, asthma attacks, recurrent obstructive bronchial syndromes, influenza-like illness, and upper respiratory tract infections), presented a 95% decrease compared to the previous two years in our service (Figure 3).
We know that almost all children are exposed to the respiratory syncytial virus (RSV) and other viral pathogens (eg, rhinovirus) during the first and second years of life. Of these, ~40% of children develop bronchiolitis clinical, and between 3 and 10% will be hospitalized(4,5).
In 2009 alone, there were 130,000 hospitalizations for bronchiolitis (18% of childhood hospitalizations), at a direct cost of $ 550 million, in the United States(6,7). We have not analyzed the costs in our hospital, but 567 hospitalizations of children with moderate to severe bronchiolitis in just 2 months of 2019, undoubtedly represent a challenge. If we estimate a requirement of ~5% mechanical ventilator attendance(8) and ~10% need for noninvasive ventilation or high-flow oxygen by nasal cannula, the magnitude of the impact can be easily deduced.
Expectation and concern were that COVID-19 will add to the other agents that cause respiratory infection in children and in some cases possible coexistence(5). Although we estimated that the suspension of the school calendar, the measures of population isolation, the acquisition of hygienic practices by the general population, were positive factors to reduce the incidence of infection in the youngest, we did not predict this degree of impact.
In the months of March, April, and part of May in Paraguay, there was the confinement of adults and children, which justifies a minimal seasonal viral transmission evidenced by the absence of consultations for respiratory syndromes. In mid-May, the adults resumed their work activities (phase 3) and we saw a slight increase in asthma and pneumonia. However, patients with bronchiolitis remained rare and generated little pressure on the system. Winter is not over yet and we ask ourselves: is its appearance only delayed?
The pronounced decrease in seasonal acute respiratory diseases in PEM seems to be explained simply by the suspension of classes. It is, then, necessary to evaluate interventions to be implemented from now on in schools to reduce the transmission of respiratory viruses during the winter that is not only focused on reducing that of SARS-CoV-2.
Classes were suspended to prevent the transmission of Covid-19 between children and from them to their caregivers. Current evidence suggests that they may not be large transmitters as initially thought(9) and that the severity of the disease in pediatrics is much less than in adults(10,11).
Important communication campaigns were carried out to produce habit changes in the population and measures and interventions have been demanded to reduce contagion in public places. Wouldn't it be an understandable approach for the future to carry out prevention efforts aimed at reducing the impact of the transmission of seasonal respiratory viruses to protect the little ones and those with special risk conditions?
On the other hand, consultations for simple colds also imply a high healthcare burden on our service. Educating the population on how to deal with mild and self-limited pathology is part of a medical literacy that will make it possible to direct resources to the care of the most serious patients. Learning about these changes in attendance could offer an opportunity to find alternative ways to support families outside of SEP in the future(12).
This epidemiological situation forced us to make changes and investments at the health level. It is therefore necessary to develop a model for pediatric emergency care that is not the same as the pre-pandemic period. It is an opportunity for improvements in triage, infrastructure, health education for the population, and the application of telemedicine to represent advances that are sustained over time.
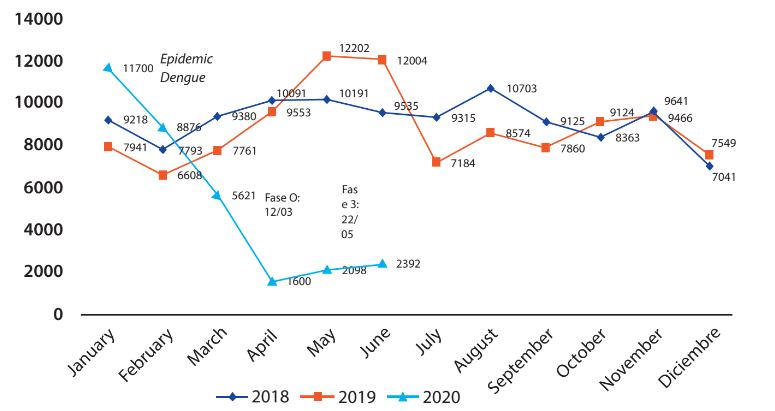
Figure 1. Consultations in the pediatric emergency service, years 2018, 2019. The pandemic period until June 2020. Hospital General Pediátrico Niños de Acosta Ñu.
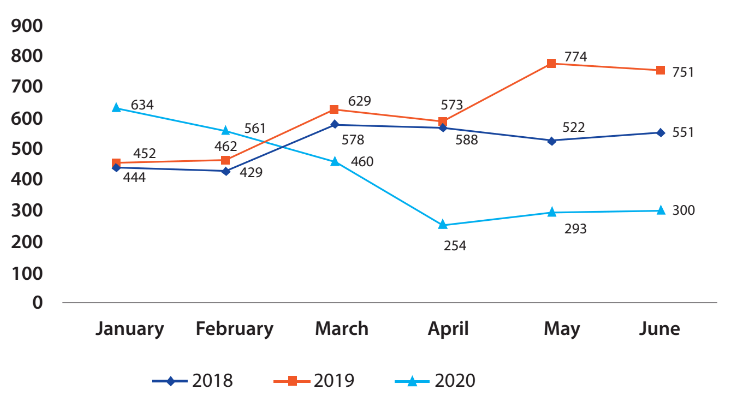
Figure 2. Hospitalizations since PEM 2018-2019 and in the pandemic period of 2020. General Pediatric Hospital Children of Acosta Ñu.
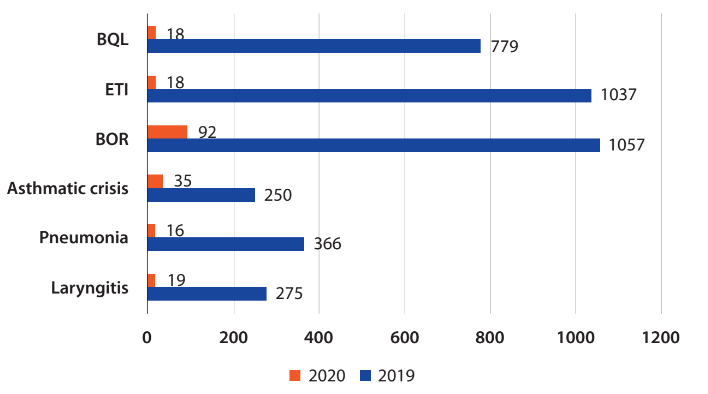
(BQL = Bronchiolitis ETI = Influenza-like disease BOR = Recurrent obstructive bronchial disease)
Figure 3. Visits for respiratory diseases in the month of June 2019 and 2020.
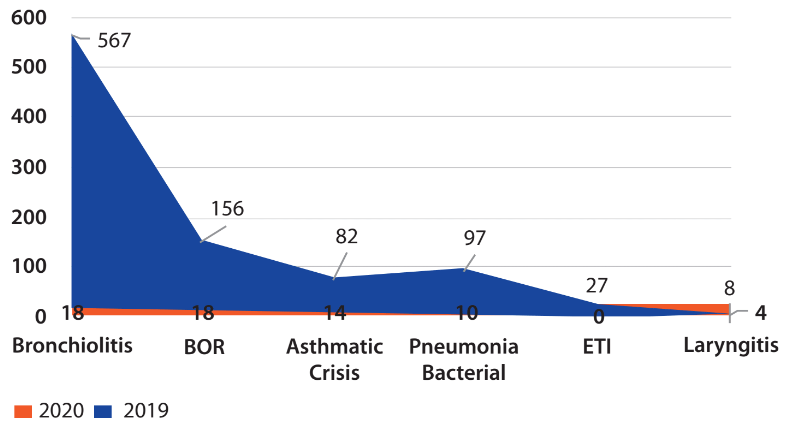
(ETI = Influenza-like disease BOR = Recurrent obstructive bronchial)
Figure 4. Hospitalization for diseases respiratory diseases in May and June 2019 and 2020 during the pandemic period..
Correspondence: Viviana Pavlicich
Address: Hospital General Pediátrico "Niños de Acosta Ñu", Arnaldo Bacigalupo, San Lorenzo, Asunción-Paraguay.
Telephone: +595 971 206043
Email: p_viviana@hotmail.com
REFERENCES
