ORIGINAL ARTICLE
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2020 - Universidad Ricardo PalmaDOI 10.25176/RFMH.v20i4.3220
THE ESTIMATE OF EXCESS REPORTED DEATHS COMPARED TO DEATHS ASSOCIATED BY COVID - 19 IN PERU FROM MARCH TO MAY 2020
ESTIMACIÓN DEL EXCESO DE MUERTES REPORTADAS FRENTE AL REPORTE DE FALLECIDOS POR COVID-19 EN PERÚ DE MARZO A MAYO DEL 2020
Pedro Fidel Grillo Rojas1,a, Roberto Romero Onofre1,a,b
1Universidad San Martín de Porres. Lima, Perú.
aSurgeon, Specialist in health administration.
bDoctor in Health Management
Introduction: Mortality from COVID-19 is increasing, this being a concern for the authorities and the general population. Objective: To estimate the existence of an excess of total deaths between March to May 2020 concerning the number of deaths from COVID-19 reported by the Ministry of Health from COVID-19 and to establish a relationship between the excess of total deaths and the COVID-19 pandemic in Peru. Material and Methods: We compared the gap between the Sistema Nacional de Muertes (SINADEF) with the official deaths reported by COVID -19 from March 1 to May 31, 2020. Violent deaths (homicide, suicide, traffic accident, other accidents, and unknown deaths) were excluded. A seasonal linear regression was used to estimate the baseline of deaths, from January 1, 2017, to December 31, 2019, with a 95% confidence interval. The deaths reported in the National System of Deaths were compared to the initial deaths. The excess of reported deaths was estimated using the "simple difference method.” Results: The results of the investigation showed that the total excess deaths, from March 1 to May 31, 2020, is 2.24 times higher than the official number of deaths reported by COVID-19. Conclusion: The differences found may be directly associated with an unrecorded death from COVID-19 and other general causes of death related to failures in our Public Health System during the period of the pandemic.
Key words: COVID-19, SARS-CoV-2, Mortality, Pandemics(Source: MeSH NLM).
Mortality from the current pandemic has been one of the most critical concerns since its onset, especially in populations at risk.
Some studies projected that the lack of successful treatment or the development of an effective vaccine could cause around 500 million deaths from the pandemic, an important figure. It represents 6% of the world population(1), highly recommended suppression or mitigation actions to reduce said mortality projections.
Mortality, rather than the number of infected or confirmed patients, is the indicator that in most countries would give us the most vital information on the success or failure of the non-pharmacological interventions adopted and the preparation of health systems face the pandemic. It is done despite the ethnic, geographical, and demographic differences between countries and how countries and governments have dealt with mortality, in each of them.
Today’s consequences from COVID-19 are the high capacity to spread demonstrated by SARS Cov-2 among the population, the intrinsic deficiencies of health models, social inequities, a significant number of asymptomatic, pre-symptomatic, and the high number of medical health personnel working for humanitarian organizations(2), (3). All this has generated that the countries’ health systems’ capacity is under maximum tension in some of them, and in others, these capacities have been overwhelmed.
All these conditions have materialized in very high mortality in several countries and in short periods for which they were not prepared. It is also pertinent to think that there are under-registration problems due to the health services’ capacities to provide timely and quality information. The form of a collection of death data, among other reasons.
This reasonable doubt generates the need to try to make an evaluation in our country between the mortality reported by COVID-19 and the increase in global mortality reported in the National Death System of our country in the months since the beginning and with the highest incidence of the COVID-19 pandemic in our country, such as March, April and May 2020.
Therefore, the objective of this study was to estimate the existence of an excess of total deaths between March to May of 2020 regarding the number of deaths from COVID-19 reported by the Ministry of Health (MINSA) for COVID-19 and establish a relationship between the excess of total deaths and the COVID-19 pandemic in Peru.
MATERIAL AND METHODS
Type and design
The ecological study, comparing the projection of national data on mortality in Peru.
Population and sample
The national mortality data of the National Death System were analyzed(4) and the information reported by the MINSA on deaths from COVID-19 during 2020(5).
Variables and instruments
The variable evaluated was mortality, between March, April, and May 2020, evaluated through the projection of deaths from the data from 2017 to 2019; and comparing it with the real registry of deaths for the evaluation period and with the projection obtained added to the number of deaths from COVID-19 reported by the CDC.
Procedures
For data analysis, deaths reported as violent death (homicide, suicide, traffic accident; other accidents and unknown death) were excluded. The daily data of interannual deaths was obtained from 2017 to the year 2020, differentiated by gender. This data was revised to show the seasonal fluctuations in each of the years.
Statistical analysis
A projection of the number of deaths for the year 2020 was calculated through a seasonal linear regression, using the data from January 1, 2017, to December 31, 2019, with a 95% confidence interval.
It was compared with 1) the number of deaths reported in the National System of Deaths from January 1, 2020, to May 31, 2020, and 2) with the projection of deaths obtained through linear regression (baseline) for that The same period to which the deaths reported by COVID-19 were added in the months of March, April and May 2020.
The excess number of deaths reported among the three groups was estimated using the Simple Difference method.
Ethical aspects
The study worked with population data, without directly affecting any subject in the present study.
RESULTS
Source: SINADEF, Own Elaboration.
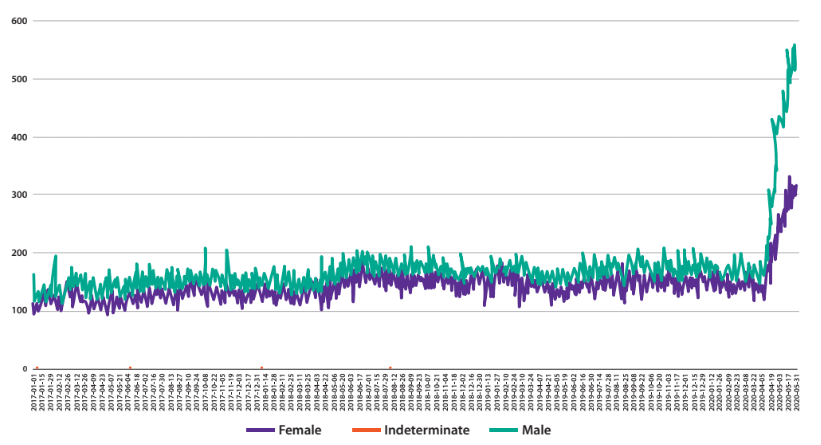
Figure 1. Total registered deaths by gender from January 1, 2017 to May 31, 2017- Peru.
Graph 1 shows a significant growth in the number of deaths that began in March 2020, reaching figures well above the seasonal fluctuations of previous years in May, with the number of male deaths far exceeding to the number of women who died until the end of May 2020.
Source: SINADEF, Own elaboration.
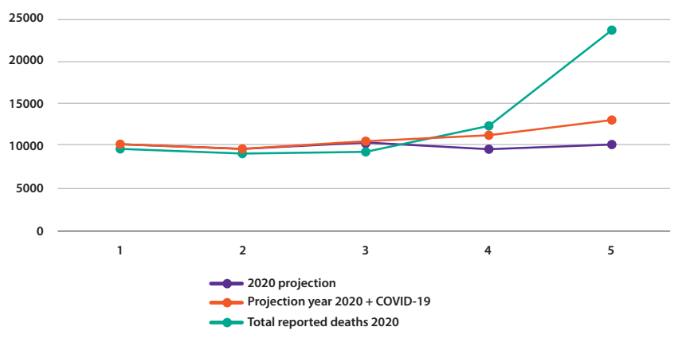
Figure 2. Total deaths reported by SINADEF until 05/31/2020 VS baseline year 2020 + deaths from COVID-19.
In Graph 2, it can be seen that there is an important difference in the number of deaths reported in the SINADEF versus the number of deaths of the projection with the addition of deaths from COVID-19 reported for the same period.
Table 1. Comparison of the numbers of deaths during the study period.
| Groups of records of deaths | 2020 | ||||
| Mar - 20 | Apr - 20 | May - 20 | Total | ||
| A | Real registry of deaths | 9393 | 12315 | 23675 | 45383 |
| B | Forecast 2020 + COVID-19 | 10485 | 11433 | 13041 | 34959 |
| C | 2020 Forecast (baseline) | 10437 | 9663 | 10239 | 30339 |
| D1 | Difference AC | -1044 | 2652 | 13436 | 15044 |
| D2 | Difference BC | 66 | 1770 | 2802 | 4638 |
When observing the results in Table 1, it has been found that there is a difference of 15,044 total deaths between the data entered in the SINADEF and a difference of 4,638 deaths reported as COVID-19 when compared to the projected baseline.
The number of deaths reported by COVID-19 is equivalent to 30.8% of total deaths in excess, finding that 10,406 deaths were not reported as COVID-19, finding a reason of 2.24 deaths reported in excess compared to the deaths from COVID-19 during that period.
DISCUSSION
One of the main discussions that have been taking place worldwide is how accurate are the figures that countries are currently reporting, focusing on the number of cases (confirmed by test or by clinical diagnosis or others), also on lethality or the crude ratio of fatality and mortality rates per thousand or in many cases per million inhabitants.
The case-fatality ratio is closely linked to the number of confirmed cases in each country. It is a manipulable data and depends on the countries’ capacity or willingness to carry out massive tests (serological or molecular).
The mortality rate is a less manipulable piece of information, but one that is currently facing questioning, due to the difference between countries when identifying cases or related to how the data is reported in each country.
The exercises carried out in different countries to identify this excess have been reported in deaths. The differences between them have been calculated, especially in those months in which an increase in the mortality reported by COVID-19 was observed.
The increase observed from March to May 2020 in the number of deaths reported in the SINADEF with a predominance of mortality in men is coincident with the epidemiological behavior of higher mortality in men compared to women. It is currently known that men and women have the same prevalence; However, men with COVID-19 have a higher risk of worse results and death, regardless of age, having a 2.4 times higher mortality in men than in women.(6)
In Peru, a level of underreporting of mortality of 43.3% is calculated, but with different levels of fluctuation at the national level.(7)
Regarding the count of deaths from COVID-19 in our country, the notification of deaths from COVID-19 should include confirmed suspected cases.(8) However, there is no certainty of compliance with this provision or the capture for the count by the MINSA. Therefore, it is likely that only the majority of cases have been reported as deaths from COVID-19 confirmed with serological or molecular tests.
The number of confirmed and probable deaths related to COVID-19 may not include deaths among people with SARS-CoV-2 infection who did not access diagnostic tests, tested falsely negative or the infection was post-test negative, died outside the scope of medical care, or health personnel does not suspect COVID-19 as a cause of death(9).
In the same report, an excess of 24,172 deaths was found for the expected forecast from March 11 to May 2, 2020. 78% of these deaths were laboratory-confirmed deaths or probable deaths or deaths associated with COVID -19, while 5,293 deaths, 22% were considered as excess deaths not identified as confirmed or probable COVID-19.
The Italian Institute conducted a study in May 2020 and found a difference of 46,909 total reported deaths and a difference of 27,938 (59.56%) deaths reported by COVID-19 to the baseline, calculating an excess of 18 971 (40.44%) deaths between March 1 and April 30, 2020.(10)
In a recent article published in The Economist in which they compared the information from the European mortality monitoring activity, for the years From 2017 to 2019, estimating a comparative baseline with 2020, for 24 European countries, they found that there would be more than 170,000 excess deaths in that continent until May 17, 2020.
The cases with the highest excess of deaths and magnitude, concerning the official figures from COVID-19, are Italy, the Netherlands, followed by Great Britain, with only 51, 60, and 77% of deaths from COVID-19 to total deaths recorded during that period. In this same article, Istanbul and Jakarta were included, observing 0% for Istanbul and only 14% for Jakarta. This difference will surely be more significant in the poorest countries, which have less capacity to evaluate and treat patients(11).
The results of the differences between the increase in the number of deaths reported in the SINADEF versus the number of deaths from COVID-19 are consistent to a greater or lesser extent with the findings reported in Italy and New York in the previously cited articles referring to the which also found unreported mortality during the COVID-19 pandemic, for the case of our study the number of excess deaths reported during the period is 2.24 times higher than the number of deaths officially reported by COVID-19 by the MINSA.
CONCLUSION
There has been an excess of 10,406 deaths reported during the months of March to May 2020 compared to the number of deaths reported by COVID-19 during that same period, which could be explained by an under-registration of deaths from COVID-19 or deaths associated with intrinsic problems of the health system, enhanced and lack of attention due to other morbidities during the period of the pandemic. Likewise, much higher mortality has been evidenced in men than, in women in the data entered in the SINADEF from March to May 2020, which is consistent with the possibility that an essential part of said excess deaths are by COVID-19.
Declaración: Declaramos que el material contenido en el manuscrito no ha sido publicado previamente ni remitido a otra revista biomédica.
Author’s contributions: The authors participated in the genesis of the idea, project design, data collection and interpretation, analysis of results, and preparation of the manuscript of this research work.
Funding: Self-financed.
Conflictos de intereses: Los autores declaran no tener conflictos de interés en la publicación de este artículo
Received: June 11, 2020
Aproved: June 24, 2020
Correspondence: Roberto Romero Onofre.
Address: Instituto de Investigación en Ciencias Biomédicas, Facultad de Medicina Humana, Universidad Ricardo Palma, Lima-Perú.
Telephone: +511 980 222 114
Email: carlosromeroonofre@hotmail.com
REFERENCIAS BIBLIOGRÁFICAS
