ARTICULO ORIGINAL
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2021 - Universidad Ricardo PalmaDOI 10.25176/RFMH.v21i1.3264
COVID - 19 MORTALITY RISK FACTORS IN HOSPITALIZED PATIENTS: A LOGISTIC REGRESSION MODEL
FACTORES DE RIESGO DE MORTALIDAD POR COVID-19 EN PACIENTES HOSPITALIZADOS: UN MODELO DE REGRESIÓN LOGÍSTICA
Irma Yupari-Azabache1,a, Lucia Bardales-Aguirre2,b, Julio Rodriguez-Azabache3,c, J. Shamir Barros-Sevillano3,4,d,Ángela Rodríguez-Diaz3,5,e
1 Instituto de Investigación, Universidad César Vallejo. Trujillo, Perú.
2 Departamento de Ciencias, Universidad Privada del Norte. Trujillo, Perú.
3 Facultad de Ciencias de la Salud, Universidad César Vallejo. Trujillo, Perú.
4 Sociedad Científica de Estudiantes de Medicina de la Universidad César Vallejo (SOCIEM UCV). Trujillo, Perú.
5 Centro de Salud San Martin De Porres, Facultad de Ciencias de la Salud, Universidad César Vallejo. Trujillo, Perú.
a Graduate in Statistics, Doctor in Education
b Statistical Engineer, Magister in Public Management
c Graduate in Statistics, Magister in Education
d Medical Student
e Surgeon, Master in Public Health
Introduction: The population is susceptible to COVID-19 and knowing the most predominant characteristics and comorbidities of those affected is essential to diminish its effects. Objective: This study analyzed the biological, social and clinical risk factors for mortality in hospitalized patients with COVID-19 in the district of Trujillo, Peru. Methods: A descriptive type of study was made, with a quantitative approach and a correlational, retrospective, cross-sectional design. Data was obtained from the Ministry of Health’s database, with a sample of 64 patients from March to May 2020. Results: 85,71% of the total deceased are male, the most predominant occupation is Retired with an 28,57% incidence, and an average age of 64,67 years. When it came to symptoms of deceased patients, respiratory distress represents the highest percentage of incidence with 90,48%, then fever with 80,95%, followed by malaise in general with 57,14% and cough with 52,38%. The signs that indicated the highest percentage in deaths were dyspnea and abnormal pulmonary auscultation with 47,62%, in Comorbidities patients with cardiovascular disease were found in 42,86% and 14,29% with diabetes. The logistic regression model to predict mortality in hospitalized patients allowed the selection of risk factors such as age, sex, cough, shortness of breath and diabetes. Conclusion: The model is adequate to establish these factors, since they show that a fairly considerable percentage of explained variation would correctly classify 90,6% of the cases.
Keywords: Risk, mortality, COVID-19, Comorbidity, Hospitalization (source: MeSH NLM).
On December 31, 2019, the Chinese government first reported an outbreak of the coronavirus disease (COVID-19) in Wuhan, the capital of Hubei province in China. This pandemic has spread rapidly from this city to all the areas of China and worldwide (1).
In Latin America, the first case was registered in Brazil on February 26, and the first death was reported in Argentina on March 7. Although the first confirmed cases were people arriving from trips, community contagion spread the pandemic to different countries on this continent, reaching Peru on March 6 of this year (2).
On March 15, the Peruvian government declared the country in a state of emergency, but despite this, the infections have been increasing, so that hospitals have collapsed. As of September 7, Peru reports 676,848 confirmed cases and 29,554 deceased cases, being the fifth country with the most infected worldwide and the first in deaths per million people, becoming the main public health and economic problem in the country (3,4).
Trujillo is one of the most populated districts in the department of La Libertad, located in the north of the country. To date, it counts more than 8,000 infected and more than 800 deaths; hospitals have collapsed to such an extent that people stand in long lines to be treated and some die without being treated (5).
The population is generally susceptible to this virus; however, within the characteristics of those affected, males and people with comorbidities have been more noticeable. Therefore, mortality generally occurs in older adults and people with diabetes, hypertension, obesity, and cardiovascular diseases(6,7). Thus, a study carried out in Cuba shows that in most cases it has a clinical picture corresponding to a self-limited upper respiratory infection, with a variety of symptoms according to risk groups, presenting a rapid progression to severe pneumonia and multi-organ failure, generally fatal in the elderly and with the presence of comorbidities(8).
Most people show symptoms in an interval of 3 to 7 days after infection, but in some, it can take up to 14 days, and infect others without realizing it. Symptoms can include fever, runny nose, sore throat, cough, fatigue, muscle aches, shortness of breath, sputum, hemoptysis, and diarrhea(9).
Another study conducted in China shows that patients diagnosed with COVID-19 were middle-aged (56 years), the majority (62%) were men, and around half (48%) had underlying chronic conditions being the most common arterial hypertension (30%) and diabetes (19%). Also, from the onset of the disease, the median time to discharge was 22 days, and the average time to death was 18.5 days(10). The average number of new cases per infected ranges between 2.24 (95% CI: 1.96-2.55) and 3.58 (95% CI: 2.89-4.39). A person can infect approximately 2 to 4 people(11).
A study carried out in Spain confirms that older adults living in residences are an important factor associated with mortality; regression models indicate a significant effect of temperature on the differences in incidence between the autonomous communities (12).
In Peru, patients with COVID-19 who were admitted to a public hospital in Lima, had a high mortality rate. It was independently associated with oxygen saturation, admission, and age over 60 years (13).
Due to the above, and wanting to contribute to research that helps us expand our knowledge of this disease, we ask ourselves the following question: What are the risk factors for mortality in hospitalized patients with COVID-19 in the Trujillo district? It was considered a research hypothesis that biological factors, such as gender and age; social like occupation; Clinical factors such as signs, symptoms, and comorbidities are risk factors for mortality in patients hospitalized for COVID-19 in the district Trujillo. As a general objective, we establish the analysis of biological, social, and clinical risk factors for mortality in hospitalized patients with COVID-19 in the Trujillo district. The study has specific objectives to propose a logistic regression model that allows determining the risk factors for mortality in hospitalized patients by COVID-19 in the Trujillo district, and estimate the degree of fit of the model to predict the death of hospitalized patients from COVID-19.
MATERIAL AND METHODS
Design and study area
Descriptive type of study, with a quantitative approach and correlational, retrospective, cross-sectional design (14).
Population and sample
The population consisted of all hospitalized patients in the Trujillo district with COVID 19 treated in the Trujillo microgrid. The information was obtained from the health ministry system, selecting a sample of 64 patients who met the selection criteria and who were collected during the period from March to May 2020
Procedure and variables
For data collection, the applied technique was the documentary analysis and the instrument the data collection sheet approved by the Ministry of Health and regulated within the System of the National Center for Epidemiology, prevention and control of diseases. Biological variables, such as gender and age, were reviewed; social like occupation; and clinical factors such as signs, symptoms and comorbidities.
Statistical analysis
For the analysis of the information, an Excel database was elaborated, the analysis was carried out in the SPSS version 26 Program. To identify the biological, social and clinical factors of risk of mortality in hospitalized patients with COVID-19, binary logistic regression analysis was performed using Ward's method; and to estimate the degree of fit of the model, the ROC curve was applied (15).
RESULTS
64 patients with COVID-19 hospitalized between March 1 and May 31, 2020, were identified. The mean age of the patients was 52.56 years (+/- 20.27), being male (68.8 %) with higher cases. The other epidemiological characteristics are presented in Table 1.
The most frequent clinical manifestations found in hospitalized patients were fever, respiratory distress, general malaise, cough, and abnormal lung auscultation (Table 2). Likewise, among the pre-existing comorbidities, cardiovascular disease was the most frequent comorbidity (Table 3).
In Table 4, it shows us that by means of the method in front of Wald it allowed the selection of the variables Age, gender, Cough, Respiratory difficulty, Joint pain and Diabetes, so the model would be as follows:
Where Y: Mortality (Deceased / Not Deceased)
X1: Age, X2: gender, X3: Cough, X4: Respiratory difficulty , X5: Diabetes
The OR value of the Age variable is equal to 1.11 (CI: 1.029-1.206), where both values are greater than 1. Therefore, the fact that a person is older is a risk factor mortality (death) of patients hospitalized for COVID 19.
The OR value of the gender variable is equal to 0.008 (CI: 0.000-0.258), where both values are less than 1. Therefore, the female gender reduces the probability of mortality (death) of patients hospitalized for COVID-19.
The OR value of the cough variable is 0.055 (CI: 0.005-0.648), where both values are less than 1. Therefore, the fact that a person has symptoms of cough reduces the probability of mortality (death) of the patients hospitalized for COVID-19.
The OR value of the respiratory distress variable is 89.703 (CI: 3.575-2250.718), where both values are greater than 1. Therefore, the fact that a person presents respiratory distress symptoms increases the probability of mortality or death of patients hospitalized for COVID-19.
The OR value of the joint pain variable is 37.099 (CI: 0.619-222.044); the interval includes 1. Therefore, the fact that a person presents a joint pain symptom is not significant to determine the mortality of patients hospitalized for COVID-19, so this variable is not included in the model.
The OR value of the diabetes variable is 77.478 (CI: 1.167-5142.378), where both values are greater than 1. Therefore, the fact that a person has comorbidity of diabetes increases the probability of mortality or death of patients hospitalized for COVID-19.
The model summary shows a minimal value of -2LL (-2 Logarithm of the likelihood), which indicates that the model obtained, in step 6, is better suited to the data than the models in the previous steps. Likewise, the coefficients of determination of R squared of Cox and Snell and R squared of Nagelkerke, indicate that 50.2% and 69.9% of the variation of the dependent variable death, is explained by the variables included in the model, showing a considerable percentage of explained variation(15 and 17).
The Hosmer-Lemeshow test for step 6 allows us to study the goodness of fit of the logistic regression model, having as a null hypothesis that there are no differences between the observed and predicted values, where the p-value of significance is greater than 0, 05 (p = 0.396> 0.05), therefore, we conclude that the model is well adjusted to the data(15).
Table 5 shows us that of the 43 patients hospitalized for COVID-19 in the Trujillo district who did not die, 40 patients are classified by the model, representing 93%, and of the 21 patients hospitalized for COVID-19 that did die, there are a total of 18 patients well classified by the model, representing 85.7%. It is expected that in the population the model would correctly classify 90.6% of the cases(16,17).
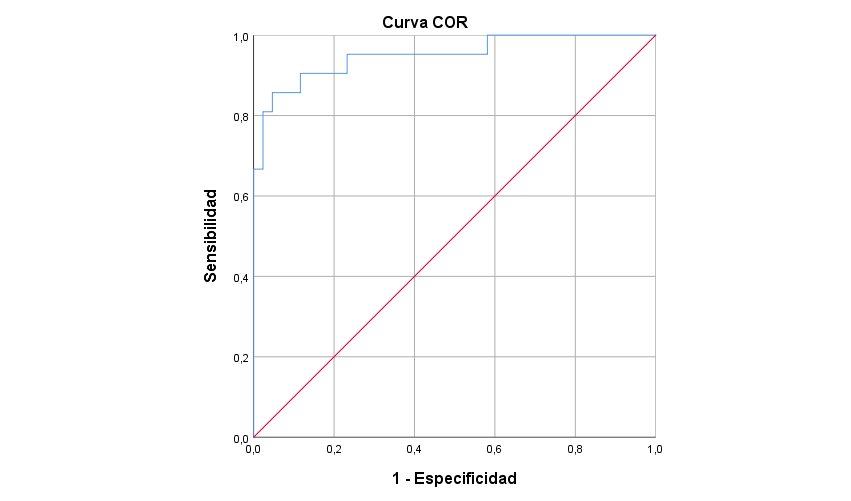
Figure 1 shows that the AUC (area under the ROC curve) for the model is equal to 0.95 (95% CI: 0.890 to 1). The result leads to rejecting the null hypothesis of non-discrimination (p <0.000). It is concluded that the model provides excellent discrimination power (15).
Table 1.General characteristics of patients hospitalized for COVID-19 who died or not in the district of Trujillo, Peru.
|
Characteristic |
Deceased |
Total (n = 64)
|
||||
|
Si (n = 21) |
No (n = 43) |
|||||
|
|
n |
% |
n |
% |
n |
% |
|
Age |
64.67 ± 16.88 |
46.65 ± 16.88 |
52.56 ± 20.27 |
|||
|
Gender |
|
|
|
|
|
|
|
Male |
18 |
85,7 |
26 |
60,5 |
44 |
68,8 |
|
Female |
3 |
14,3 |
17 |
39,5 |
20 |
31,3 |
|
Occupation |
|
|
|
|
|
|
|
Student |
0 |
0 |
2 |
4,7 |
2 |
3,1 |
|
Works with animals |
0 |
0 |
1 |
2,3 |
1 |
1,6 |
|
Health worker |
1 |
4,7 |
1 |
2,3 |
2 |
3,1 |
|
Others |
20 |
95,2 |
39 |
90,7 |
59 |
92,2 |
|
Housewife |
3 |
14,3 |
10 |
23,3 |
13 |
20,3 |
|
Unknown |
5 |
23,8 |
5 |
11,6 |
10 |
15,6 |
|
Military |
1 |
4,7 |
7 |
16,3 |
8 |
12,5 |
|
Retired |
6 |
28,6 |
1 |
2.3 |
7 |
10,9 |
|
Employee |
1 |
4,8 |
4 |
9,3 |
5 |
7,8 |
|
Entrepreneur/merchant |
1 |
4,8 |
4 |
9,3 |
5 |
7,8 |
|
Independent |
0 |
0 |
5 |
11,6 |
5 |
7,8 |
|
Driver |
2 |
9,5 |
1 |
2,3 |
3 |
4,7 |
|
Mine worker |
1 |
4,8 |
1 |
2,3 |
2 |
2,3 |
|
worker Agribusiness |
0 |
0 |
1 |
2,3 |
1 |
1,6 |
Table 2. Signs and symptoms of patients hospitalized for COVID-19 who died or not in the district of Trujillo, Peru
|
Signs |
Death |
Total (n = 64) |
|||||
|
Yes (n = 21) |
No (n = 43) |
||||||
|
|
n |
% |
n |
% |
n |
% |
|
|
Temperature |
|
37,6 ± 0,9 |
37,4 ± 0,9 |
37,4 ± 0,9 |
|||
|
Dyspnoea |
Yes |
10 |
47,6 |
17 |
39,5 |
27 |
42,2 |
|
No |
11 |
52,4 |
26 |
60,4 |
37 |
57,8 |
|
|
auscultation abnormal lung |
Yes |
10 |
47,6 |
24 |
55,8 |
34 |
53,1 |
|
No |
11 |
52,4 |
19 |
44,2 |
30 |
46,8 |
|
|
abnormal findings lung Rx |
Yes |
7 |
33,3 |
19 |
44,2 |
26 |
40,6 |
|
No |
14 |
66,7 |
24 |
55,8 |
38 |
59,4 |
|
|
Symptoms |
|
|
|
|
|
|
|
|
Fever |
Yes |
17 |
81,0 |
34 |
79,1 |
51 |
79,7 |
|
No |
4 |
19,1 |
9 |
20,9 |
13 |
20,3 |
|
|
General malaise |
Yes |
12 |
57,1 |
28 |
65,1 |
40 |
62,5 |
|
No |
9 |
42,9 |
15 |
34,88 |
24 |
37,5 |
|
|
Cough |
Yes |
11 |
52,4 |
28 |
65,1 |
39 |
61,0 |
|
No |
10 |
47,6 |
15 |
34,8 |
25 |
39,1 |
|
|
Sore throat |
Yes |
4 |
19,1 |
19 |
44,2 |
23 |
35,9 |
|
No |
17 |
81,0 |
24 |
55,8 |
41 |
64,1 |
|
|
Shortness of breath |
Yes |
19 |
90,5 |
20 |
46,5 |
39 |
60,9 |
|
No |
2 |
9,5 |
23 |
53,5 |
25 |
39,1 |
|
|
Diarrhea |
Yes |
3 |
14,3 |
9 |
20,9 |
12 |
18,8 |
|
No |
18 |
85,7 |
34 |
79,1 |
52 |
81,3 |
|
|
Nausea |
Yes |
2 |
9,5 |
6 |
14,0 |
8 |
12,5 |
|
No |
19 |
90,5 |
37 |
86,1 |
56 |
87,5 |
|
|
Headache |
Yes |
2 |
9,5 |
13 |
30,2 |
15 |
23,4 |
|
No |
19 |
90,5 |
30 |
69,8 |
49 |
76,6 |
|
|
Muscle pain |
Yes |
5 |
23,8 |
13 |
30,2 |
18 |
28,1 |
|
No |
16 |
76,2 |
30 |
69,8 |
46 |
71,9 |
|
|
Abdominal pain |
Yes |
1 |
4,8 |
2 |
4,7 |
3 |
4,7 |
|
No |
20 |
95,24 |
41 |
95,4 |
61 |
95,3 |
|
|
Chest pain |
Yes |
2 |
9,5 |
12 |
27,9 |
14 |
21,9 |
|
No |
19 |
90,5 |
31 |
72,1 |
50 |
78,1 |
|
|
Joint pain |
Yes |
1 |
4,8 |
2 |
4,7 |
3 |
4,7 |
|
No |
20 |
95,2 |
41 |
95,4 |
61 |
95,3 |
|
Table 3. Comorbidities of patients hospitalized for COVID 19 who died or not in the Trujillo district, Peru
|
Comorbidities |
Died |
Total (n = 64) |
|||||
|
Yes (n = 21) |
No (n = 43) |
||||||
|
n |
% |
n |
% |
n |
% |
||
|
Cardiovascular disease (includes hypertension) |
Yes |
9 |
42,9 |
9 |
20,9 |
18 |
28,1 |
|
No |
12 |
57,1 |
34 |
79,1 |
46 |
71,9 |
|
|
Diabetes |
Yes |
3 |
14,3 |
1 |
2,3 |
4 |
6,3 |
|
No |
18 |
85,7 |
42 |
97,7 |
60 |
93,8 |
|
|
Chronic lung disease |
Yes |
2 |
9,5 |
0 |
0 |
2 |
3,3 |
|
No |
19 |
90,5 |
43 |
100 |
62 |
96,9 |
|
|
Cancer |
Yes |
3 |
14,3 |
0 |
0 |
3 |
4,7 |
|
No |
18 |
85,7 |
43 |
100 |
61 |
95,3 |
|
Table 4. Selection of variables associated with the mortality of patients hospitalized by COVID 19 in the district of Trujillo, Peru
|
Variables in the equation |
||||||||
|
|
B |
Standard Error |
Wald |
gl |
Sig. |
Exp(B) |
95% CI for Exp (B) |
|
|
Lower |
Upper |
|||||||
|
Age |
0,108 |
0,041 |
7,096 |
1 |
0,008 |
1,114 |
1,029 |
1,206 |
|
gender |
-4,856 |
1,79 |
7,392 |
1 |
0,007 |
0,008 |
0,000 |
0,258 |
|
Cough |
-2,901 |
1,26 |
5,318 |
1 |
0,021 |
0,055 |
0,005 |
0,648 |
|
Respiratory Distress |
4,497 |
1,64 |
7,480 |
1 |
0,006 |
89,703 |
3,575 |
2250,718 |
|
pain joints |
3,614 |
2,09 |
3,003 |
1 |
0,083 |
37,099 |
0,619 |
222,044 |
|
Diabetes |
4,350 |
2,14 |
4,138 |
1 |
0,042 |
77,478 |
1,167 |
5142,378 |
|
Constant |
-2,657 |
2,99 |
0,888 |
1 |
0,346 |
0,060 |
|
|
|
Summary of the Model: |
||||||||
Table 5. Classification table of observed and predicted cases for the mortality model in hospitalized patients for COVID 19 of the district of Trujillo, Peru
|
Classification table |
|||||
|
Observed |
Predicted |
||||
|
Deceased |
Percentage correct |
||||
|
No |
Yes |
||||
|
Step 6 |
Deceased |
No |
40 |
3 |
93,0 |
|
Si |
3 |
18 |
85,7 |
||
|
Global percentage |
|
|
90,6 |
||
|
DISCUSSION
The analysis performed on the results shows us that in Table 1, the mean age of hospitalized patients was 52.56 years, with deceased patients having an average age of 64.67 years. Likewise, 68.8% of hospitalized patients were male. In the same way, 85.7% of this gender predominated in the deceased. This is confirmed by the majority of investigations from different parts of the world, as well as the reports are shown by the MINSA, since the largest number of deceased people in Peru are those of the male gender (4).
On the other hand, 92.2% of patients had different occupations; however, we can see that, in deceased patients, retirees lead this group with 28.6%. According to the data analyzed, we can also affirm that the deceased had approximately 9.7 (+/- 9.9) days of average length of stay in hospitalization until their death. This information coincides with the study carried out at the Hospital de Lima-Perú where the authors mention that they had a time of illness until death of 8 days (+/- 3.0) (18) and having a minimal difference with the study of China since it mentions that the mean time from admission to death was 5 (3.0-9.3) days(19).
Table 2 shows that the mean temperature of hospitalized patients was 37.4 ° C ± 0.97. In deceased patients, the mean temperature recorded was 37.6 ° C ± 0.9. The most frequent signs in hospitalized patients were dyspnea in 42.2%, abnormal lung auscultation in 53.1%, and abnormal lung X-ray findings in 40.6%. In deceased patients, dyspnea, abnormal lung auscultation, and abnormal X-ray findings were presented. Pulmonary in 47.6%, 47.6% and 33.3% respectively. Likewise, in the study carried out in China, they affirm that fever and cough were the most frequent symptoms at the beginning of the disease and that dyspnea and chest tightness were much more common in deceased patients(19).
Table 2 also shows that the symptoms that most affected patients hospitalized for COVID-19 were fever with 79.7%, general malaise with 62.5%, cough, and respiratory distress in the same frequency with 60.9%. Similar results were obtained in deceased patients, as the symptoms of fever, general malaise, cough and respiratory distress in 81.0%, 57.1%, 52.4% and 90.5% were presented within this group of patients. This is similar to studies such as those published in Cuba and in our country where patients suffering from this disease presented similar symptoms(9).
The most frequent comorbidities of patients hospitalized for COVID-19 were hypertension in 28.1% of patients and diabetes in 6.3%. In deceased patients, cardiovascular disease predominated (including hypertension) in 42.9%, diabetes and cancer in 14.3% in both comorbidities, as shown in Table 3. Similar results were found in deceased patients from China, since The authors mention that chronic hypertension and other cardiovascular comorbidities were more frequent among deceased patients (54 (48%) and 16 (14%)) than recovered patients (39 (24%) and 7 (4%))(19).
Table 4 shows us that a logistic regression model has been established by selecting the variables age, gender, cough, respiratory distress, and diabetes. Likewise, the fact that a person is older and has respiratory difficulty are risk factors for mortality in hospitalized patients. This coincides with the studies carried out in China and by the Institute of Experimental Medicine of Peru since they mention that mortality generally occurs in older adults(6,7).
Among the comorbidities, we find Diabetes as a risk factor for the mortality of patients hospitalized for COVID 19. This is corroborated with the research carried out in Cuba, since the authors mention that one of the risk comorbidities is diabetes(8).
The results also indicate that the fact of being female and having a cough reduces the probability of mortality in patients hospitalized for COVID 19, corroborating the descriptive results, this is what was mentioned above, and most studies, as well as the Ministry of Health confirms it.
The analyzed indicators of the proposed logistic regression model shown in tables 4, 5, and figure 1 indicate that the model is significant and of good fit, concluding that it provides excellent discrimination power. Therefore, our contribution to the research is the proposal of the logistic regression model to predict mortality in hospitalized patients with its associated factors.
CONCLUSIÓN
In conclusion, the results show that the model is adequate to establish the risk factors for mortality, being the most significant within the biological factors age and gender, within the social factors none were included in the model and within the clinical ones the cough, respiratory difficulty and comorbidity, Diabetes. The coefficients of determination of R squared of Cox and Snell, and R are acceptable since they show a quite considerable percentage of explained variation, as well as that the model would correctly classify 90.6% of the cases.
Author’s contributions: The authors participated in the genesis of the idea, project design, data collection and interpretation, analysis of results and preparation of the manuscript of this research work.
Funding: Self-financed.
Conflict of interest: The authors declare that they have no conflict of interest
Received: September 11, 2020
Accepted: December 18, 2020
Correspondence: Irma Yupari-Azabache
Adress: Las Flores Mz B 5 Dpto 202, Trujillo–Perú.
Cell: +51 964612831
Email: iyupari@ucv.edu.pe
REFERENCES
