CASE REPORT
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2021 - Universidad Ricardo PalmaDOI 10.25176/RFMH.v21i2.3459
DENGUE WITH SIGNS OF ALARM AND LEPTOSPIROSIS IN A PEDIATRIC PATIENT WITH COVID-19
DENGUE CON SIGNOS DE ALARMA Y LEPTOSPIROSIS EN UN PACIENTE PEDIÁTRICO CON COVID-19
Mayron D. Nakandakari(1,a), Hamilton Marín-Macedo(2,b), Raúl Seminario-Vilca(2,b)
1 Universidad Nacional de la Amazonía Peruana. Loreto - Perú.
2 Departamente de Pediatría. Hospital Regional de Loreto “Felipe Santiago Arriola Iglesias”. Loreto - Peru.
a Resident in Pediatrics.
b Pediatric Specialist.
Dengue and Leptospirosis are endemic metaxenic diseases that affect tropical and subtropical areas, mostly in underdeveloped countries. In addition to this, the COVID-19 pandemic is causing a great deal of damage to both the population and the health level. This is the case of a 13-year-old patient who had fever, gingival and intermenstrual bleeding, abdominal pain and shortness of breath. She had SARS-CoV-2 Inmunoglobulin M (IgM) and Inmunoglobulin G (IgG) positive rapid test, and positive serology NS1 for Dengue and IgM for Leptospira. In addition, non-contrast pulmonary tomography showed areas of consolidated and frosted glass at the base level, as well as cysturitis. Diagnoses of COVID-19 pneumonia, Dengue with warning signs and Leptospirosis were had. Therapeutics were based on fluid therapy according to diuresis and blood pressure, symptomatic, oxygen support, constant monitoring and antibiotic therapy with Ceftriaxone, having a favorable evolution.
Keywords: Dengue; Leptospirosis; Coronavirus; Pediatrics. (Source: MeSH – NLM)
RESUMEN
El Dengue y la Leptospirosis son enfermedades metaxénicas endémicas que afectan áreas tropicales y subtropicales, en su mayoría de los países subdesarrollados. Sumado a ello la pandemia por la COVID-19, estos vienen generando mucho daño tanto a la población como a nivel sanitario. Se presenta el caso de una paciente de 13 años que cursó con fiebre, sangrado gingival e intermenstrual, dolor abdominal y dificultad respiratoria. Tuvo prueba rápida SARS-CoV-2 Inmunoglobulina M (IgM) e Inmunoglobulina G (IgG) positivo, y serología positiva NS1 para Dengue e IgM para Leptospira. Además, en la Tomografía Pulmonar sin contraste se evidenciaron áreas de consolidados y de vidrio esmerilado a nivel de las bases, además de cisuritis. Se tuvieron los diagnósticos de Neumonía COVID-19, Dengue con signos de alarma y Leptospirosis. La terapéutica se basó en fluidoterapia según la diuresis y presión arterial, sintomáticos, soporte oxigenatorio, monitoreo constante y antibioticoterapia con Ceftriaxona, teniendo evolución favorable.
Palabras Clave: Dengue; Leptospirosis; Infecciones por Coronavirus; Pediatría. (Fuente: DeCS-BIREME)
Dengue and leptospirosis are prevalent metaxenic diseases worldwide.
According to the World Health Organization (WHO), dengue is responsible for around 390 million infections per year, while leptospirosis is responsible for an estimated 500 thousand cases per year(1,2).
Both diseases usually occur in tropical and subtropical areas. It is much more frequent in underdeveloped countries, where there is a fragmented health system with many limitations(3).
In China, in December 2019, the report of cases of infections by an unknown virus, currently called SARS-CoV-2 and its disease COVID-19, began. This virus has spread exponentially fast, affecting more than 180 countries, becoming an uncontrollable pandemic for all health systems(4).
The arrival of SARS-CoV-2 in the Amazonian regions was inevitable, especially in Loreto - Peru, one of the regions worst struck by COVID-19, with a case-fatality rate of 4.38%, and where the Ministry of Health reported only about 1000 deaths, a number that is questionable and negligible due to the large degree of underreporting.
COVID-19, added to dengue and leptospirosis, has been causing great harm to the population and health care(5).
Thus, we present a case of coexistence of infections among COVID-19, dengue and leptospirosis in a pediatric patient treated in a hospital in the Peruvian Amazon.
CLINICAL CASE
This is the case of a 13-year-old patient from Iquitos – Loreto.
Who five days before admission started having recurrent fever and general malaise. Every time she had a fever, her mother was giving her Paracetamol 500 mg.
Three days prior to admission, the patient noted abundant active bleeding at the gingival level, as well as low intermenstrual bleeding. She denied any significant prenatal, natal, and postnatal history.
Due to the bleeding that she presented, she first went to the Centro de Salud de Nanay, later being referred to the Hospital de Apoyo Iquitos (HAI).
In that hospital, a hemogram was performed showing leukopenia, neutropenia, lymphocytosis, and severe thrombocytopenia, whereby she was hospitalized for two days with a diagnoses of dengue with alarm signs, in order to rule out leptospirosis. She started fluid therapy with 0.9% sodium chloride at a rate of 3 cc/kg-hour. On the second day of hospitalization, the patient began with respiratory distress. A rapid test for COVID-19 was performed, obtaining a SARS-CoV-2 IgM and IgG positive result, after which the diagnosis of COVID-19 pneumonia was raised, and intravenous ceftriaxone 1 g every 12 hours, intravenous dexamethasone 4 mg at 8 am and 4 pm, and oxygen therapy by high-flow nasal cannula (HFNC) at 2 liters/minute were started.
Likewise, she was referred to the Regional Hospital of Loreto “Felipe Santiago Arriola Iglesias” (HRL), which had been designated by the Ministry of Health as a COVID-19 hospital.
At the time of admission to the HRL, her oxygen saturation was 98% with HFNC at 2 liters/minute, the respiratory rate was 20 breaths/minute, and she maintained a mean arterial pressure (MAP) of 73.3 mmHg. On physical examination, she presented a generalized skin rash, as well as features of an old bleeding from the oral cavity. Regarding the respiratory system, the vesicular murmur was decreased in the lower 2/3 of both hemithoraxes. There were no added sounds. Abdominally, there was pain as a result of the superficial and deep palpation in the epigastrium. No alterations were found in the rest of the apparatus and systems.
Compared with the hemogram performed in the HAI, the complementary tests show a greater decrease in leukocytes and hemoconcentration, as well as an increase in platelets. There was also an elevated quantitative C-reactive protein, and liver enzymes (Aspartate aminotransferase and Alanine aminotransferase) that were present at around 10 times their normal value. Likewise, the serology result for dengue and leptospirosis was obtained, with NS1 positive for dengue and IgM for Leptospira (Table 1).
Table 1. Clinical laboratory results.
|
Laboratory tests |
Reference range (*) |
Before admission |
During hospitalization |
||
|
Day 1 |
Day 2 |
Day 3 |
|||
|
Hemogram |
|||||
|
Leukocytes (103/uL) |
5,5 - 15,5 |
5,1 |
4,3 |
5,9 |
5,5 |
|
Granulocytes (%) |
40 - 60 |
25,4 |
62,1 |
45,3 |
31,2 |
|
Lymphocytes (%) |
20 - 40 |
50,4 |
28,8 |
42 |
57,4 |
|
Eosinophils (%) |
1 - 4 |
3,5 |
5 |
4,1 |
4,5 |
|
Monocytes (%) |
2 - 8 |
1 |
0 |
2 |
1 |
|
Hemoglobin (g/dL) |
≥ 12,5 |
14,3 |
14 |
13,7 |
13 |
|
Hematocrit (%) |
37 |
41,9 |
41,9 |
39,8 |
38,9 |
|
Platelets (103/uL) |
150 - 350 |
17 |
45 |
48 |
81 |
|
Biochemical profile |
|||||
|
Urea (mg/dL) |
22 - 55 |
- |
19 |
- |
- |
|
Creatinine (mg/dL) |
0,5 - 1 |
- |
0,9 |
- |
- |
|
Lactate Dehydrogenase (U/L) |
240 - 479 |
- |
468 |
- |
- |
|
C-Reactive Protein (mg/L) |
< 5 |
- |
12,5 |
- |
- |
|
Aspartate aminotransferase (U/L) |
15 - 40 |
- |
728 |
- |
- |
|
Glutamate Aminotransferase (U/L) |
10 - 35 |
- |
215 |
- |
- |
|
Total protein (g/dL) |
6,4 - 8 |
- |
6,7 |
- |
- |
|
Albumin (g/dL) |
3,7 - 5,5 |
- |
3,7 |
- |
- |
|
Total bilirubin (mg/dL) |
0 - 1 |
- |
0,8 |
- |
- |
|
Direct bilirubin (mg/dL) |
0 - 0,3 |
- |
0,7 |
- |
- |
|
Blood type and RH factor |
- |
- |
O "Positive" |
- |
- |
|
Crops |
|||||
|
Blood culture |
- |
- |
- |
- |
Negative |
|
Urine culture |
- |
- |
- |
- |
Negative |
|
ELISA for Dengue |
|||||
|
IgM |
- |
Negative |
- |
- |
- |
|
NS1 |
- |
Positive |
- |
- |
- |
|
ELISA for Leptospira |
|||||
|
IgM |
- |
Reactive |
- |
- |
- |
|
Rapid test COVID-19 |
|||||
|
SARS-CoV-2 IgM |
- |
Positive |
- |
- |
- |
|
SARS-CoV-2 IgG |
- |
Positive |
- |
- |
- |
|
Thick drop |
- |
- |
Negative |
- |
- |
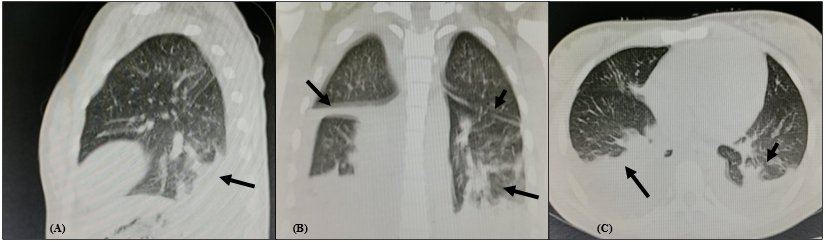
Radiologically, she had an anteroposterior chest X-ray exam showing a bilateral interstitial pattern (Figure 1). In the Pulmonary Multi-slice spiral computed tomography (MSCT) without contrast, areas of consolidation and ground glass were observed at the base level, in addition to cisuritis (Figure 2).
Figure 1. Anteroposterior chest X-ray on admission: bilateral interstitial infiltrate and horizontal cisuritis in the right pulmonary field.
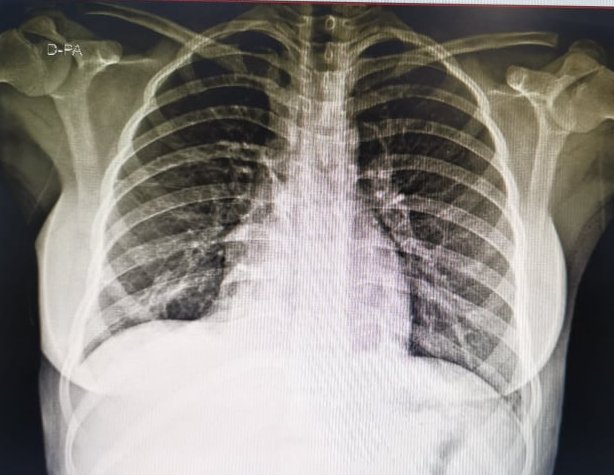
Figure 2. Pulmonary Multi-slice spiral computed tomography (MSCT) without contrast on admission: areas of consolidation and ground glass at the base level, in addition to cisuritis in both lung fields.
The diagnoses of the following diseases were raised:
-
1. COVID-19 pneumonia,
2. Dengue with warning signs,
3. Leptospirosis.
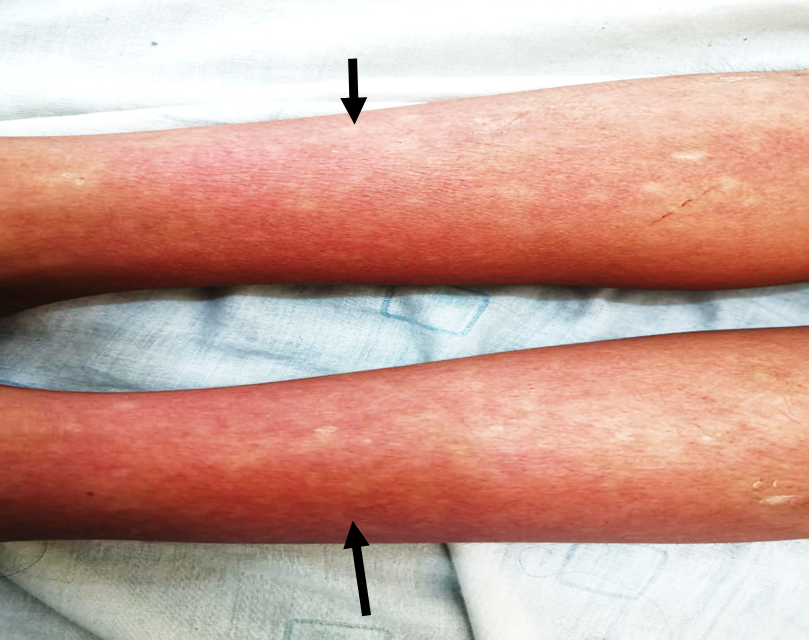
On day 5 of hospitalization in the HRL, platelets increased, hemoconcentration did not return, fever peaks subsided, and abdominal pain and respiratory distress did not recur. Likewise, a predominance of the upper and lower extremities skin rash was evidenced type "white islands in a sea of red" characteristic of the dengue convalescence phase (Figure 3). Due to her evolution and favorable prognosis, she was discharged from the hospital.
Figura 3. Skin rash on lower limbs type "white islands in a sea of red" from the convalescent phase of dengue.
DISCUSSION
The case of a patient who began with episodes of fever associated with gingival and vaginal bleeding was reported, whose first diagnostic suspicion in the Amazon region is metaxenic diseases, including dengue.
In addition, it is very common to see cases of co-infection between dengue with leptospirosis, Malaria and Urinary tract infections (UTIs), for this reason it was sought to rule out these diseases(6,7).
Currently, although there are no official reports that describe the rate of patients with COVID-19 co-infected with dengue and leptospirosis, this is very frequently observed within hospital management in the Loreto region.
On the other hand, it is mentioned that the pediatric population is usually the least affected by COVID-19, however, until epidemiological week 44 of 2020, 167 deaths were registered among children and teenagers in Peru(8). Likewise, there were several deaths of pediatric patients in the Loreto region who presented severe symptoms of respiratory failure associated with COVID-19.
Although the patient in the case did not die, she presented the need for oxygen support due to extensive lung lesions compatible with COVID-19. Likewise, there was no need to use corticosteroids, azithromycin, hydroxychloroquine or ivermectin, drugs that had been suggested at that time for the treatment of COVID-19(9).
Therapeutics consisted of adequate fluid therapy management according to diuresis and blood pressure, symptoms, oxygen support, constant monitoring, and antibiotic therapy with Ceftriaxone at 80 mg/kg/day due to the diagnosis of leptospirosis(10,11).
Additionally, although in the reported case COVID-19 and dengue have been presented as co-infections, it is important to emphasize that both share similarities within the pathophysiological events, as well as clinical findings such as maculopapular rash, gastrointestinal and respiratory symptoms, among others, which could be confusing to establish the diagnosis of one or the other(12). Likewise, cases where SARS-CoV-2 infection has led to false positives in dengue screening have been reported(13).
Furthermore, both dengue and COVID-19 can cause hyperactivity of the immune system, which can lead to events such as hypovolemic shock, vasoplegia, and cardiopulmonary collapse. The immune response can be so resounding that it can even trigger a cytokine storm syndrome, complicating the health and prognosis of the patient(14).
On the flip side, one of the diagnostic challenges was to determine the cause of the patient's shortness of breath. At first, pleural effusion was suspected due to a possible volume overload during hydration therapy associated with capillary leakage in dengue cases. Nonetheless, it was determined with the help of a pulmonary MSCT that the respiratory symptomatology was more associated with the COVID-19 that the patient had developed.
It is essential to mention that the case was registered during epidemiological week No. 26 of 2020. Despite the fact that the Centro Nacional de Epidemiología, Prevención y Control de Enfermedades (National Center of Epidemiology, Prevention a Disease Control, CDC) registered a lower number of dengue cases around this epidemiological week, it should be emphasized that the city of Iquitos and the Department of Loreto as such are endemic areas of dengue with frequent increases in the number of cases, which constantly lead to the over-demand of patients hospitalized for this disease.
Among the limitations of the case, it was not possible to take the molecular test for COVID-19 because there was not material to carry out this test in the hospital.
In conclusion, one of the pediatric cases showing coinfection between the new COVID-19 and the old and endemic metaxenics such as dengue and leptospirosis was presented.
It is suggested that, despite the restrictions established by the COVID-19 pandemic, it is necessary to continue actively carrying out epidemiological surveillance, as well as sanitary interventions for the control of dengue and leptospirosis, such as fumigation and the management of sewage. Due to the social isolation and quarantine measures dictated by the Peruvian Government, these interventions were not carried out, leading to an increase in dengue cases in the different regions of the Peruvian Amazon.
Authorship contributions: MN: Conception and design of the present work, analysis and interpretation of data, drafting of the manuscript, collecting or obtaining results, funding acquisition, approval of the final manuscript; HM: Patient or study material contribution, analysis and interpretation of data, critical review of the manuscript, technical and administrative advice, approval of the final manuscript. RS: Patient or study material contribution, critical revision of the manuscript, technical and administrative advice, approval of the final manuscript.
Este manuscrito fue elaborado utilizando la Guía CARE.
Funding sources: Self-financed.
Conflicts of Interest: The authors declare no conflicts of interest.
Received: December 18, 2020.
Approved: February 13, 2021.
Correspondence: Mayron D. Nakandakari.
Address: Av. 28 de Julio Nº 1063. Punchana, Iquitos, Loreto - Peru.
Telephone: (+51) 973 868 114
E-mail: mayron.nakandakari@outlook.com
BIBLIOGRAPHIC REFERENCES
