REPORTE DE CASO
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2021 - Universidad Ricardo PalmaDOI 10.25176/RFMH.v21i3.3922
SEIZURE OR CHILD ABUSE.
¿CRISIS CONVULSIVA O MALTRATO INFANTIL?.
Consuelo Luna-Muñoz(1,a,b), Martín Seminario-Aliaga(1,a,c), Sandra Mendoza-Cernaqué(a), Giuliana Reyes-Florian(1,a,c)
1 Hospital Nacional Edgardo Rebagliati Martins, Servicio de Emergencia Pediátrica, Lima-Perú.
a Surgeon.
b Specialist in Pediatrics, Doctor in Public Health.
c Resident in Pediatrics.
More child abuse cases are reported in Peru every year; however, there is no official report that describes the actual incidence, especially of the most vulnerable population such as infants. Signs of physical abuse generally involve brain injury and constitute shaken baby syndrome or pediatric abusive head trauma, which is a challenging diagnostic challenge. A 3-month-old infant is admitted to the emergency room for 30-minute generalized tonic-clonic seizures. On physical examination, the presence of a bony callus on the right clavicle was striking. A brain tomography and magnetic resonance imaging were performed, showing hyperintense lesions in the white matter, non-contrast enhancers, limited diffusion, and a bilateral subdural collection. Together, a bone survey was taken, which revealed multiple fractures in different areas of the body and suspecting the case of child abuse, so the relevant authorities (medical and judicial) were notified. Currently, the infant is in the custody of the Child Protection Unit, pending the definition of her final custody.
Keywords: Child abuse; Shaken baby syndrome; Pediatric abusive head trauma. (Source: MeSH – NLM)
RESUMEN
Cada año se informan más casos de maltrato infantil en el Perú, sin embargo, no hay un reporte oficial que describa la incidencia real, en especial de la población más vulnerable como son los lactantes. Los signos de abuso físico generalmente implican lesiones cerebrales y constituyen el síndrome del bebé sacudido o traumatismo craneal abusivo pediátrico, que representa todo un desafío diagnóstico. Lactante de 3 meses ingresa a emergencia por convulsiones tónico clónicas generalizadas de 30 minutos de duración. En el examen físico llamó la atención la presencia de un callo óseo en la clavícula derecha. Se realizó una tomografía y una resonancia magnética cerebral, que muestra lesiones hiperintensas en la sustancia blanca, no captadoras de contraste, con difusión limitada y una colecci se evidenció múltiples fracturas en distintas áreas corporales. Ante la sospecha del caso de maltrato infantil, se comunicó a las autoridades pertinentes (médicas y judiciales). Actualmente, la lactante se encuentra bajo custodia de la Unidad de Protección al Menor a la espera de la definición de su custodia final.
Palabras Claves: Maltrato infantil; Síndrome del bebé sacudido; Traumatismo craneal abusivo pediátrico. (Fuente: DeCS - BIREME)
Child abuse causes severe physical consequences, the most common injuries are those of the brain. Pediatric abusive head injury (AHT) involves a miscellany of symptoms and signs; therefore, the clinical picture is nonspecific and underdiagnosed. It occurs in children under 5 years of age, mainly infants(1).
In Peru, during the first semester of 2019, 5,458 cases of physical violence were reported in children under 5 years of age, where the main aggressors were parents (90.6%).(2) However, this report based on people served in emergency centers can underestimate the incidence in our country known for its ethnic, cultural, and geographic variability.
This article addresses the diagnostic complexity of pediatric abusive trauma in an infant admitted to our emergency room due to seizures.
Clinical case
The mother refers, a 3-month-old female patient, with a 72-hour illness time, presented free fall towards the ground, hitting her head, then “repetitive movements” are added in the arms and legs with ocular retroversion and hypersalivation, which is why she is taken to a hospital. Faced with clinical improvement, both parents request voluntary withdrawal from the hospital. However, the patient at home continued with involuntary movements, 10 to 12 times a day, for 48 hours.
He was admitted to the pediatric emergency service of the E. Rebagliati Martins National Hospital due to generalized tonic-clonic seizures lasting more than 30 minutes that gave way to intravenous midazolam treatment. On physical examination, a patient with seizure with the aforementioned characteristics, slight alteration of the respiratory pattern, looks pale, adequate perfusion, a bony callus is palpated in the right clavicle and the anterior fontanelle appears normotensive, the rest without particularities.
Background: Mother with insufficient maternal obstetric controls (No. 3), presented syphilis in the third trimester, did not complete the treatment. Patient with APGAR at birth 91 'and 95', weighs 3 125 grams, hospitalized in the Neonatal Intensive Care Unit for congenital neurosyphilis, is discharged at three weeks, completed treatment. He received a single immunization at the time of birth, without follow-up or a control card for the growth and development of the healthy child.
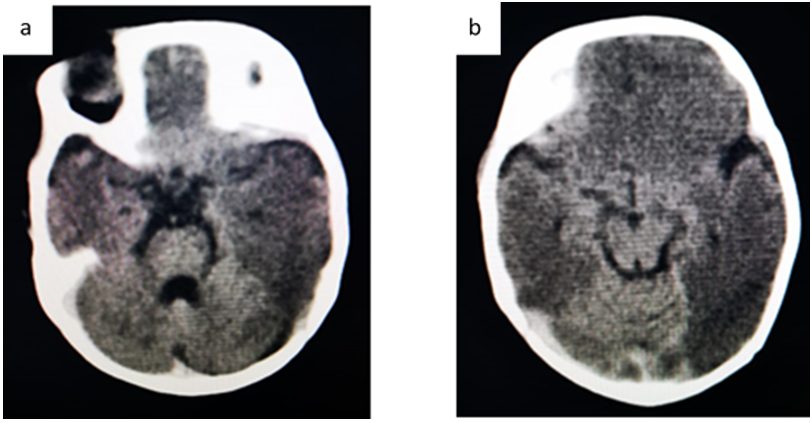
In the brain tomography (Figure 1), the pediatric neurosurgeon indicates multiple hypodensities at the level of the white matter, without compromising the basal ganglia, and requests an MRI to establish the etiology of these lesions.
Figure 1. Brain TEM showed (a) Hypodensities in white matter in frontal-parietal regions, predominantly right (b) Brain edema.
In order to be able to identify other focal and/or diffuse alterations in the patient's skeleton, a bone survey was indicated, which confirms an old fracture at the level of the right clavicle and shows a line of a linear fracture at the level of the right parietal shell. skull, in addition to a recent spiral fracture at the level of the right tibia, being immobilized with a plaster splint.
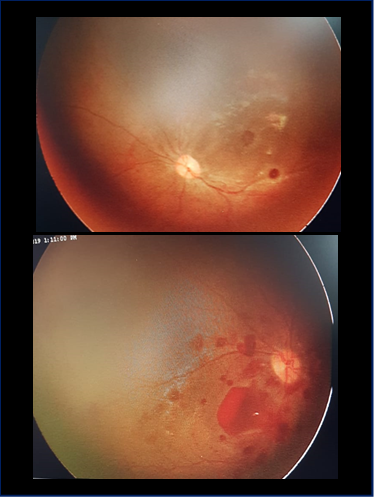
The evaluation, shows that the patient does not show fixation of the gaze before luminous or striking stimuli, reason for which pediatric ophthalmology is consulted, who evidence in the fundus of the eye, bilateral macular hemorrhages compatible with shaken baby syndrome or child abuse.
The patient is evaluated by a pediatric neurologist, who suggests studies of auditory and visual potentials, which did not present any alteration. Likewise, I recommend starting maintenance anticonvulsant therapy with phenytoin orally, with no recurrence of seizure.
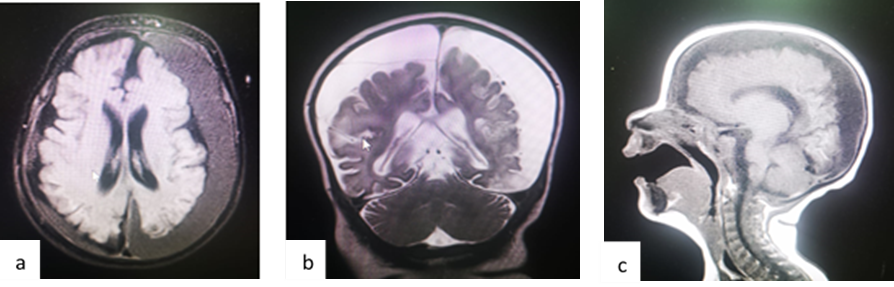
In the nuclear magnetic resonance with contrast (Figure 4), hyperintense lesions are evident, with limited diffusion and a bilateral subdural collection compatible with the post-ECT process, not dependent on drainage or placement of shunts at the time.
Figure 4. Brain magnetic resonance imaging (a and b) in the T1 sequence showed a hypointense collection compatible with bilateral frontoparietal subdural hemorrhage in different stages; (c) in the T2 sequence showed hyperintense lesions in non-contrast-enhancing white matter with limited diffusion.
Given the suspicion of child abuse, it was reported from the beginning to the Chief of staff. The patient was discharged from the hospital setting with prior notice to the case’s judicial authorities. Currently a patient in the custody of the Child Protection Unit who will define, through the judicial process, the classification of the crime of child abuse, and who will have final custody of the infant.
DISCUSSION
The American Pediatric Association recommends the term Abusive Head Injury (AHT) which includes the biomechanics of the injury inflicted by shaking, forceful impact or a combination of these; To date, the term shaken baby syndrome (SBS), named with the triad of cerebral edema, subdural hematoma and retinal hemorrhage, is accepted as a synonym(1).
ED is considered the most serious form of child abuse. This entity occurs in the population under 5 years of age, especially in infants; its diagnosis is a challenge since the symptoms are usually nonspecific and varied, the report is misleading by the tutor, and because it is reported as an accident most of the time, as was the case with our patient(1).
Infants are the most vulnerable population due to the head-to-body ratio, making them susceptible during falls and to suffer more acceleration-deceleration injuries due to their high-water content in the brain(1).
During pregnancy, an emotional mother-child bond develops that increases in the first months of life. The deterioration of this relationship can be affected by prenatal factors (negative feelings towards pregnancy and primiparity) and postnatal factors (postpartum depression)(3). According to the perception of health professionals, there are cultural factors (absolute authority of the father, preference for male children), social (lack of education, stressful lifestyle, children in the care of other relatives), family (low economic status, little parental experience, parents with mental health problems, single-parent family structure) and the patient's own (naughty children or with a congenital defect) that influence child abuse(4). In Peruvian society, these factors are frequent, among them the naturalization and conceptualization of child abuse as a parenting method to avoid “wrong” children(5).
Cases of eating disorders are challenging to determine due to lack of diagnostic suspicion due to misleading reports by the tutor and poorly oriented physical examinations(1). Health professionals recognize that there is an underreporting of them(6). Emergency child abuse screening tools have been developed. However, more studies are needed to estimate their accuracy(7,8).
The antecedent of refusal of hospitalization by the parents, the finding on physical examination of a bony callus in the clavicle, and the images to aid in diagnosing brain trauma and multiple fractures suggest eating disorders in our infant(1).
ED involves brain lesions manifesting alteration of consciousness, such as seizures, coma, or death (1). Although there are no statistics of seizures due to ED in Peru, in the United States, they report that the rate of post-brain trauma seizures is 6,4%(9), and in the case of ED, it reaches 43%(10). Another of the main characteristics of abused children is fractured. In a Korean emergency center, they report that the most common fractures are usually located in the skull, followed by the upper and lower limbs(11). Even only a minority have multiple fractures(11,12). Retinal hemorrhages are part of the SBS triad(1), in which the prevalence, in a North American study, was 63% of children with eating disorders(10).
Brain tomography (TEM) and magnetic resonance imaging (REM) are relevant to determine the severity of head trauma, the treatment, and the prognosis of the infant(13). Subdural hematoma is found in 90% of ED patients, and it is characterized by presenting different stages (acute, subacute, and chronic)(10,13). Hyperdensity, isodensity, and hypodensity in brain TEM suggest an acute, hyperacute, and chronic course, respectively. MRI is more sensitive than TEM in delineating parenchymal damage(14). The neurosurgeon's management aims to evaluate the intracranial pressure (ICP), the Glasgow coma scale (ECG) to avoid secondary brain damage and make the surgical decision if necessary. Continuous monitoring of intracranial pressure in patients with ECG ≤ 8 is limited in patients younger than 1 year, so many neurosurgeons use indirect methods to measure ICP such as measurement of head circumference, fontanel examination, signs ocular and cardiorespiratory. However, there is little scientific evidence(13).
According to the literature, these children present long-term consequences ranging from social disabilities to paralysis(1); however, they are little estimated due to the lack of consensus on the follow-up time in the outpatient clinic(15).
Regardless of the signs and symptoms for which patients are taken to the emergency or medical consultation, the health professional should routinely look for signs of child abuse that remains hidden, as in our case that the patient was admitted for a seizure, to identify the highest number of eating disorders and prevent future disabilities and deaths in children.
CONCLUSION
The diagnosis of child abuse in emergencies is complex. A clinical history directed in searching for child abuse and images to support the diagnosis is essential to identify it.
Author’s contributions: The authors participated in the genesis of the idea, project design, data collection and interpretation, analysis of results, preparation of the manuscript.
Funding Sources: Self-financed.
Conflict of interest: The authors declare that they have no conflict of interest in the publication of this article.
Received: May 14, 2021.
Approved: June 14, 2021.
Correspondence: Consuelo Luna Muñoz.
Address: Hospital Nacional Edgardo Rebagliati Martins, Servicio de Emergencia Pediátrica. Avenida Edgardo Rebagliati Nº490 Jesús María.
Telephone: (+51)999 859 192
E-mail: lunaconsuelo21@gmail.com
BIBLIOGRAPHIC REFERENCES