ARTICULO ORIGINAL
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2021 - Universidad Ricardo Palma10.25176/RFMH.v21i3.3949
CLASSIC HODGKIN LYMPHOMA AT THE EDGARDO REBAGLIATI MARTINS NATIONAL HOSPITAL DURING 2015 TO 2019.
LINFOMA HODGKIN CLÁSICO EN EL DEPARTAMENTO DE ANATOMÍA PATOLÓGICA DEL HOSPITAL NACIONAL EDGARDO REBAGLIATI MARTINS DURANTE LOS AÑOS 2015 A 2019.
María del Pilar Quiñones Ávila1,c , Eugenio Américo Palomino Portilla1,b,c, Dr. Herbert Alejandro Yábar Berrocal1,a,b,c.
1. Servicio de Patología Quirúrgica, Departamento de Anatomía Patológica del Hospital Nacional
Edgardo Rebagliati Martins.
a. Doctorate Degree
b. Masters Degree
c. Pathological Anatomy Specialty
ABSTRACT
Introduction: Hodgkin lymphomas are B-cell lymphoid neoplasms histologically characterized by a mixed inflammatory cellular component and few Hodgkin/Reed-Sternberg neoplastic cells. Classical Hodgkin Lymphoma (CHL) represents 10% of all lymphoma cases and 85% of all Hodgkin Lymphomas. According to the current World Health Organization classification, CHL is divided into 4 types: Nodular Sclerosing (NS), Mixed Cellularity (MC), Lymphocyte-Rich (LR), and Lymphocyte-Depleted (LD). Objetive: We reviewed all cases of Classical Hodgkin Lymphoma in the Pathological Anatomy Department at Edgardo Rebagliati Martins National Hospital during 2015 to 2019, in order to determine the most frequent type, the incidence according to age and gender, phenotypical characteristics and relation to Epstein Barr Virus (EBV). Materials and Methods: We performed a retrospective descriptive case study of Classical Hodgkin Lymphoma and its 4 clinical-pathological types in the Pathological Anatomy Department at Edgardo Rebagliati Martins National Hospital during 2015 to 2019. 72 patients were identified with Classical Hodgkin Lymphoma diagnosis, of which only 64 were selected for the study. The exclusion criteria were the absence of confirmatory immunohistochemical tests and relapse cases. Results: The most frequent type observed was Nodular Sclerosing with 34 cases (53.12%) and the least frequent type was Lymphocyte-Rich with 2 cases (3.12%). Likewise, a predominance in the male gender was observed, with 42 cases, 20 of which were Nodular Sclerosing and 14 not classified, as the most frequent types, and a greater incidence among those 41 to 50 years of age, without detection of the bimodal peak referenced in international literature. The most frequent immunohistochemical profile of Hodgkin/ Reed- Sternberg was CD15 and CD30 positive, with CD45 negative. EBV was present in 36% of cases and is more frequent in the Mixed Cellularity and Lymphocyte-Depleted types. Conclusions: Classical Hodgkin Lymphoma is a group of lymphoid neoplasms with clinical, histological, and phenotypically defined characteristics. It is more frequent in men between 41 and 50 years of age. A complete clinical information and a good biopsy, preferably excisional, is required for an adequate diagnosis. The Nodular Sclerosing type is the most frequent and the Lymphocyte-Rich is the least frequent type. Hodgkin/ Reed- Sternberg cells are usually CD-15 and CD-30 positive and CD-45 negative. The Pax-5 mild positivity allows it to be differentiated from B-cell Non-Hodgkin Lymphomas. EBV is most frequent in Mixed Cellularity and Lymphocyte-Depleted types.
Keywords: Classical Hodgkin Lymphoma, Nodular Sclerosing, Mixed Cellularity, Lymphocyte-Rich, Lymphocyte-Depleted, Epstein Barr virus, immunohistochemistry (fuente: MeSH NLM).
RESUMEN
Introducción: Los Linfomas Hodgkin son neoplasias linfoides de células B, caracterizadas histológicamente por un contexto celular inflamatorio mixto mayoritario y escasas células neoplásicas de Hodgkin/ Reed- Sternberg. El Linfoma Hodgkin Clásico (LHC) representa el 10% de todos los casos de linfoma y el 85% de todos los Linfomas Hodgkin. De acuerdo con la vigente clasificación de la Organización Mundial de la Salud, el LHC se divide en 4 variantes: Esclerosis Nodular (EN), Celularidad Mixta (CM), Rico en Linfocitos (RL) y Depleción Linfocítica (DL). Objetivo: En este estudio revisamos todos los casos de Linfoma Hodgkin Clásico en el Departamento de Anatomía Patológica del Hospital Nacional Edgardo Rebagliati Martins durante los años 2015 a 2019, para determinar la variante más frecuente, la incidencia en cuanto a edad y sexo, características fenotípicas y relación con el Epstein Barr Virus (EBV). Materiales y Métodos: Se realizó un estudio descriptivo retrospectivo de la casuística de Linfoma Hodgkin Clásico en sus 4 variantes clínico - patológicas en el Departamento de Anatomía Patológica del Hospital Nacional Edgardo Rebagliati Martins durante los años 2015 a 2019. Se identificaron 72 pacientes con el diagnóstico de Linfoma Hodgkin Clásico, de los cuales únicamente se seleccionaron para el estudio 64. Los criterios de exclusión fueron la ausencia de pruebas de inmunohistoquímica confirmatoria y los casos de recidiva. Resultados: Se observó que la variante más frecuente correspondió a Esclerosis Nodular con 34 casos (53.12%) y la menos frecuente a la variante Rica en Linfocitos con 2 casos (3.12%). Así mismo se observó una predominancia en el sexo masculino con 42 casos, 20 de ellos con Esclerosis Nodular y 14 no clasificables, como las variantes más frecuentes, y una mayor incidencia entre los 41 y 50 años de edad, sin detectarse el pico bimodal referido en la literatura internacional. El perfil inmunohistoquímico más frecuente de las células Hodgkin/ Reed- Sternberg es CD15 y CD30 positivo, con CD45 negativo. El EBV estuvo presente en el 36% de los casos realizados y es más frecuente en las variedades Celularidad Mixta y Depleción Linfocítica. Conclusiones: El Linfoma Hodgkin Clásico es un grupo de neoplasias linfoides con características clínicas, histológicas y fenotípicas definidas. Es más frecuente en varones entre 41 y 50 años. Para un adecuado diagnóstico se requiere una completa información clínica y una buena biopsia, de preferencia excisional. La variante Esclerosis Nodular es la más frecuente y la Rica en Linfocitos la menos frecuente. Las células Hodgkin/ Reed- Sternberg suelen ser positivas para CD15 y CD30 y negativas para CD45. La positividad tenue del Pax-5 permite diferenciarlo de Linfomas no Hodgkin de Células B. El EBV es más frecuente en las variantes Celularidad Mixta y Depleción Linfocítica.
Palabras Clave: Linfoma Hodgkin Clásico, Esclerosis Nodular, Celularidad Mixta, Rico en Linfocitos, Depleción Linfocítica, Epstein Barr virus, inmunohistoquímica. (fuente: DeCS BIREME).
INTRODUCTION
Lymphomas are a group of hematopoietic neoplasms of which Hodgkin Lymphoma corresponds to a
family of lymphomas with unique characteristics. The first reports of this kind were performed by Thomas
Hodgkin in 1832, however, it was until 1865 that Samuel Wilks, with the acknowledgment of new cases and
Hodgkin’s work, coined the term “Hodgkin’s Disease” in honor of its discoverer, a name used for over a
century and currently termed Hodgkin Lymphoma, according to the current World Health Organization
classification for Lymphohematopoietic Neoplasms.(1)
Hodgkin Lymphomas are divided into 2 large groups, quite different from each other from the
biological, morphological, and phenotypical point of view: Classical Hodgkin Lymphoma and Nodular
Lymphocyte-Predominant Hodgkin Lymphoma. The first, reason of our review, is a B-cell derived monoclonal
lymphoid neoplasm and represents approximately 85% of all Hodgkin Lymphomas(7). It is subdivided into 4 types: Nodular Sclerosing (NS), Mixed Cellularity
(MC), Lymphocyte-Rich (LR), and Lymphocyte-Depleted (LD)(1), each one with its
individual characteristics and that, in common, they are mainly composed of inflammatory cells, made up
of T cells, B cells, histiocytes, plasma cells, neutrophils, eosinophils and mastocytes(13) and in a lesser degree made up of neoplastic cells, called Hodgkin - Reed
Sternberg (HRS) cells, same which can adopt particular morphologies depending on the histological
subtype, among which are lacunar cells from NS. Furthermore, the classic mononuclear Hodgkin cells,
Reed-Sternberg cells that can be binucleated (owl’s eye appearance) or multinucleated and mummified
cells, observed with greater frequency in the other three types(2,12).
It is important to emphasize that the specimen’s morphological and structural evaluation is
fundamental to establish an adequate diagnosis, and, in this sense, the sample characteristics may or
may not favor this diagnosis. When the organ that is evaluated is a complete lymph node, it is possible
to determine if the neoplastic process is intrafollicular, which leans towards Nodular Sclerosing or the
Lymphocyte-Rich types, while if it is interfollicular, it is most likely a Mixed Cellularity type. For a
long time, Nodular Sclerosing was classified based on the relative proportion of neoplastic cells
(lacunar), grade 2 corresponding to the syncytial type, when numerous lacunar cells formed compact
groups without inflammatory cells among them. However, the more frequent worldwide use of core biopsies
and therapeutic protocols have made this unnecessary for the rutinary clinical diagnosis(14.). In that
respect, it has been proposed that the syncytial type is associated with a more aggressive clinical
course, however, more research is required to determine its use in clinical practice(15). Regarding its phenotypical expression, it is also characteristic. The
HRS cells are CD15 and CD30 positive and CD45 negative. However, the expert recommendations suggest that
the initial panel should include: CD3, CD15, CD20, CD30 and Pax5(3,10). When discordant patterns are detected, it is necessary to broaden the
study with antibodies more specific to each cell line and exclude probable differential diagnosis. In
our experience, CD45 is also included in the initial panel given that its negativity guides the
diagnosis of Classical Hodgkin Lymphoma.
On the other hand, since the first reported cases, it was suspected that an infectious agent
could be involved in the development of Hodgkin Lymphoma. The presence of HRS cell with a prominent
nucleolus and perinuclear halo suggests a viral influence. Diverse studies in patients with Hodgkin’s
Lymphoma showed elevated concentrations of Epstein Barr Virus (EBV) antibodies, especially anti
EBNA-2(4). In 1987, Weiss et al. detected EBV DNA in Hodgkin Lymphoma samples
and, later in 1993, Armstrong et al. were able to demonstrate through in-situ hybridization techniques,
the presence of EBER (Epstein Barr-encoded RNA) in the majority of HRS cells in approximately 50% of
Classical Hodgkin Lymphoma cases and, in addition, they express the proteins coded by LMP-1, LMP-2ª y
EBNA-1 genes, a latent viral infection expression pattern(5). In the remaining
50% in which EBV presence was not shown, lkBl gene mutations have been found, a protein complex that
controls DNA transcription and is implicated in the cellular response against stress, cytokines, among
others. However, these mutations are not found in all patients(5). Presently,
it is known that 9p24.1 chromosome mutations are present in the vast majority of Classical Hodgkin
Lymphoma cases, whether it is gaining copies, amplification or polysomes, with amplification being most
frequent in advanced stages and all directly related to overexpression of the PD-L1 y PD-L2 proteins.
(6)
In international literature, not many publications exist regarding Classical Hodgkin Lymphoma in
Peru. One of the first articles by Peruvian authors dated 1966, published in the indexed journal Cancer
Research by doctors Andrés Solidoro, César Guzmán journal in 1973and Alfonso Chang, and following the
emblematic work of Dr. Pedro F. Albújar, with cases compiled from 2 national hospitals in the city of
Trujillo, published in the Cancer. We consider it important to make the caseload of our hospital known
and compare it to other series of cases.
A retrospective descriptive study about the caseload of Classical Hodgkin Lymphoma and its 4
clinical-pathological types was performed in the Pathological Anatomy Department at Edgardo Rebagliati
Martins National Hospital during 2015 and 2019. 72 patients were identified with Classical Hodgkin
Lymphoma diagnosis, of which only 64 were selected for the study. The exclusion criteria were the
absence of confirmatory immunohistochemistry test and relapse cases.
We must emphasize that the majority of cases corresponded to outpatient film evaluation (33
cases), mainly incisional or core biopsies. While inpatient cases (31), were
18 excisional, 7 incisional, 5 core biopsies and 1 endoscopic.
The variables that were considered were the histological type according to patient age and
gender.
All the cases were evaluated with histological sections stained with hematoxylin-eosin and the
immunohistochemical tests were performed with a Ventana automated system. The reactants and antibodies
used were from the Ventana brand: CD3, CD15, CD20, CD30, CD45, Pax-5 and EBV LMP-1, all prediluted
antibodies ready to use.
We proceeded to register the information in an Excel spreadsheet.
The work did not require approval by the institution nor informed patient consent, given that
patient names, biopsy number and any information that violates personal rights is kept in complete
reservation. This work is descriptive and retrospective.
RESULTS
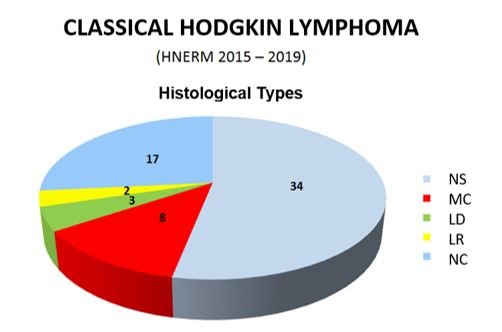
Of the 64 valid cases, 34 correspond to Nodular Sclerosing, 8 Mixed Cellularity, 3 Lymphocyte-Depleted, and 2 Lymphocyte-Rich types. 17 cases were considered as non-classifiable, given taht they presented histological characteristics of more than one type (figure 1).
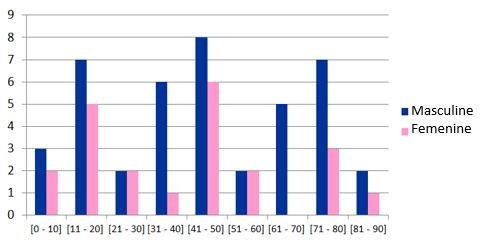
With respect to gender, we found a clear predominance in males, with 42 cases, versus 22 in the female gender (Table 1).
Table 1. Distribution of Classical Hodgkin Lymphoma cases by age group and gender
| Age (years) | N° cases | Percentage | Masculine | Femenine |
|---|---|---|---|---|
| 0-10 | 5 | 7.81 | 3 | 2 |
| 11-20 | 12 | 18.75 | 7 | 5 |
| 21-30 | 4 | 6.25 | 2 | 2 |
| 31-40 | 7 | 10.94 | 6 | 1 |
| 41-50 | 14 | 21.88 | 8 | 6 |
| 51-60 | 4 | 6.25 | 2 | 2 |
| 61-70 | 5 | 7.81 | 5 | 0 |
| 71-80 | 10 | 15.62 | 7 | 3 |
| 81-90 | 3 | 4.69 | 2 | 1 |
| TOTAL | 64 | 100 | 42 | 22 |
However, when we analyze the pediatric population (under 14 years of age), a gender predominance does not exist, and it is in the adolescent population (between 14 and 17 years of age) that we begin to observe a male gender predominance. On the other hand, the characteristic presentation of the bimodal peak in age groups was not observed in our patients, with a greater incidence among 41 to 50 years of age with 14 cases, 8 male and 6 female. After this group, we can observe 2 groups under 12 cases between 11 and 20 years of age and another with 10 cases between 71 and 80 years of age (figura 2).
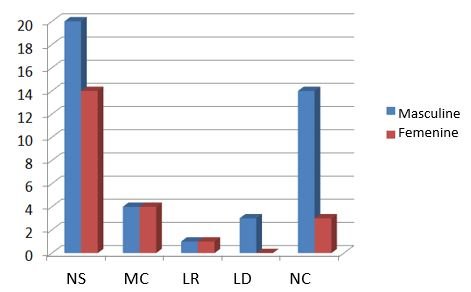
We also observed that in males the Nodular Sclerosing type was more frequent, followed by Non-classifiable and Lymphocyte-Depleted types. While in the Mixed Cellularity and Lymphocyte-Rich types, the number of cases were similar for males and females (figura 3).
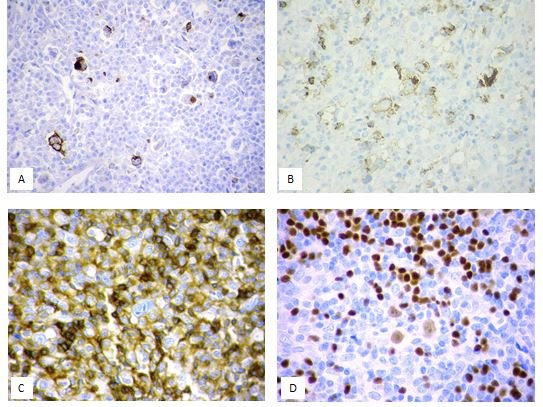
Regarding phenotypic expression of HRS cells, we observed that in the majority of cases the HRS cells expression was CD15 and CD30 positive and CD45 negative. Pax5 was very useful with its characteristic weak expression in neoplastic cells, particularly in cases where CD15 was too weak or even negative. On the other hand, a weak positivity for CD20 was observed in 18.75% of cases (12) and positivity for EBV LMP-1 in 36% of cases, more frequent in men, with a ratio of 2/1 versus women and in the Mixed Cellularity and Non-classifiable types, each with 33.3% of cases.
DISCUSSION
The current study was performed based on the caseload of 5 years (2015 to 2019) of Classical Hodgkin
Lymphoma in Edgardo Rebagliati Martins National Hospital of EsSalud (Social Security), the largest
hospital in Peru. In the international literature, there are no publications regarding this group of
neoplasms in our country.
One of the first articles by Peruvian authors dated 1966, published in the indexed journal
Cancer Research by doctors Andrés Solidoro, César Guzmán journal in 1973and Alfonso Chang, and following
the emblematic work of Dr. Pedro F. Albújar, with cases compiled from 2 national hospitals in the city
of Trujillo, published in the Cancer. They are an inspiration for us who cultivate interest in research
and despite the limited resources we have and little support of our authorities, we persist in our quest
to learn more about our reality and make it known through our publications.
According to international literature, the majority of our cases correspond to the Nodular
Sclerosing type (53.12%), whose diagnosis is suspected from the H-E stained biopsy evaluation, in which
the presence of thick hyaline collagen bands describing nodules from the nodular capsule and the
presence of lacunar cells and other HRS surrounded by a mixed inflammatory infiltrate characterized by
mature lymphocytes, histocytes, plasma cells and eosinophils which complete the cellular composition of
Classical Hodgkin Lymphoma (Figure 1).

|
A. Dense hyaline collagen bands and nodular pattern.
B. Lacunar cells and mixed inflammatory surroundings
Traditionally, NS was graded as NS1 and NS2 based on established histological criteria by Mac
Lennan et al. in 1989, with grade 2 related to the majority of neoplastic cells, creating a syncytial
pattern, associated with necrosis foci and eosinophilic micro abscesses. Currently this grading is not
necessary, however, in advanced cases there has been certain relation with an unfavorable
prognosis.(15) It is important to emphasize that the initial CHL diagnosis
should be performed in an adequate sample, for which fine needle aspiration and core biopsies are not
recommended, given that the architecture is a very important criteria in order to establish an adequate
diagnosis, lymph node excisional biopsies are recommended (7). In recent
years, pathologists receive
smaller samples each time which hinders our diagnosis and often prevents the classification of
neoplasms. In the current work, the majority of the samples studied correspond to incisional and core
biopsies, which prevents their adequate classification, creating an elevated number of cases (17) in the non-classifiable category.
Mixed Cellularity and Lymphocyte-Depleted were the following in frequency, with 8 and 3 cases,
respectively, both types shared certain clinical characteristics and the association with EBV in the
majority of cases. However, from a morphological point of view, MC has a great number of reactive
inflammatory cells and few HRS cells, same that show a classical morphology, while in LD the cellular
component is more fibro histiocytic and numerous HRS cells exist, many of which are pleomorphic. The
Lymphocyte-Rich type is the less frequent type, 2 cases in our series and, unlike the others, present a
cellular component mainly made up of mature lymphocytes, some plasma cells and basically no
eosinophiles. The differential diagnosis of this type is fundamentally with Nodular
Lymphocyte-Predominant Hodgkin Lymphoma, however, the phenotypic expression of HRS neoplastic cells
confirm the diagnosis. In the majority of our cases, according to the international literature, the HRS
cells were CD30 positive, with the typical Golgi pattern and/or membrane and for Pax5 they had a weak
nuclear positivity. CD15 was positive with less intensity and some cases only with a Golgi pattern. CD20
was usually considered as negative in this lymphoma group, however, in recent years a weak positivity in
HRS cells has been reported, with greater frequency in the LR type compared to other CHL types(11). CD45 is a very useful marker in the CHL diagnosis, since the negativity
in HRS cells allows them to be differentiated from its imitators (Fig 2).
Nevertheless, given that many types of lymphomas present neoplastic cells similar to HRS cells, it is usually necessary to expand the immunohistochemical panel with B and T lineage antibodies. On the other hand, it is important to emphasize that the anatomopathological diagnosis is an integrated diagnosis, in which we analyze each patient’s case from the clinical history, therefore it is necessary to count on complete information in each case. In our country, for example, there are lymphomas associated to endemic viruses in certain regions, such as EBV and HTLV-1, therefore, if we do not count on that information, we cannot establish an adequate correlation. Establishing multidisciplinary task force teams are becoming ever more necessary to standardize criteria and move forward in the same direction.
CONCLUSIONS
Classical Hodgkin Lymphoma is a lymphohematopoietic neoplasm with defined clinical, histological and phenotypic characteristics. It is more common in men between the ages of 41 and 50. Good clinical information and a good biopsy, preferably excisional, are required for an adequate diagnosis. The Nodular Sclerosing type is the most frequent and the Lymphocyte-Rich type is the less frequent. EBV was present in 36% of the cases, however the detection was by immunohistochemistry with a non-optimal sensitivity. Later studies with in-situ hybridization techniques for EBER will be necessary in order to establish a real relation in this group of lymphomas.
Authorship contributions The author participated in the design, drafting, review and
approval of the manuscript.
Funding sources: Self-financed
Conflict of interests The author declares not having any conflict of interests in the
publication of this article.
Received: April 01, 2021
Approved: May 17, 2021
Corresponding author: María del Pilar Quiñones Avila
Address: Hospital Nacional Edgardo Rebagliati Martins,Jr.Edgardo Rebagliati
490.Jesús María.
Telephone: (01) 2654901
E-mail: mpilarquinones@gmail.com
BIBLIOGRAPHIC REFERENCES: