ARTICULO REVISIÓN
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2021 - Universidad Ricardo Palma10.25176/RFMH.v21i3.4016
DAMAGE CONTROL APPROACH AND REDUCED RESUSCITATION OF THE POLYTRAUMATIZED PEDIATRIC PATIENT IN THE EMERGENCY ROOM
ABORDAJE DE CONTROL DE DAÑOS Y REANIMACIÓN REDUCIDA DEL PACIENTE PEDIÁTRICO POLITRAUMATIZADO EN URGENCIAS
Augusto Flavio Figueroa-Uribe1,a, Julia Hernández-Ramírez1,b, Gabriela
Mendoza-Besares1,c, Inti Ernesto Bocanegra-Cedillo2,d, Michelle Fabienne
Vela-Díaz Infante1,e, Jorge Omar Flores-del Razo1,f
1Hospital Pediátrico Peralvillo SSCDMX, Ciudad de México México
2Hospital de Traumatología y Ortopedia, IMSS, Monterrey, N.L, México
aPediatric Emergency Specialist, Medical subdirector
bPediatric Nurse, Education Coordinator
cPediatric Emergency Specialist, Chief of Emergency
dPediatric Intensive Care Specialist, Assistant Physician at UMAE No. 21
eEmergency Physician, Assistant Physician to Emergency Department
fPediatric Emergency Specialist, Assistant in Management
ABSTRACT
Polytrauma in pediatric patients is a frequent event, so its timely approach and management define its prognosis. Polytrauma is defined as the presence of two or more traumatic injuries or a single one that endangers life or there is a risk of serious sequelae; resuscitation is understood as the restoration of vital functions of the patient in the pre-hospital area to the hospital area aimed at avoiding the damage caused by the fatal pentad of trauma (coagulopathy, acidosis, hypothermia, hyperglycemia and hypoxemia) for which the damage control protocol was carried out, which is referred as all the maneuvers that have the purpose of preserving life, but without carrying out definitive repairs in order to mitigate complications derived from the prolonged state of shock, secondary to a prolonged surgical time that postponed adequate resuscitation, this reduced resuscitation consists of 6 precise indications for its performance, being approached from the TEP (Pediatric Evaluation Triangle) and the MARCHDEF protocol (Massive Bleeding, Airway, Breathing, Circulation, Hypothermia, Neurological Deficit, Glycemia, Pain, Exposure, FAST).
Keywords: Polytrauma, Damage control, Reduced resuscitation, TEP, MARCHDEF (source: MeSH NLM).
RESUMEN
El politrauma en el paciente pediátrico es un evento frecuente por lo que su abordaje y manejo oportuno definen el pronóstico del mismo. Se define como politrauma a la presencia de dos o más lesiones traumáticas o una sola que pone en peligro la vida o existe el riesgo de secuelas graves; la reanimación se entiende como el restablecimiento de las funciones vitales del paciente en el área prehospitalaria hasta el área hospitalaria encaminados a evitar el daño causado por la pentada mortal del trauma (coagulopatía, acidosis, hipotermia, hiperglicemia e hipoxia) por lo que se realizó el protocolo de control de daños el cual es referido a todas la maniobras que tiene el fin de preservar la vida, pero sin llevar a cabo reparaciones definitivas con el objetivo de mitigar complicaciones derivadas del estado de choque prolongado, secundario a un tiempo quirúrgico prolongado que postergaba la reanimación adecuada, ésta reanimación reducida consta de 6 indicaciones precisas para su realización, siendo abordado desde el TEP (Triangulo de evaluación pediátrica) y protocolo MARCHDEF (Hemorragias masivas, Vía aérea, Respiración, Circulación, Hipotermia, Déficit Neurológico, Glicemia, Dolor, Exposición, FAST).
Palabras Clave: Politrauma, Control de daños, Reanimación reducida, TEP, MARCHDEF. (Fuente: DeCS - BIREME)
INTRODUCTION
When a patient has two or more traumatic lesions or only one that puts their life in danger or at risk of undergoing serious sequelae, we define the concept of polytrauma, cranioencephalic traumatism as the most frequent and often associated to lesions in other parts of the body. Death in a pediatric patient with polytrauma generally occurs within the first minutes after an accident and the most frequent reported causes are lesions to the brain, medulla and major vessels. Only a third of deaths (30%) occur hours aft4er the accident due to hypovolemia, hemorrhage or hypoxia.
Immediate resuscitation
Resuscitation is the reestablishment of the child’s vital functions, in this case, trauma victim
where pre-hospital care is begun to continue to hospital care with the necessary invasive procedures to
diminish and avoid damage caused by coagulopathy, acidosis, hypothermia and hypoxia (1).
This concept was first applied during the Vietnam War where trauma lesions were observed that
caused coagulopathy and acidosis, for which early hemotransfusion with reconstituted blood was proposed.
During the Afghanistan War, in the first decade of the XXI century, patient care with high energy trauma
was systematized and the damage control resuscitation or immediate resuscitation thinking was applied
(1).
In the decade of 1970, the University of Pennsylvania proposed the damage control protocol that
included the patient care with trauma of high energy, multiple fractures and state of exsanguinating
shock, referred to all maneuvers that had the goal of preserving the patient’s life, without taking
definitive repairs since they take time and perpetuate the state of shock and hypothermia in the
patient. Patients died more from prolonged state of shock derived complications, secondary to prolonged
surgical time that postponed the optimal patient resuscitation.
There are six resuscitation indications with damage control:
- Lesion severity, defined by the presence of two lesions or organs or systems that place the patient’s life in danger, the majority of times they are secondary to high energy trauma or have damage severity index greater than 35 points.
- State of exsanguinous shock with a loss of circulating volume in the pediatric patient (80 a 90cc kg) of 28% or more during more than 70 minutes, which could be complicated with consumption coagulopathy.
- Invest time in procedures that don’t improve patient survival or the insufficient medical experience while conducting same.
- Hypothermia less than 34°, acidosis with pH <7,2 and coagulopathy (prothrombin time >19sec, partial thromboplastin time <60 o >60 sec, serum lactate > 5 mmol/L and base deficit > 6mmol/L).
- Failure to block external and internal hemorrhages (intrabdominal or thoracic).
- Presence of associated comorbidities such as diabetes, obesity, cardiopathy, renal insufficiency, malformations, age below 5 years or greater than 60 years (1).
Clinical approach
The recommended model for evaluation consists of a general and initial evaluation of the child through a pediatric evaluation triangle (TEP) and the first, second and third evaluations. The goal was to recognized signs of central nervous system dysfunction, respiratory insufficiency, compensated shock and decompensated shock to promptly intervene and save the patient’s life. If patients are not treated promptly, they can rapidly progress to cardiopulmonary insufficiency whose final outcome is cardiac arrest (2).
The basic care outline is the following:
- General evaluation
-
Primary evaluation (MARCHDF system)
- M. Massive hemorrhages
- A. Airway
- R. Respiration
- C. Circulation
- H. Hypothermia
- D. Neurologic deficit/Capillary glycemia (Destrotix®)/Neurologic incapacity (Glasgow), Pain
- E. Exposure
- F Drugs, FAST, Family.
- Secondary Evaluation (MESIRT System)
- Monitoring
- Craniocaudal exploration
- SAMPLE simplified clinical report
- Referral
- Reevaluation
- Transfer
Use the “evaluate-identify-intervene” model to evaluate and treat the pediatric patient who is
hurt and critical. Performa an initial evaluation and proceed to repeat the evaluation in order to
decide the best treatment and patient intervention. Categorize the clinical status according to the type
and severity, decide and act to initiate treatment. Later, reevaluate and repeat the process
“evaluate-identify-intervene”.
If a potentially deadly inconvenience is identified, proceed to initiate the necessary
interventions to sabe the child’s life and use the evaluation with a systematic approach(1,2,3,4,5).
Pediatric Evaluation Triangle TEP
TEP is an approach for the initial evaluation, specially adapted for children, It is a quick,
simple and useful tool to evaluate children of all ages. It allows the patient characteristics to be
integrated with those of general impression independently from the illness or lesion. TEP has become the
basic evaluation model in national and international programs of vital support (1). It is a simple instrument to begin the evaluation of a child exclusively
based on visual and auditory indices, not requiring a stethoscope, sphygmomanometer, cardiac monitor, or
pulse oximeter. Use the TEP tool wherever the first patient is done, the evaluation should be done in 30
to 90 seconds.
TEP is the evaluation paradigm at first sight. The three components of TEP reflect the general
physiological state of oxygenation, ventilation, perfusion and cerebral function. The components of TEP
are appearance (conscience or unconsciousness, irritability, hyperactivity, hyporeactivity, and
bleeding), circulation (cyanosis, paleness, and marbled skin) and respiratory (apnea, dyspnea, polypnea
or bradypnea). TEP is a tool and not an instrument that helps first contact health personnel offer
support to the patient in an emergency situation.
The three components in TEP (Figure 1) allows the initial evaluation of
cardiopulmonary state,
cerebral function and metabolism of the child, as well as identification of the type and severity of the
physiologic state to initiate treatment as soon as possible (1,2,6).

a.Appearance: Alteration of consciousness or bleeding
b.Circulation: Color, cyanosis, paleness, marbled, etc,.
c.Respiratory: Increase or decrease of respiratory work or abnormal sounds such as stridor or respiratory sounds.
- If the patient presents respiratory difficulty, they will be placed in a comfortable position and administer supplemental oxygen as required, furthermore the specific therapy for the possible etiologies is begun, If the patient presents respiratory insufficiency, the head position, airway permeability are reviewed and oxygen is administered at 100% through bag-mask ventilation as needed. If the patient has foreign bodies, we proceed to extract them. Lastly, we obtain an advanced airway.
- Oxygen is administered for patients with shock.
- In a vital risk situation, it is important to verify the adequate head position, maintain a permeable airway and if necessary proceed to orotracheal intubation, ventilation is initiated with the corresponding device, oxygen at 100% is administered and resuscitation maneuvers are initiated.
Due to TEP being easy and practical to perform and record, it ensures that all health personnel involved in the emergency services “speak the same language”, allowing to rapidly categorize the alteration that the pediatric patient presents. It constitutes the first step to prioritize critical patient care who comes to the emergency room by only responding to the following questions:
- How serious is the pediatric patient’s lesion?
- What is the probable physiological abnormality?
- What is the urgency in the care to initiate treatment?
Primary evaluation
The primary evaluation is the clinical evaluation that consists of a rapid and systematic exploration for the purpose of detecting lesions that constitute a vital risk to the patient. The treatment must be effective and simple.
MARCH-DEF System
An acronym used and accepted by the United States trauma committee for the management and approach of the ten platinum minutes in the pediatric patient and the polytraumatized adult in a conventional and hostile pre-hospital and hospital setting (1,7,8).
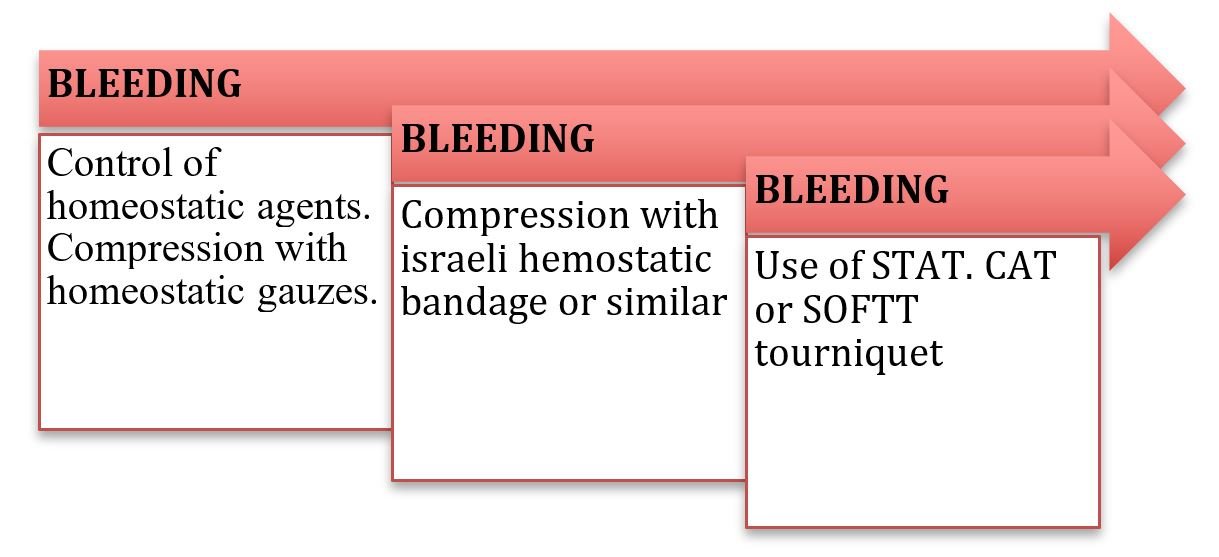
M Massive hemorrhage
The first cause of death within the first hour of trauma care is exsanguinous bleeding that provoked hemorrhagic shock, acidosis, and consumption coagulopathy within a short time. The rapid, effective and efficient control of exsanguinous hemorrhage with compressive agents (turnstiles, compressive bandages, hemostatic gauzes, etc.) and hemostatic agents according to protocol, victim state and place of situation, is priority in polytraumatized patient care. A hemorrhage that compromises a main vessel, artery, or vein, may provoke death within five to ten minutes. Therefore, the hemorrhage management is of maximum priority (9,10).
Systemic hemostatic agents
Tranexamic acid (ATX) is a synthetic derivative of the amino acid lysine and inhibits fibrinolysis
through the blockage of lysine fixation sites in the plasminogen, which could be administered in a wide
gamma of pathologies in the medical care environment.
Children have a reduced blood volume compared to adults and cannot tolerate great losses of
blood volume. However, the lack of cardiac and vascular diseases in them allows a greater compensation
capacity during hemorrhagic shock (10).
The incidence for ATX use in pediatric trauma is low. However, we consider that its
incorporation in the management of pediatric trauma has the potential to significantly reduce mortality
in children and young people without increasing the adverse events, which is why it is suggested to
consider its use.
Its early application is recommended following protocol used in adults. The loading dose of 1g
applied within 10 minutes during the first 3 hours after a lesion, followed by an infusion of 1 g during
8 hours for children over 12 years of age. For those under 12 years of age, the loading dose is 15mg/kg
(maximum dose 1 g) followed by an infusion of 2mg/kg/hour during at least 8 hours or until bleeding
stops. The adverse effects of TXA in pediatrics is rare, however, under the context of trauma we
acknowledge that more research is necessary since some studies have very low levels and grades of
recommendations.
The first measure of care is direct compression with hemostatic gauze or Israeli compressive
bandage (10,11). (Figure 2).
Tourniquets
Few studies have been published in relation to the prehospital experience with tourniquets in
children. The Pediatric Trauma Society supports the use of tourniquets in prehospital environment and
during resuscitation in patients who suffer from exsanguinous hemorrhages (C/D recommendation grade) *.
We must remember that during the Boston attack many victims were children and the first
responders placed tourniquets to various pediatric victims with exsanguinous hemorrhages that saved
lives with this simple intervention. In the year 2012, the TECC (Tactical Emergency Casualty Care)
pediatric guide appeared in which its use is allowed in the pediatric patient.
Children who are victims of violence generally present similar lesion patterns as adults.
Therefore, in them the use of tourniquets may also be indicated with the aim in seeking hemorrhage
control in their extremities. After the Boston attack, the American Academy of Pediatrics recommended
the use of STAT type tourniquet in children.
With the aim of obtaining maximum security and clinical use in pediatric patients from the
different age groups, it is necessary to perform research in the pediatric field to evaluate the size of
the tourniquets taking into consideration the child’s physiological characteristics and other aspects
related with these types of patients. (12).
Absolute clinical indications for immediate tourniquet placement in pediatrics: (Figure 3)
- In amputations of important magnitude with moderate or severe external hemorrhage.
- Important bleeding not controlled by direct compression or hemostatic bandage.
- Multiple bleeding in different spots that don’t allow the optimal application of direct pressure.
- Patients with severe external hemorrhages in extremities that require urgent ventilatory support or airway maintenance.
- Uncontrolled hemorrhage generated by penetrating object. (1,4)
The best way to control bleeding depends on a series of factors such as the victim’s state, and the magnitude and severity of hemorrhage, the proximity to a health department with surgical solving capacity, the simultaneous number of those injured, accessibility of human resource and transportation means, as well as emergency shock unit health personnel training on damage control, since they are who provide the primary assistance in a hospital (12).
Airway
The polytraumatized patient should always be considered as “difficult airway”. It is
mandatory
to administer supplemental oxygen in these patients to maintain oxygenation and prevent hypoxemia.
Airway obstruction is the main cause of avoidable mortality in polytrauma. It is produced in
unconscious patients due to the tongue falling towards the pharynx and in conscious patients due to the
obstruction of airway by blood, vomit, edema, foreign objects or food remains (13).
The first phase of identification is characterized by three alerts:
- Cervical alert
- State of consciousness alert
- Airway alert
Cervical alert
Is referred to the immediate cervical stabilization in which the assistant will keep the head-neck-trunk aligned and immobilized in a neutral position. The neck collar will be placed only if the patient’s present situation does not require intubation.
- If necessary, the instrumental management of the airway will proceed with bimanual immobilization and once the airway is established the collar will be placed.
- It is fundamental to remember that the selective restriction of spinal movements is what has proven to have better results in children (NICE 2016).
- The collar should always be removed to evaluate the neck.
State of consciousness alert
Consists in determining the state of alert in a child, as a general norm every conscious patient that speaks or breaths has a permeable airway. If the patient were unconscious, with abnormal respiratory sounds, irregular breathing or retractions, the instrumental airway management is initiated immediately (13).
Airway alert
If the airway is obstructed, we proceed to unblock through secretion aspiration or removal of foreign objects. To maintain a permeable airway, oropharyngeal cannulas are used. Keep in mind a semi-conscious or conscious patient may present with vomiting or laryngospasms with risk of bronco aspiration. If no improvement is observed, the orotracheal intubation is indicated, with which definite airway control is achieved. Remember it is indicated in different phases of our initial evaluation of the polytraumatized pediatric patient. Remember to apply a rapid sequence of intubation with premedication. The intubation should be performed by removing the collar, immobilizing the cervical column in a bimanual manner and always using a bougie type guide. Other advanced airway management options, in case of not achieving orotracheal intubation, include supraglottic devices, preferably those who posteriorly co-adjuvate the orotracheal intubation (SALT, LMA Fastrack devices, laryngeal tubes), as well as cricothyrotomy in extreme cases (14,15).
R. Respiration
Secure the airway and proceed to immobilize the neck. Then evaluate the patient’s pulmonary function (oxygen and ventilation) and detect signs of severe respiratory insufficiency. Evaluate the organ position to detect the presence of cyanosis, neck congestion, thorax dilation, dyspnea and pulmonary air quality. If symptoms of persistent respiratory insufficiency are present, it is important to rule out the presence of tension pneumothorax before intubating (16). In this stage, it is critical to detect fatal thoracic lesions such as tension pneumothorax, open pneumothorax, or massive pneumothorax. Due to the rapid progression, the diagnosis must be based on clinical evidence, without waiting for radiologic confirmation for treatment. The older the patient and the lower the complexity, the less resistant the pneumothorax is. The ventilator may convert a simple pneumothorax into a tension pneumothorax, and whenever there is a suspicion of tension pneumothorax during hospital treatment, drainage over the puncture should be prioritized (NICE 2016). If this can’t be obtained and/or if the condition is not permitted, an immediate thoracocentesis should be performed ono the second intercostal space, midclavicular line, with a 14 or 16 G catheter coupled to a water seal or Helmich valve that fulfills the same function. In case of open pneumothorax, it should be sealed to avoid tension pneumothorax and convert it to simple pneumothorax that is controlled as previously described. Massive hemothorax correspond to the presence of blood in the pleural cavity causing hemodynamic instability (> 20 cc / kg / hr or > 25% blood volume in pediatric patients). Treatment consists of placing a thoracic drainage tube in the fifth intercostal space along the midaxillary line and perform a potent volume replacement (15).
C. Circulation. Hemodynamic management of damage control.
After securing that the airway is not obstructed and verifying oxygenation and ventilation, the
patient’s circulatory system should be evaluated. First, confirm the location where the compression
device was previously placed, since the hemostatic gauze prevents bleeding. If the bleeding continues,
evaluate the placement of a second tourniquet. If the first is used or a fabric device for compression,
the first tourniquet should be placed. If the patient is amputated, the tourniquet should be immediately
applied (16,17).
Posteriorly, the patient should be clinically evaluated to detect signs of hypovolemic shock and
classify their severity (compensated or uncompensated/ hypotensive), Analyze the following to determine
severity:
- Central and peripheral pulses
- Capillary refill (<4 seconds)
- Temperature
- Heart rate
- Arterial pressure
Currently, the standard vascular Access for patients with multiple critical lesions is the immediate
placement of osteoclysis (intraosseous water). If time and patient conditions allow, two peripheral
lines should be cannulized in the forearm and the use of short and great caliber jelcos are recommended.
When the prior method fails, the third line is the percutaneous line in the femoral vein (18)
Once the venous line is canalized, whether intravenous or intraosseous, a blood sample should be
collected for a complete blood count, cross tests for transfusion and glycemia, the latter using
destroxtis to rule out hyperglycemia or hypoglycemia. The gold standard treatment for traumatic shock
from hypovolemia caused by hemorrhage is the immediate administration of reconstituted blood (NICE
2016). The possibility of applying protocols for balanced massive transfusion should be evaluated using
the ABC classification of massive transfusion. If signs of shock appear, administer liquids to improve
the hemodynamics (19). Restrictive fluid replacement should be managed,
meaning if you do not count on blood use hypertonic saline solution 3% at a dose of 5-10 cc kg in 20
minutes as a second option to avoid the phenomenon of reperfusion and instability of the already formed
clots (“popping the Clot” phenomenon), three doses, if you cannot apply this option then use saline
solution 0,9% at a dose of 20 cc kg during 20 minutes (20).
If hemorrhage is not controlled begin management of permissive hypotension and delayed
resuscitation with hypertonic saline solution 3% from 5 to 10 cc/ kg in 20 minutes with the purpose of
avoiding complications such as consumption coagulopathy, reperfusion syndrome and internal compartment
syndrome. Permissive hypotension method is contraindicated when the patient presents cranioencephalic
traumatism and younger than 5 years of age (17). In patients 5 to 17 years of
age with a head lesion, hypotension permissive measures are prohibited (17).
When each solution bolus is finalized, evaluate the hemodynamic response of the patient exploring again
the cardiovascular clinical data, as well as signs of third spacing (lung). If they don’t present signs
of shock, liquids should be infused according to basal needs. Most probably the patient lost at least
20% of the circulating volume. If they don’t respond, a new bolus of corticoid and/or total blood
transfusion should be assessed if they have it.
Not yet controlled bleeding or occult bleeding should be searched for. In newborns and infants
under 8 kg, intracranial bleeding alone may provoke severe hypovolemic shock as well as concomitant
neurological involvement (7,20).
H. Hypothermia
In children over 10 years of age, hypothermia implies a temperature under 35° and at younger ages hypothermia presents at higher temperatures. Neonates are considered hypothermic if they have a temperature under 37°. In polytraumatized patients, hypothermia has different etiologies, and hydric resuscitation can generate heat loss that is proportional to the mas of administered liquids and to the liquid temperature gradient in the patient. Hypothermia affects all body systems, adverse effects include arrhythmias, decrease in cardiac output and cardiac frequency, increase in vascular resistance, decrease in glomerular filtration rate and sodium absorption, central nervous system depression, etc. Nursing patients and newborns are transferred to a heat source as soon as possible to facilitate body temperature measurement (21).
D. Neurological deficit (disability)/destroxtis (glycemia)/cranial lesion (head and eye injury) pain.
In this section we evaluate the four “D’s”:
- Neurological deficit (Disability). Cranioencephalic traumatism causes primary and irreversible
nervous damage as a direct result of impact. However, it is fundamental to avoid secondary lesion
due to hypovolemia, hypotension, hypoxia and hypercapnia.
The standard evaluations are:- Pupil evaluation through the light pupil response (size, response capacity and symmetry), is an indicator of brainstem function.
- The AVDI (alert, verbal, pain, unconsciousness) pediatric response scale (21,22) allows evaluation of the cerebral cortex function, and
- the Glasgow scale (eye opening, motor and verbal responses) determines the level of consciousness and neurological state of the pediatric patient. If the patient has a score < 8 they should be intubated.
- Anisocoria
- Bradycardia / tachycardia
- Hypertension
- Pupilar hyporeactivity
- Decerebrate or decorticate posturing.
- Rapid Glasgow decrease
Intracranial hypertension signs should be sought: - Glycemia (Destroxtis): If the patient presents hypoglycemia, a bolus of glucose solution at 10% at 2 cc kg dose should be immediately administered.
- Ocular deficit: Ocular lesion, if necessary, cover them with dressings and wait for eye wash during the second evaluation.
- Pain: Pain management is very important since its damaging effects such as oxygen consumption, energy, glucose and increase in intracranial pressure. Therefore, it is necessary to manage pain as soon as possible.
E. Exposure
The final step in the primary evaluation is to prepare for the second evaluation:
The patient must be exposed, their clothing should be removed entirely. Once undressed, a quick
exploration will be performed to localize lesions that cannot wait to be diagnosed during a second
exploration, such as amputations, deformities, exposed fractures or lesions in internal organs. The
patient’s evaluation must be complete (anterior and posterior), the necessary safety measures must be
taken during the patient’s mobilization in order to avoid lesions (21).
F. FAST, Pharmaceuticals and Family
The name of the FAST ultrasound derives from the English acronym Focused Abdominal Sonography for Trauma. It is used in the United States since 1990 and its main objective is to detect free fluid in the abdominal cavity of patients with closed abdominal traumatisms. Six areas are assessed:
- Hepatorenal recess or Morrison’s pouch
- Splenorenal recess
- Bilateral paracolic gutters
- Pelvis
- Pericardium
- Some centers assess the thorax searching for pleural effusion or pneumothorax. The indications for the FAST exam include: Abdominal, blunt or penetrating chest trauma, undifferentiated shock and/or hypotension (as part of the Rapid Ultrasound for Shock and Hypotension (RUSH) exam).
In this phase, the early administration of coadjuvant drugs is administered, such as tranexamic acid, analgesics, and, if necessary, antibiotics, blood components, etc.
Pain and anxiety management in polytraumatized pediatric patients is very important in reducing morbimortality. We begin with ketorolac, fentanyl or buprenorphine depending on the type of lesion and the main hemodynamic and neurologic clinical condition.
Only if necessary, should first line antibiotics be started since one of the causes of death in intensive therapy is sepsis. However, starting antibiotics is not indicated in traumatic lesions, such as burns, if there is no clinical or laboratory information that suggests the presence of an infectious process.
FAMILY
During this time, we should inform the child’s family about the patient’s condition avoiding
minimizing or hiding their state. The informed consent has been framed mainly through the legal and
moral philosophy languages. Therefore, the informed consent legally protects patients from aggressions
and lesions in the form of unwanted medical interventions.
The patient’s state of consciousness is important when receiving information about the illness
and treatment they require. If there is a condition that prevents the acceptance or refusal for
treatment, this information may be presented to a legal representative who will make the decision with
respect to the medical steps to follow. However, the legal standards that apply to obtaining the
informed consent vary from one jurisdiction to another and its interpretation continues evolving. Some
jurisdictions use the reasonable person standard, while others use the oldest reasonable physical person
standard, therefore, it is important that clinicians determine the precise standard used in their
jurisdiction and adapt their practice in an orderly fashion. This way, according to the laws of the
nation in which they reside, it is important to consider life and the wellbeing of the pediatric
patients above any religious discipline against treatment refusal. Blood transfusions generally are
performed in the child’s benefit.
The information given to the patient is an important aspect, it should be of quality and
understandable to the patient, family member or legal representative, avoiding complex terminology, with
the purpose that the family member or legal representative, in the case of pediatric patients, make the
best decision. Therefore, the informed consent is basically a communication process and has to focus on
reassuring the patient, to benefit them and face their illness the best way possible (18,19).
Secondary evaluation
The secondary evaluation only initiates once the primary evaluation has been completed and the
life-threatening lesions have been treated. If, during an examination, any decline is detected, they
need to go back to go over the primary evaluation.
A detailed clinical history and physical exam, diagnostic imaging, and problem identification of
the significant lesions must be performed. Throughout the evaluation, standard precautions for blood or
fluid transmitted infections must be observed.
The MEASIRT methodology may be performed to easily remember the steps to be
followed(18,19).
-
Monitoring
While the team leader performs the primary evaluation, the patient should be monitored since this gives a quick notion of the response to the treatment administered. -
Cephalocaudal exploration
- Head and face. Examination of the head allows to discover a hematoma in the scalp, a depression or laceration in the cranium. The scalp and osseous segment lacerations may only be identified through careful palpation, which is why palpation of the scalp is important, as well as assessing all facial expressions, including the orbit, superior and inferior mandible and the nose.
- Neck. Should be carefully examined, palpated and immobilized. A lesion in the cervical column should be assumed until the contrary is proven, which will be studied through diagnostic imaging of X-rays or computerized tomography. Swelling and acute pain in the throat should be searched for.
- Thorax. Thoracic lesions, in order of frequency in a pediatric patient, are pulmonary contusions, rib fractures, pneumothorax and hemothorax. They should be identified and treated as an emergency in the primary evaluation of massive hemothorax, tension pneumothorax and cardiac tamponade. Pleural effusion due to tension pneumothorax and cardiac paralysis should be detected and treated urgently during the initial evaluation. The entire thoracic wall should be palpated to detect crepitation (subcutaneous emphysema) and sensitivity. The area above the sternum and the clavicles requires spatial attention since the fractures that affect these bones may suggest a significant force and the need for evaluation searching for intrathoracic lesions. Evaluate the presence of respiratory distress, abnormal respiratory and cardiac sounds. Inspect if there is a hematoma related to the safety belt. An X-ray should be taken and in the event of pleural effusion or pneumothorax, the necessary drainage should be performed.
- Abdomen. Subtle signs of closed abdominal trauma from hollow or solid organ should be searched for. These signs are most frequent in the unconscious patient, and we should consider that its absence does not rule out the possibility of a serious abdominal lesion.
- Extremities. The extremities should be evaluated to assess contusions, bleeding, crepitations, deformities, wounds, etc. The integrity of the joints not lesioned by the active and passive movements.
- Back. The patient should be mobilized in blocks to search for back and spine lesions. If neck lesions have not been ruled out, patient should be immobilized.
- Complete neurological exploration. Neurological exploration must
be evaluated in a complete manner reevaluation the initial exploration:
- Consciousness level
- Pupil
- Glasgow scale
- Cranial pairs
- Mobility and muscular tone
- Sensitivity
- Osteotendinous reflexes
-
(Focused clinical history)/Care documentation
In the clinical history we should consider the probability of damage and the forever trauma mechanism and when they are known. The SAMPLE mnemonic application, (signs/symptoms, allergies, medication, prior clinical history, last time they ate or drank and events that led to the current illness), serves to identify antecedents and discomfort that the child presents. This information is useful in determining the decline in respiratory, neurological or cardiovascular function (21,22). -
Referral
Taking into account the findings in the first and second physical evaluation we should assess the referrals to diverse practitioners (pediatric surgeons, neurosurgeons, orthopedics, intensive therapy, plastic surgeons, etc.). Therefore, the decision to transfer a polytraumatized patient after stabilization depends on the availability of these resources (21,22). -
Periodic reevaluation/ X-rays/tomography
During the treatment and stabilization phase, it is necessary that the patient continue with monitoring indicated in the initial exploration. However, we should pay attention to a reiterated patient reevaluation. The polytraumatized pediatric patient may evolve in a rapid form which is why the periodic reassessment is important to promptly detect any complication that may arise (24). Once the patient is stabilized, specific diagnostic imaging tests may be performed, such as imaging, x-rays/ tomography (Tertiary evaluation). -
Transfer
Once we’ve obtained the initial stabilization of a patient with multiple traumas, we should consider asking the trauma hospital to begin treatment of the lesion in primary phase (surgical). The adequate hospital should be assessed. Mainly in our means, it will be a tertiary hospital or a hospital center with experience in pediatric polytraumatized patient management. When the transfer is performed, it will be when the patient finds themselves the most stable possible and have been accepted by the receiving hospital center. A bidirectional communication between the sending hospital, the receiving party and the transport team is required. (24,25).
CONCLUSIONS
Polytrauma is characterized by the presence of multiple lesions and/or a single lesion that is life-threatening, being the cause of death at the moment of the accident or hours later in 30% of patients due to the complications caused by hemorrhage, hypovolemia or hypoxia. The approach in these patients requires directing the attention to the early reestablishing of vital functions of the child performing procedures leading to avoid damage due to coagulopathies, acidosis, hypothermia, hypoglycemia and hypoxia, which is performed through the concept of immediate resuscitation or damage control resuscitation. To perform a general evaluation or clinical approach, we recommend the attention outline with a general evaluation that includes the Pediatric Evaluation Triangle for a diagnostic, rapid and brief evaluation, based on visual and auditive patient guidelines, the Primary Evaluation through the MARCHDF system, for the evaluation and treatment of hemorrhages, airway, breathing, circulation, hypothermia, neurological deficit, cranial lesion, glucometer, exposure and FAST ultrasound and administration of coadjuvant medications in the treatment (hemorrhage control, analgesia). Later a Secondary Evaluation is performed through the MESIRT system that allows a complete patient assessment and exploration from head to toe performing a cephalocaudal exploration and monitoring, for such a clinical history is directed through a pneumonic SAMPLE (signs/symptoms, allergies, prior Medication, previous pathology, food/liquids and last meal and event origin). Referrals are done for a multidisciplinary approach. A periodic re-assessment should be performed, with studies and conclude with the movement of the patient to an adequate trauma center to start damage control in phase 1 which corresponds to the center with greater experience in the management of the pediatric polytraumatized patient. The procedures since the prehospital management to the treatment in the last instance, requires an effective, fluid, bidirectional communication, and a multidisciplinary follow-up (Figure 4).

Whenever a phase is observed, the clinical data assessed and its therapeutic approach in order of priority. This protocol is directed for damage control caused by the mortal triad of trauma before damage control surgery and in order for admission there to be the most stable possible.
Authorship contributions: The authors participated in the creation and design of the
article, data collection and analysis and interpretation of the information, critical revision
and drafting of the final version.
Funding sources: Self-financed.
Declaration of conflicts of interest: The authors declare not having conflicts of
interest in the publication of this article.
Received: May 02, 2021
Approved: June 14, 2021
Correspondence: Augusto Flavio Figueroa Uribe.
Address: Hospital Pediátrico Peralvillo SSCDMX, Calz San Simon 14, San Simón
Tolnahuac, Cuauhtémoc, 06920 Tolnahuac, CDMX – México.
Telephone: 555427275164
E-mail: mandolarian1975@gmail.com
REFERENCIAS BIBLIOGRÁFICAS