CASO CLÍNICO
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2022 - Universidad Ricardo Palma10.25176/RFMH.v22i2.4393
GOLDENHAR SYNDROME ASSOCIATED WITH AN EPIBULBAR DERMOID: CASE REPORT
SINDROME DE GOLDENHAR ASOCIADO CON UN DERMOIDE EPIBULBAR: REPORTE DE CASO
Diego José Mamani Maquera1,2,a, Adriana Palomino Bernal1,3,b
1 Unidad de Órbita y Oculoplástica, Servicio de Oftalmología, Hospital Nacional Carlos Alberto
Seguín Escobedo - EsSalud. Arequipa, Perú
2 Universidad Nacional de San Agustín. Facultad de Medicina, Arequipa, Perú
3 Universidad Católica Santa María. Facultad de Medicina, Arequipa, Perú
a Ophthalmology Resident Surgeon
b Surgeon specialist in Ophthalmology
ABSTRACT
We present the case of a 7-year-old male child with Goldenhar syndrome associated with an epibulbar choristoma. The patient presents a homogeneous tumor, rounded in shape, with well-defined borders, of a soft consistency, vascularized, approximately 9x10 mm, yellowish-white in color, adhered to the sclera and cornea, with hairy formations on its surface, located at the level of the sclerocorneal limbus of the temporal-lower quadrant of his right eye. The histopathology study showed the presence of hair follicles and sebaceous glands, immersed in a stroma of fibrous connective tissue with a superficial squamous-type lining, which defined the diagnosis of limbar epibulbar dermoid. Conjunctivaplasty was performed to cover the scleral defect and use amniotic membrane to cover the corneal and scleral defect. The limbar epibulbar dermoid is the most common type of conjunctival choristoma and should be considered in the differential diagnosis of pediatric epibulbar tumors.
Keywords: Goldenhar syndrome; epibulbar choristoma; epibulbar dermoid. (Source : MeSH - NLM).
RESUMEN
Presentamos el caso de un escolar varón de 7 años con Sindrome de Goldenhar asociado a un coristoma epibulbar. El paciente presenta una tumoración homogénea, de forma redondeada, con bordes bien delimitados, de consistencia blanda, vascularizada, de aproximadamente 9x10 mm, de color blanco–amarillento, adherido a esclera y córnea, con formaciones pilosas en su superficie, ubicada a nivel del limbo esclerocorneal del cuadrante temporal-inferior del ojo derecho. El estudio histopatológico demostró la presencia de folículos pilosos y glándulas sebáceas, inmersas en un estroma de tejido conectivo fibroso con un revestimiento superficial de tipo escamoso, lo cual definió el diagnóstico de dermoide epibulbar limbar. Se realiza conjuntivoplastía para recubrir el defecto escleral y se usa membrana amniótica para recubrir el defecto corneal y escleral. El dermoide epibulbar limbar es el tipo más común de coristoma conjuntival y debe ser considerado en el diagnóstico diferencial de los tumores epibulbares pediátricos.
Palabras Clave: Sindrome de Goldenhar; coristoma epibulbar; dermoide epibulbar. (Fuente: DeCS BIREME).
INTRODUCTION
Goldenhar syndrome (GS), also known as hemifacial microsomia and oculo-auriculo-vertebral dysplasia, was
described by the first time by Von Arlt in 1854 and later named after Dr. Maurice Goldenhar, who
reported 3 cases in 1952. (1,2)
The precise etiology is still unknown, it is a complex developmental disorder during fetal life,
which mainly affects structures of the head and neck derived from the first and second brachial arches.
It is a rare disease and has a prevalence of 1:3500 to 1:7000 live births, it is more common in men than
in women, with a ratio of 3:2 respectively. In 85% of cases, only one side of the face is affected, with
right-sided involvement being the most common. (1,3)
There is no consensus in the literature about the diagnostic criteria for GS. Currently, the
diagnosis depends on the clinical manifestations, which include the classic triad: 1) mandibular
hypoplasia, resulting in facial asymmetry, 2) ocular and auricular malformations, and 3) vertebral
anomalies. Other skeletal, ocular, renal, and cardiac anomalies have been described. (1,4)
In relation to ocular manifestations, they are most commonly represented by colobomas of the
upper eyelid associated with iris/chorioretinal coloboma, epibulbar choristoma (epibulbar dermoid and
conjunctival lipodermoid) and, less frequently, microphthalmia/anophthalmia, strabismus, cataracts or
cleft asymmetry eyelids. (5,6)
Epibulbar dermoid represents one of the most common forms of the various ocular manifestations
that occur in GS; It can be eccentric or limbal and has the following characteristics: it is a soft,
localized, elevated, opaque, yellowish-white mass at the limbus, with full-thickness corneal
involvement, sometimes with hair follicles on the surface. The most common location is
temporal-inferior, but choristomas of the nasal limbus have been reported. It is necessary to determine
the extent of the lesion, if there is suspicion of intraocular involvement, it is decided to perform an
ultrasonic biomicroscopy (UBM); if orbital extension is suspected, computed tomography (CT) or magnetic
resonance imaging (MRI) may be performed. (5,7)
The treatment of the epibulbar dermoid can be conservative (periodic observation) or surgical,
depending on the size and the involvement of the cornea and anterior chamber. Regarding surgical
treatment, a combination of excision, lamellar keratoplasty and amniotic membrane resurfacing, and
limbal stem cell transplantation is recommended. The goal of treatment is to prevent amblyopia (caused
by irregular astigmatism or visual axis obstruction) or by cosmetic considerations. (7,8)
We present the case of a patient with a Goldenhar Syndrome diagnosis, carrier of an epibulbar
limbal dermoid in the right eye (RE), we discuss the surgical management and postoperative evolution.
The relatives authorized the publication of the clinical case and explicit photographs through informed
consent.
CASE PRESENTATION
A 7-year-old male schoolboy from Arequipa, diagnosed with Goldenhar Syndrome, who underwent surgery on several occasions for multiple congenital malformations (cleft lip, preauricular appendages, and mandibular hypoplasia), whose mother reported a tumor in the RE present since birth. birth, which has been increasing in size over the last few years, and which causes tearing and difficulty closing the eyelid of the RE. (Figure 1).

(Source: Clinical History)
On ophthalmological examination, he presented a best corrected visual acuity (BCVA) of 20/70 in the right eye (RE) and 20/20 in the left eye (LE). An intraocular pressure of 13 mmHg in the RE and 12 mmHg in the LE is found. Examination of the anterior segment of the RE revealed a homogeneous tumor, round in shape, with well-defined borders, soft, vascularized, approximately 9x10 mm, yellowish-white in color, adhered to the sclera and cornea, with hairy formations in the its surface, located at the level of the sclerocorneal limbus of the temporal-inferior quadrant; no alterations were found in the LE during the evaluation (Figure 2). There were no abnormalities in the intrinsic or extrinsic ocular motility tests and normal Cover Test. The fundus examination was normal in both the RE and the LE.

(Source: Clinical History)
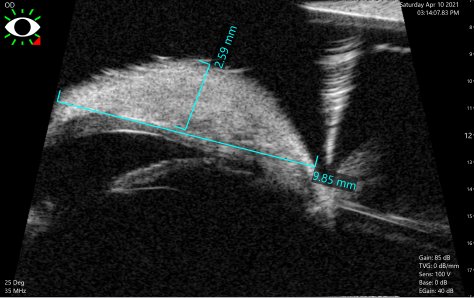
An image study with CT of the RE orbit is requested, which rules out orbital involvement. The UBM of RE shows that at the level of the temporal-inferior quadrant, on the corneal surface there is a homogeneous lesion, with defined borders, of approximately 2.59 mm in maximum height and 9.85 mm in extension, with a cleavage plane between the corneal tissue and the lesion whithout signs of infiltration of the cornea or the anterior chamber. Thinning of the corneal tissue under said lesion is also observed, ranging from 0.39 mm to 0.42 mm (Figure 3).
(Source: Clinical History)
Due to the characteristics described, a benign corneal-conjunctival tumor is proposed as a possible
diagnosis: limbal epibulbar dermoid. A sclerotomy and lamellar keratectomy with a No. 15 scalpel blade
are performed to remove the epibulbar tumor for cosmetic purposes and to reduce the risk of amblyopia.
The ocular surface defect is reconstructed, conjunctivoplasty is performed to cover the scleral defect
and amniotic membrane is used to cover the corneal and scleral defect, the latter is fixed to the
perilimbar conjunctiva with 10/0 nylon.
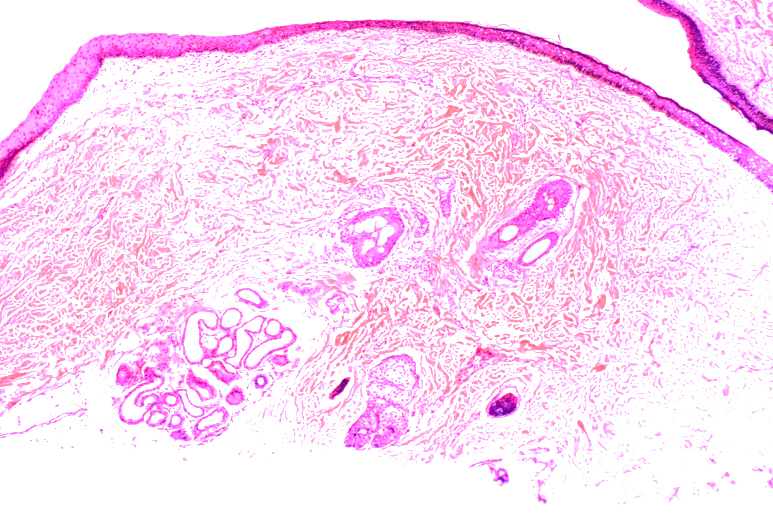
The sample is sent to the Pathological Anatomy Service, the microscopic analysis reports
subepithelial fibrous tissue, with hair follicles, sebaceous glands surrounded by conjunctival
epithelium and moderate perifollicular lymphocytic infiltrate compatible with the diagnosis of an
epibulbar limbal dermoid-type conjunctival choristoma (Figure 4).
(Source: Clinical History)
Postoperative treatment with Ciprofloxacin and topical Dexamethasone for three weeks is indicated.
Postoperative evolution was satisfactory. The stitches were removed at three weeks, by which time the
ocular surface had regenerated and the amniotic membrane had disintegrated. There were no postoperative
complications.
Three months later, the clinical evolution is favorable: he is asymptomatic, on physical
examination the BCVA of the RE is 20/30, the formation of an avascular corneal leukoma in the
temporal-inferior quadrant is evident, corresponding to the area affected by the tumor, conjunctiva
normal in appearance, no signs of recurrence of the lesion can be seen (Figure 5).

(Source: Clinical History)
DISCUSSION
Epibulbar choristoma represents normal tissue proliferating in an abnormal location; It is a rare
entity, with a reported incidence between 1/10,000 and 1/30,000. Histopathologically, they are
classified into 4 groups: dermoids, dermolipomas, complex choristomas, and single-tissue choristomas.
Limbal epibulbar dermoid is the most common type of epibulbar choristoma; it is characterized by being
well circumscribed, being a dome-shaped keratinized limbal mass and being located inferotemporally
(9,10), as in the present case.
Epibulbar choristomas are normally characterized by being sporadic and can develop alone,
however, they can occasionally appear associated with different systemic syndromes, such as Goldenhar
syndrome, epidermal nevus syndrome, Haberland syndrome, oculo-cerebro-cutaneous syndrome and oculodermal
syndrome. (11), in the present case it was associated with Goldenhar
Syndrome.
These lesions can cause amblyopia and strabismus, although with early identification and
excision of limbal epibulbar dermoid lesions, amblyopia and strabismus can be avoided, and thus improve
the visual prognosis of patients with Goldenhar syndrome (12), as happened in
the present case.
The anatomopathological study showed the presence of hair follicles and sebaceous glands,
immersed in a stroma of fibrous connective tissue with a superficial scaly-type coating, as mentioned in
the literature. (13,14)
Infiltration of the cornea and sclera by these tumors is rare, and in these cases excision of
the lesion and reconstruction by means of a conjunctivoplasty is not usually sufficient; in these cases
amniotic membrane coverage is indicated. (12,15)
The amniotic membrane is used to act as a substrate for the migration of epithelial cells, which
can easily replicate, and achieve regeneration of the conjunctival-corneal epithelium and also
reconstruction after the removal of both malignant and benign tumors (15,16), due to all these characteristics we resorted to amniotic membrane
coverage in the present case.
CONCLUSION
Goldenhar syndrome is rare and has a very varied spectrum presentation among patients. This pathology is
characterized by an abnormal development of several craniofacial structures, such as the eyes, which
have epibulbar choristomas as their classic presentation.
As it is a congenital pathology, manifestations should be taken into consideration early and
assess how to worsen normal visual development.
Limbal epibulbar dermoid is the most common type of epibulbar choristoma and should be
considered in the differential diagnosis of epibulbar tumors located in the temporal-inferior quadrant.
Histopathological study is important to confirm the diagnosis and rule out malignant lesions.
Excision of the tumor is indicated in the presence of symptoms or in case of progressive growth; In
cases of extensive tumors, the use of amniotic membrane coating is indicated, due to its regeneration
properties of the conjunctive-corneal epithelium and being a substrate for the migration of epithelial
cells.
Authorship contributions: The authors carried out the design, data collection,
preparation, critical review and approval of the final version of the article.
Funding sources: Self-financed.
Conflicts of Interest: The authors declare that they have no conflicts of interest in the
publication of this article.
Received: June 12, 2022
Approved: December 17, 2022
Correspondence: Diego José Mamani Maquera
Address: Calle Ronda Recoleta 303 – Yanahuara – Arequipa.
Telephone number: 942943535
E-mail: md.diegojose@gmail.com
REFERENCES
