ARTICULO DE REVISION
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2021 - Universidad Ricardo Palma10.25176/RFMH.v22i1.4398
IMPACT OF MODERATE PHYSICAL EXERCISE ON SLEEP DISORDERS IN PATIENTS WITH FIBROMYALGIA
REPERCUSIÓN DEL EJERCICIO FÍSICO MODERADO SOBRE LOS TRASTORNOS DEL SUEÑO EN PACIENTES CON FIBROMIALGIA
Sylvia Gabriela Alfaro-Castro1,a
1 Facultad de Medicina Humana, Universidad Ricardo Palma. Lima – Perú.
2 Medical Student.
ABSTRACT
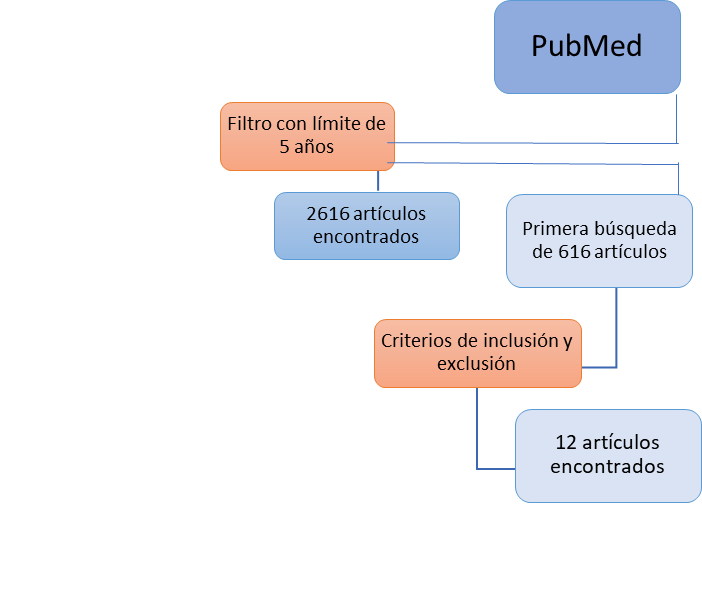
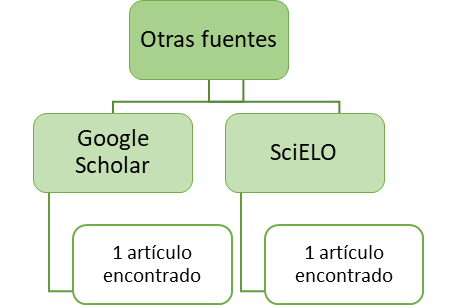
Introduction: Fibromyalgia (FM) or Fibromyalgia Syndrome (FMS) is currently defined as a chronic condition of unknown cause characterized by generalized pain, among other symptoms, in the absence of a specific organic disease. Sleep disorders are recognized as one of the main symptoms in fibromyalgia patients, and performing various types of physical activity in this group of patients could improve sleep quality and other sleep disorders. Objective: To determine if the performance of moderate physical exercise has a positive impact on sleep disorders in patients with fibromyalgia. Methods: A PubMed search was carried out, where 2616 articles were found in the last 5 years, after applying the inclusion and exclusion criteria, and in a first search of 616 articles, 12 useful articles were obtained; using other search engines such as Google Scholar, SciELO, the number of articles obtained was 2; adding a total of 14 articles. Results: The 14 studies reviewed showed that moderate physical exercise reduces sleep disorders in patients with fibromyalgia, 02 suggest individualized treatment, 02 mention that sedentary lifestyle aggravates symptoms, 04 found benefits in complementing exercise with yoga or balneotherapy, and 01 additionally, supports high intensity interval training. Conclusion: The conclusion of this review article was that the performance of moderate physical activity in patients with fibromyalgia has a beneficial impact on regulating and even modifying sleep disorders.
Keywords: Fibromyalgia, Physical exercise, Sleep disorders, Treatment, Lifestyle. (fuente: MeSH NLM).
RESUMEN
Introducción: La fibromialgia (FM) o Síndrome de Fibromialgia (SFM) se define actualmente como la afección crónica de causa desconocida caracterizada por dolor generalizado, entre otros síntomas, en ausencia de una enfermedad orgánica específica. Los trastornos del sueño son reconocidos como uno de los síntomas principales en los pacientes con fibromialgia, y la realización de diversos tipos de actividad física en este grupo de pacientes podría mejorar la calidad de sueño y otros trastornos del sueño. Objetivo: Determinar si la realización de ejercicio físico moderado repercute positivamente sobre los trastornos del sueño en pacientes con fibromialgia. Métodos: Se realizó la búsqueda en PubMed, donde se hallaron 2616 artículos en los últimos 5 años, después de aplicar los criterios de inclusión y exclusión, y en una primera búsqueda de 616 artículos, se obtuvo 12 de utilidad; mediante otros motores de búsqueda como Google Scholar, SciELO, el número de artículos obtenidos fue 2; sumando un total de 14 artículos. Resultados: Los 14 estudios revisados demostraron que el ejercicio físico moderado reduce los trastornos del sueño en pacientes con fibromialgia, 02 sugieren tratamiento individualizado, 02 mencionan que el sedentarismo agrava los síntomas, 04 encontraron beneficios en complementar el ejercicio con yoga o balneoterapia y 01 adicionalmente, apoya el entrenamiento a intervalos de alta intensidad. Conclusión: La conclusión del presente artículo de revisión fue que la realización de la actividad física moderada en pacientes con fibromialgia repercute de manera benéfica regulando e incluso modificando los trastornos del sueño.
Palabras Clave: Fibromialgia, Ejercicio físico, Trastornos del sueño, Tratamiento, Estilo de vida. (fuente: DeCS BIREME).
INTRODUCTION
Fibromyalgia (FM) or Fibromyalgia Syndrome (FMS) is currently defined as a chronic condition of unknown cause characterized by generalized pain, stiffness and sensitivity in muscles, ligaments and joints, associated with fatigue, sleep disorders, cognitive impairment, depression and anxiety, in the absence of a specific organic disease (1,3).
Currently, the diagnosis is based on the sum of diverse symptoms that the patient presents, without the need of meeting a minimum of sensitive points or trigger points, different from the previously mentioned form of diagnosis that existed for over a decade (4).
Prevalence is 2-4% of the general population, most frequent among young adult women. Although the cause is unknown, diverse authors pose that alterations in some neuroendocrine transmitters such as substance P, cortisol, growth hormone, and serotonin, as well as the poorly regulated autonomic system, with exacerbated central sensitization and hypofunction of the inhibitory pain pathways(5), could be interrelated to conduct a decrease in pain umbral and amplify the signals that produce them, modifying the organism’s response to stress(6). Furthermore, we found a marked deterioration of the hypothalamic-pituitary-adrenal axis (HPA)(7).
On the other hand, sleep disorders, known as one of the main symptoms in patients with fibromyalgia, may have a direct implication in its pathogenesis. In electroencephalographic exams(1), we observed that the fourth sleep stage is decreased in patients with fibromyalgia and its importance is due to the secretion of growth hormone (GH) and insulin-like growth factor 1 (IGF-1) during this stage, both implicated in the recovery of muscular microtraumatisms. Therefore, the muscular tissue healing could be affected by sleep disorders.
As we obtain more information on this pathology and in light of the increase number of cases through the years, Larsson et al(8) posed, from the patient’s point of view, a desire for a good quality of life, but most importantly, they express a real need to count on a professional that guides and supports them in the process of starting an active lifestyle since the nature of this illness creates a challenge.
For this reason, the importance of a study lies in determining if moderate physical exercise as part of lifestyle in people with fibromyalgia reduces sleep disorders, considering that these are one of the main symptoms of the clinical presentation in this group of patients. Therefore, delving in this topic and proving the benefits of physical exercise on sleep disorders and pain intensity, in addition to having an impact on the broad range of symptoms present in this pathology, could be considered as a fundamental pillar in the treatment of patients with fibromyalgia, given that it would improve their quality of life.
The objective of the following review article is to determine if moderate physical exercise has a positive impact on sleep disorders in patients with fibromyalgia.
METHODS
The question posed in the following review article was What is the impact of moderate physical exercise on sleep disorders in patients with fibromyalgia? The PECO question is: P: patients with fibromyalgia, E: moderate physical exercise, C: no physical exercise or excessive physical exercise, O: impact on sleep disorders.
We carried out a systematic review search in pages such as PubMed, SciELO, Google Scholar (See annex n° 1) to carry out the presentation of the following article.
The inclusion criteria were the following: studies dating maximum 10 years, studies carried out in patients with diagnosis of fibromyalgia, moderate physical activity, studies on the effects of moderate physical activity on sleep disorders in patients with fibromyalgia, studies on the effects of moderate physical activity on pain level in patients with fibromyalgia. We excluded studies performed on individuals with additional diagnosis other than fibromyalgia and/or comorbidities, studies that did not mention the impact on sleep disorders, studies performed in patients with recent changes in pharmacological treatment, studies performed through use of physical agents such as TENS, infrared, ultrasound for pain management.
Tabla 1. Terms used in systematic search
| P | Participants | Fibromyalgia | “Fibromyalgia”[mh] OR Fibromyalgias*[tiab] OR Fibromyalgia-Fibromyositis Syndrome*[tiab] OR Fibromyalgia Fibromyositis Syndrome*[tiab] OR Fibromyalgia-Fibromyositis Syndromes*[tiab] OR Syndrome, Fibromyalgia-Fibromyositis*[tiab] OR Syndromes, Fibromyalgia-Fibromyositis*[tiab] OR Rheumatism, Muscular*[tiab] OR Muscular Rheumatism*[tiab] OR Fibrositis*[tiab] OR Fibrositides*[tiab] OR Myofascial Pain Syndrome, Diffuse*[tiab] OR Diffuse Myofascial Pain Syndrome*[tiab] OR Fibromyositis-Fibromyalgia Syndrome*[tiab] OR Fibromyositis Fibromyalgia Syndrome*[tiab] OR Fibromyositis-Fibromyalgia Syndromes*[tiab] OR Syndrome, Fibromyositis-Fibromyalgia*[tiab] OR Syndromes, Fibromyositis-Fibromyalgia*[tiab] OR Fibromyalgia, Secondary*[tiab] OR Fibromyalgias, Secondary*[tiab] OR Secondary Fibromyalgia*[tiab] OR Secondary Fibromyalgias*[tiab] OR Fibromyalgia, Primary*[tiab] OR Fibromyalgias, Primary*[tiab] OR Primary Fibromyalgia*[tiab] OR Primary Fibromyalgias*[tiab] |
| E | Exposure | Physical exercise | “Exercise”[mh] OR Exercises*[tiab] OR Physical Activity*[tiab] OR Activities, Physical*[tiab] OR Activity, Physical*[tiab] OR Physical Activities*[tiab] OR Exercise, Physical*[tiab] OR Exercises, Physical*[tiab] OR Physical Exercise*[tiab] OR Physical Exercises*[tiab] OR Acute Exercise*[tiab] OR Acute Exercises*[tiab] OR Exercise, Acute*[tiab] OR Exercises, Acute*[tiab] OR Exercise, Isometric*[tiab] OR Exercises, Isometric*[tiab] OR Isometric Exercises*[tiab] OR Isometric Exercise*[tiab] OR Exercise, Aerobic*[tiab] OR Aerobic Exercise*[tiab] OR Aerobic Exercises*[tiab] OR Exercises, Aerobic*[tiab] OR Exercise Training*[tiab] OR Exercise Trainings*[tiab] OR Training, Exercise*[tiab] OR Trainings, Exercise*[tiab] |
| O | Outcome | Sleep disorders | “Sleep Wake Disorders”[mh] OR Disorder, Sleep Wake*[tiab] OR Disorders, Sleep Wake*[tiab] OR Sleep Wake Disorder*[tiab] OR Wake Disorder, Sleep*[tiab] OR Wake Disorders, Sleep*[tiab] OR Subwakefullness Syndrome*[tiab] OR Subwakefullness Syndromes*[tiab] OR Syndrome, Subwakefullness*[tiab] OR Syndromes, Subwakefullness*[tiab] OR Sleep Disorders*[tiab] OR Disorder, Sleep*[tiab] OR Disorders, Sleep*[tiab] OR Sleep Disorder*[tiab] OR Sleep-Related Neurogenic Tachypnea*[tiab] OR Neurogenic Tachypnea, Sleep-Related*[tiab] OR Neurogenic Tachypneas, Sleep-Related*[tiab] OR Sleep Related Neurogenic Tachypnea*[tiab] OR Sleep-Related Neurogenic Tachypneas*[tiab] OR Tachypnea, Sleep-Related Neurogenic*[tiab] OR Tachypneas, Sleep-Related Neurogenic*[tiab] OR Long Sleeper Syndrome*[tiab] OR Long Sleeper Syndromes*[tiab] OR Sleeper Syndrome, Long*[tiab] OR Sleeper Syndromes, Long*[tiab] OR Syndrome, Long Sleeper*[tiab] OR Syndromes, Long Sleeper*[tiab] OR Short Sleeper Syndrome*[tiab] OR Short Sleeper Syndromes*[tiab] OR Sleeper Syndrome, Short*[tiab] OR Sleeper Syndromes, Short*[tiab] OR Syndrome, Short Sleeper*[tiab] OR Syndromes, Short Sleeper*[tiab] OR Short Sleep Phenotype*[tiab] OR Phenotype, Short Sleep*[tiab] OR Phenotypes, Short Sleep*[tiab] OR Short Sleep Phenotypes*[tiab] OR Sleep Phenotypes, Short*[tiab] |
RESULTS
A PubMed search was carried out with the use of syntax as mentioned before, where 2616 articles were found in the last 5 years, of which, after applying the inclusion and exclusion criteria, in a first search of 616 articles, 12 useful articles were obtained. Through the use of other search engines such as Google Scholar and SciELO, after applying the inclusion and exclusion criteria, the number of articles obtained was 01 from each source.
Of the articles found, 05 were randomized controlled trials, 02 were prospective cohort studies, 02 were analytical-experimental studies, 01 was a cross-sectional study, 02 were observational studies, and 02 were systematic reviews
Tabla 2. Characteristics and results of systematic review.
| TYPE OF STUDY | YEAR | AUTHORS | TITLE | IMPORTANCE | RESULTS | STRENGTHS | WEAKNESSES |
|---|---|---|---|---|---|---|---|
| Randomized controlled single-blind trial | 2020 | Ceca, D et al | Effectiveness of a self-myofascial conditioning programme on pain, depression, anxiety and sleep quality in people with Fibromyalgia | Demonstrated significant decrease in general pain, level of anxiety and depression, as well as in three subscales of sleep quality. | Subjective sleep quality (P<0.05) Usual sleep efficiency (P<0.05) Daily disfunction (P<0.001; η2p=0.277) | Shows auto-myofascial conditioning effectiveness in the decrease of pain, depression, and sleep disorders. | Requires participant time and commitment due to drop-out risk. |
| Randomized controlled single-blind trial | 2020 | Villafaina, S et al | Effect of Exergame Training and Detraining on Lower-Body Strength, Agility, and Cardiorespiratory Fitness in Women with Fibromyalgia: Single-Blinded Randomized Controlled Trial. | The intervention duration could have changed the patients’ lifestyle. | Chair stand (p = 0,017) Walk test 6 min (p =0,011) Stair climb test with 10 steps (p=0,666) | Improvement lasted up to 24 weeks. | Difficult adherence to this type of physical activity, Focused on cardio respiration. |
| Randomized controlled single-blind trial | 2017 | Kim et al | Sustained Benefits of Exercise-based Motivational Interviewing but Only among Non-users of Opioids in Patients with Fibromyalgia. | There was an improvement in physical function, decrease in pain intensity and overall fibromyalgia severity. | Improvement in pain severity P <0,05 | Motivational interviewing favors lifestyle changes. Some participants reduced the use of opioids. | It does not explain which are the changes in sleep disturbances. |
| Randomized controlled single-blind trial | 2016 | Kurt, EE et al | Which Non Pharmacological Treatment is More Effective on Clinical Parameters in Patients with Fibromyalgia: Balneotherapy or Aerobic Exercise? | Physical exercises + Balneotherapy have very positive effects in the sleep quality of patients with fibromyalgia. | Sleep quality (p<0,001) | Another non-pharmacological treatment alternative with favorable results. | Limitations in accessing a treatment with this combination. |
| Randomized controlled single-blind trial | 2016 | Ericsson, A et al | Resistance exercise improves physical fatigue in women with fibromyalgia: a randomized controlled trial | Improvement in quality of sleep was a predictor in the decrease of fatigue among women with fibromyalgia. | Sleep subscale MFI-20 (beta = -0,54, p= 0,031, R2 = 0,05). | Study is centered on fatigue, an important symptom in this disease. | Does not consider other symptoms present in fibromyalgia. |
| Prospective cohort study | 2019 | Skarpsno et al. | The joint effect of insomnia symptoms and lifestyle factors on risk of self-reported fibromyalgia in women: longitudinal data from the HUNT Study | There is a direct relationship between sleep disorders and fibromyalgia risk, with significant differences regarding physical activity performed. | RA de 3,3%. | Applied to a great sample with classic symptoms of this disease especially regarding sleep. | There was no long term follow up on the benefits on sleep quality and greater physical activity. |
| Prospective cohort study | 2018 | Joustra et al | Physical Activity and Sleep in Chronic Fatigue Syndrome and Fibromyalgia Syndrome: Associations with Symptom Severity in the General Population Cohort LifeLines | Patients with Fibromyalgia and Chronic Fatigue Syndrome had a lower scored of physical activity and greater sleep duration. | (9541 +- 5533; p<0,001) | There is a direct relationship between greater sleep duration and severity of symptoms in these patients. | More research is needed to corroborate this data. |
| Analytical experimental study | 2019 | Lazaridou, et al. | Impact of daily yoga-based exercise on pain, catastrophizing, and sleep amongst individuals with fibromyalgia | Suggest that yoga could decrease pain, fatigue, and in some patients sleep disorders. | Decrease on sleep disorders (Rho: –0.40, p =0.03) | Yoga is a type of physical activity of greater acceptance among patients with chronic pain. | Had a beneficial effect in sleep disorders in only one percentage of patients. |
| Analytical experimental study | 2016 | Hackshaw et al | A pilot study of health and wellness coaching for fibromyalgia | Health and wellness training decreased medical care. | P= 0.006 | Less need for medical, pharmacological treatment in patients with fibromyalgia. | Access to this therapy is limited. |
| Cross-sectional study | 2020 | Segura-Jiménez et al | Sedentary Time Accumulated in Bouts is Positively Associated with Disease Severity in Fibromyalgia: The Al-Ándalus Project | A greater percentage of ST in episodes of 30 and 60 minutes is associated with a poorer function and disease severity. | (P<0,05) | The use of measurement elements allowed us to quantify the inactivity time | The study does not allow to establish a causal relationship. |
| Prospective observational study | 2020 | Bodéré C, et al | A training program for fibromyalgia management: A 5-year pilot study | Moderate intensity continuous training (MICT) and high impact interval training (HIIT) as treatment for fibromyalgia. | Active group (p <0,001) after year 3 | Participants that completed the study confirmed improvement. | High percentage of study withdrawal due to study time. (5 years) |
| Observarional study | 2013 | Olsen et al | Relationship between Sleep and Pain in Adolescents with Juvenile Primary Fibromyalgia Syndrome | If a relationship exists between sleep disorders and greater presence of pain. | Pain decreased (P = 0,000) and the subjective quality of sleep improved (P = 0,008) | A study that helps to improve treatments. | Requires more research. |
| Systemic review | 2014 | Li et al | Massage Therapy for Fibromyalgia: A Systematic Review and Meta-Analysis of Randomized Controlled Trials | Improves anxiety, depression, and pain intensity, but not sleep disorders. | (DME, 0,19; IC del 95%: -0,38 a 0,75; p = 0,52). | Complementary alternative to already established treatments. | Only evaluates massage therapy. | Systemic review | 2012 | Demirbag, Erci | The Effects of Sleep and Touch Therapy on Symptoms of Fibromyalgia and Depression | Touch therapy, aromatherapy, and music may be beneficial. | (P <0,05) | Complementary alternative to already established treatments. | Its application cannot be carried out without other treatments. |
Randomized controlled trial study:
A study performed by Ceca, D; et al.(9), titled Effectiveness of a self-myofascial conditioning program on pain, depression, anxiety and sleep quality in people with Fibromyalgia showed a significant decrease in general pain, level of anxiety and depression, as well as three subscales related with sleep quality, such as “subjective sleep quality” (P<0.05; η2p = 0.144), the “ sleep efficiency” (P < 0.05; η2p = 0.129) and “daily disfunction” (P < 0.001; η2p = 0.277) which translated into a physical and psychological benefit for this group of patients improving their quality of life.
Villafaina, S; et al(10) observed beneficial changes in the decrease of daily inactivity time, improvement in sleep quality, in quality of life and cardiorespiratory aptitude in a group of women with fibromyalgia who underwent an exergame type training during 24 weeks. After training the improvements were sustained wich is considered that the duration of the study could influence in a permanent lifestyle change
Another important marker in the increase of sleep alterations is the use of opioids which is why Kim et al(11), carried out a trial to assess the efficacy of the motivational interview in promoting light to moderate physical activity in patients with fibromyalgia and that this, in turn, decrease the use of these drugs. Furthermore, constant physical activity as part of lifestyle reduces pain severity and improves the main symptoms such as depression, anxiety, and diverse sleep alterations.
Following the list of benefits that physical activity grants to patients with chronic pain, Kurt et al(12) proposed evaluating the effects of physical exercises, balneotherapy, and the combination of both to treat patients with fibromyalgia Among the results obtained, the combined use of exercises and balneotherapy improved quality of sleep (p <0,001) and mention that these effects are superior to the combined use of these therapies.
Ericsson et al(13) compared the action of progressive resistance exercise centered in a control group and determined that exercise decreased fatigue and the improvement in quality of sleep was the best predictor of changes in women with fibromyalgia who presented fatigue.
Prospective cohort study
Skarpsno et al(14), in their study about insomnia as a risk factor for fibromyalgia found that the risk for this disease was directly proportional ti the number of symptoms of insomnia, and that preventing sleep disorders could be an important point in reducing the incidence of fibromyalgia. They also applied the physical activity variable, performed in their free time, concluding that maintaining a high level of activity as part of their lifestyle could reduce the risk of fibromyalgia which would produce symptoms of insomnia.
In the same manner, Joustra et al(15) determined a lower score of physical activity in patients with Fibromyalgia and Chronic Fatigue Syndrome compared to controls (9541 ± 5533; p<0,001), which is why they indicated that a direct relationship exists between sleep duration that is very high or very low and the high or low duration of physical activity with severity of symptoms, suggesting individualized treatment for these pathologies.
Analytical experimental study
Lazaridou et al(16) developed a study based in yoga as a variant of physical exercise ;posed for patients with fibromyalgia. Their results suggest that yoga could decrease the catastrophizing pain, fatigue and, in some patients, sleep disorders as well. Since yoga is a low impact physical exercise that allows the entire body to work in an organic manner, it was better tolerated and had greater acceptance among participants who decided to continue with the activity in their hoes after the study ended.
Hackshaw et al(17) proposed a therapy based on health and wellness training (HWC) for fibromyalgia resulting in a reduction in the seeking pharmacological medical treatment for calming pain and/or regulating sleep disorders in up to 86% for this group of patients (P =0,006) concluding that adding this therapy to the conventional one had greater improvement with respect to pain and quality of life in patients with fibromyalgia.
Cross-sectional studies
A study performed by Segura-Jimenez et al(18), demonstrated that the longer the periods of inactivity (ST) in patients with fibromyalgia, the greater the severity of symptoms and impact on disease. Participants with low ST levels, in episodes >60min, had a lower general impact in comparison to those who presented high ST levels (P = 0,002). They suggest that women with fibromyalgia could reduce daily ST episodes and have a more active life, since this could decrease disease activity and severity
Observational studies
Bodéré et al(19), obtained in a 5 year pilot study results of an important improvement in sleep quality, as well as relief from all symptoms in the active group made up of women with fibromyalgia who received moderate intensity continuous training (MICT) (p <0,0001). The improvements increased until the third year if study, with no significant changes evidenced in the fourth and fifth year of the study. No changes were observed in the passive group, and they were minimal in the semi-active group. Additionally, they mention that a high impact interval training (HIIT) enhanced the effects obtained with MICT regarding pain and other symptoms like depression and quality of sleep, an observation that differs from that posed by other authors regarding an excess of time or intensity of physical activity could be counter-productive for these patients.
Extrapolating other studies on patients with Juvenile primary fibromyalgia syndrome, Olsen et al(20) associated pain with sleep alterations in this group of patients concluding that a relationship exists between sleep disorders and the greater presence of pain, given that the participants, after a treatment to regulate sleep, decrease pain however, the post-treatment improvement was not in the subjective quality of sleep.
Li et al(21) amplified this topic by reviewing metanalysis but focused on the use of massage therapy for prolonged periods of time, concluding that although they improves anxiety, depression and pain intensity, they do not show benefits in sleep disorders.
Demirbag et al(22) , in the same manner, observed benefits regarding depression and sleep disorders applying therapy with touch-music-aromatherapy, furthermore, other symptoms such as morning fatigue, anxiety, gastrointestinal alterations and headaches were also decreased. This suggest that therapy could be applicable as a complete to pharmacological treatment and active lifestyle because the application by itself still has many limitations.
DISCUSSION
In this article the review found many studies that support the repercussion of moderate physical exercise on sleep disorders in patients with fibromyalgia. Furthermore, in the same studies they reference that even when different types of physical activity are applied there is a repercussion on sleep disorders among patients with fibromyalgia. Furthermore, it was demonstrated that those who had a recommended sleep duration for each one of the patients presented less pain than those who had prolonged sleep or insufficient sleep duration (15).
Authors such as Ceca, D et al(9)., Kurt, EE et al(12). emphasized the benefits that physical exercise offers regarding a good quality of sleep and offered combinations of other physical activities to potentiate these benefits.
In addition to the above, there are studies that emphasize the favorable repercussion of physical activity when facing fibromyalgia sleep disorders, resulting in improvement in quality of sleep, global decrease of these disorders becoming an important part within the treatment plan in this group of patients.
Likewise, we observed a greater response to exercise induced hypoalgesia in people with fibromyalgia that performed aerobic exercise of intermediate intensity for an approximate period of 20 minutes: data corroborates the importance of moderate physical activity (23).
We must emphasize that in other studies where different physical activity plans are applied demonstrated a benefit in patients with fibromyalgia who presented with sleep disorders (12,24).
On the other hand, the same results were obtained regarding recommended moderate physical activity for each patinate. It is demonstrated that regular physical exercise has a positive impact on pain intensity and quality of life improvement, however, carrying out very intense exercises by people with fibromyalgia increases pain by 3 points within the10 point scale and increases catastrophizing of pain, and this finding is a counter position to that previously stated since the greater pain presented, the greater the presence of sleep disorders.
Therefore, the physical activity performed, according to diverse authors, should be moderate and structured for each patient given that insufficient or excessive exercise leads to intense pain generating a rejection in the patient to continue this activity, putting the brakes on lifestyle changes (23,25,26).
Now, since a variety of pharmacological treatments exist centered on decreasing pain, we describe the limited effects, which is why the idea of prescription in a multidisciplinary therapy, where non-pharmacological methods have the same importance as pharmacological treatments, has a greater acceptance. .
Additionally, another study demonstrates the importance of counting on instruments that allow us to measure the quality of sleep, mentioning daily the fibromyalgia sleep disorder (FSD), the only measure of informed results by patients (PROM) created to evaluate the quality of sleep in those patients considering the variables that could be generated specifically in this disease.(27)
CONCLUSION
Practicing diverse types of [physical activity by patients with fibromyalgia improves quality of sleep as well as a significant decrease in pain and other symptoms of this disease. Therefore, this could be an alternative to treatment of sleep disorders, and at the same time pain management in patients that suffer from this pathology, becoming an adjuvant to pre-established pharmacological therapies.
Study limitations
One of the greatest limitations that has been presented in this study was the lack of information in Latin America since the majority of studies were carried out in Asia, Europe, among others. Furthermore, many of the studies found in the first search lacked results which hindered reaching optimal results.
Authorship contributions: The authors participated in the conception of the idea, project design, data collection, results analysis, and manuscript development of this research work.
Funding sources: Self-financed.
Conflict of interests: The author declares not having any conflicts of interest.
Received:October 8, 2021
Approved:November 16, 2021
Correspondence: Sylvia Gabriela Alfaro Castro
Address: Avenida Velazco Astete 3091 Dpto 201 – Surco
Telephone number: +51 997477029
E-mail: gabalfaroc@gmail.com
References