ARTICULO ORIGINAL
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2022 - Universidad Ricardo Palma10.25176/RFMH.v22i3.4795
MATERNAL FACTORS ASSOCIATED WITH FETAL MACROSOMIA ACCORDING TO THE NATIONAL SURVEY OF DEMOGRAPHY AND FAMILY HEALTH IN 2020
FACTORES MATERNOS ASOCIADOS A MACROSOMÍA FETAL SEGÚN LA ENCUESTA NACIONAL DE DEMOGRAFÍA Y SALUD FAMILIAR DE 2020
Angela Ruiz-Canchucaj1,a, Luis Cano-Cardenas2,b,c
1Hospital Nacional Dos de Mayo, Perú
2Ricardo Palma University, Lima-Peru
aMedical Student
bMedical Surgeon Specialist in Internal Medicine
cMaster in Public and Community Health
ABSTRACT
Introduction: Fetal macrosomia is a pregnancy condition that generates short, medium and long-term complications for the fetus, newborn and mother. Objectives: To determine the maternal factors associated with fetal macrosomia according to the 2020 National Demographic and Family Health. Methods: Observational, retrospective, analytical, cross-sectional study based on the ENDES survey in 2020 using data from 5096 women aged 12-49 who met the established criteria. For the statistical analysis, SPSS version 25 was used, the corrected F test for complex samples, and a significance level of less than 0.05. Results: The prevalence of fetal macrosomia is 7.5%. The multivariate analysis found that, within the personal factors, maternal age has a significant association with fetal macrosomia (RPa 1.04, 95% CI 1.008 – 1.078). Of the pathological factors, maternal obesity has a significant association with fetal macrosomia (RPa 1.05, 95% CI 1.027 – 1.080). Of the social and demographic factors associated with fetal macrosomia, none of the variables described show a significant association. Conclusion: It was determined that maternal age over 34 and maternal obesity are associated with a higher prevalence of fetal macrosomia.
Keywords: Fetal macrosomia; Risk factor; Maternal age; Maternal obesity. (Source: MeSH NLM).
RESUMEN
Introducción: La macrosomía fetal es una condición del embarazo que genera complicaciones a corto, mediano y largo plazo para el feto, en recién nacido y la madre. Objetivos: Determinar los factores maternos asociados a macrosomía fetal según la encuesta nacional de demografía y salud familiar de 2020 Métodos: Estudio observacional, retrospectivo, analítico, transversal que se realizó basado en la encuesta ENDES en el período 2020, utilizando los datos de 5096 mujeres de 12-49 años que cumplieron con los criterios establecidos. Para el análisis estadístico se empleó el SPSS versión 25, la prueba F corregida para muestras complejas y un nivel de significancia menor de 0,05. Resultados: La prevalencia de macrosomía fetal es de 7.5%. El análisis multivariado encontró que, dentro de los factores personales, la edad materna tiene asociación significativa con la macrosomía fetal (RPa 1.04, IC 95% 1.008 – 1.078). De los factores patológicos, la obesidad materna tiene asociación significativa con la macrosomía fetal (RPa 1.05, IC 95% 1.027 – 1.080). De los factores sociales y demográficos asociados a macrosomía fetal, ninguna variable descrita muestra asociación significativa. Conclusión: Se determinó que la edad materna mayor de 34 años y la obesidad materna son factores asociados a presentar mayor prevalencia de macrosomía fetal.
Palabras Clave: Macrosomía fetal; Factor de riesgo; Edad materna; Obesidad materna. (fuente: DeCS BIREME).
INTRODUCTION
Fetal macrosomia is a term used to describe a newborn with a weight equal to or greater than 4000 grams in Latin America. This condition is one of the main complications of pregnancy. The prevalence varies in different countries, approximately 10%, but the latest analyzes describe an increasing trend, reaching 20% in developed countries. (4) The World Health Organization (WHO) mentions that fetal macrosomia causes immediate morbidity and mortality, generating complications such as hypoglycemia, infection, birth trauma, respiratory distress, death, and admission to the neonatal intensive care unit (9) likewise increased risk of cesarean section.(4) There are associated factors that are already recognized, such as prolonged pregnancy, history of a macrosomic fetus, and male fetal sex. (18) Others more studied, such as, for example, gestational diabetes, which due to hyperglycemia peaks, generates a release of growth factors similar to insulin, which would condition a larger fetus. (17) Therefore, it is important to establish what factors could condition the presence of this complication to avoid the associated morbidity and mortality. The objective of this research is to determine the maternal factors associated with fetal macrosomia according to the national demographic and family health survey (ENDES) of the National Institute of Statistics and Informatics (INEI) in 2020, for which the research will be useful to reduce the multidisciplinary way the factors that contribute to macrosomia, from the obstetric, nutritional, behavioral part, which will lead to improvements in maternal and neonatal health.
METHODS
Design and study area
This study is observational, cross-sectional, retrospective, and analytical and consists of analyzing a secondary data source in 2020.
Population and sample
This research includes all women of childbearing age, between 15 and 49 years old, who had a macrosomic newborn (≥ 4000 grams) who voluntarily completed the survey and filled in the data entirely in the household and individual questionnaires in the ENDES 2020. Likewise, women of childbearing age excluded, between 15 and 49 years old, who answered "I don't know" or "I don't remember" in the ENDES 2020 questionnaires. The sample size was 5,096 women, and the type of sampling was a two-stage, probabilistic, balanced type.
Variables and instruments
For data collection, the information from the Microdata base was exported to the statistical software SPSS version 25. The database was downloaded, and the variables of interest were located.
| Variable | Label of the variable | Type of variable | Database |
|---|---|---|---|
| M19 | Birth weight (Macrosomia) | Dependent | Modulo1633- rec41 |
| HA40 | Maternal weight | Independent | Modulo1638- rec5 |
| V012 V190 V025 | Maternal age Index of wealth Area of residence | Independent | Modulo1631- rec0111 |
| S108N S119D | Educational Ethnicity | Independent | Modulo1631-rec91 |
| QS109 QS102 | Gestational Diabetes Gestational Hypertension (Comorbidity) | Independent | Modulo1640-csalud 01 |
| V219 V214 | Multiparity Duration of pregnancy | Independent | Modulo1632-re223132 |
Procedures
The variable "Macrosomia" was coded from Weight of the newborn ≥ 4000 g, the variable "Maternal comorbidity" was also coded, combining the pathologies of gestational diabetes and gestational hypertension. The "Obesity" variable was coded from "Maternal weight", establishing BMI > 30. The remaining variables kept the coding established by the INEI Microdata dictionary. A data file was created with the fusion of all the variables necessary for the execution of the study, taking into account the identifiers CASEID and HHID according to the ENDES.
Once the variables have been merged, the missing data are eliminated. The variable "duration of pregnancy" is also eliminated since it has many invalid data, increasing the possibility of error in the investigation. The design of complex samples was carried out, creating a CSPLAN, using the Stratum variable (V0005), conglomerate variable (N. CONGLOM), and the sample weighting factor.
Statistical analysis
The univariate analysis was carried out to know the descriptive characteristics of the population, the percentages obtained were calculated through complex samples, using the weighting factors; in addition, the relative sampling error (RSE) was determined with an accepted value of less than 15 %.
For the association, the corrected F test for complex samples was used, a single multivariate analysis model was carried out, in which the variables with and without statistical significance were included due to its relevance in the literature reviewed, calculating the adjusted RP using the Poisson regression model with robust variance.
For the writing of the tables of the multivariate analysis it was separated by personal, pathological, and sociodemographic factors. Thus determining the maternal factors associated with fetal macrosomia, accepting a confidence level equal to or greater than 95.
Ethical aspects
The ENDES database has informed consent, and the ethical principles applied to research are respected, all corroborated by the ethics committee of the Ricardo Palma University.
RESULTS
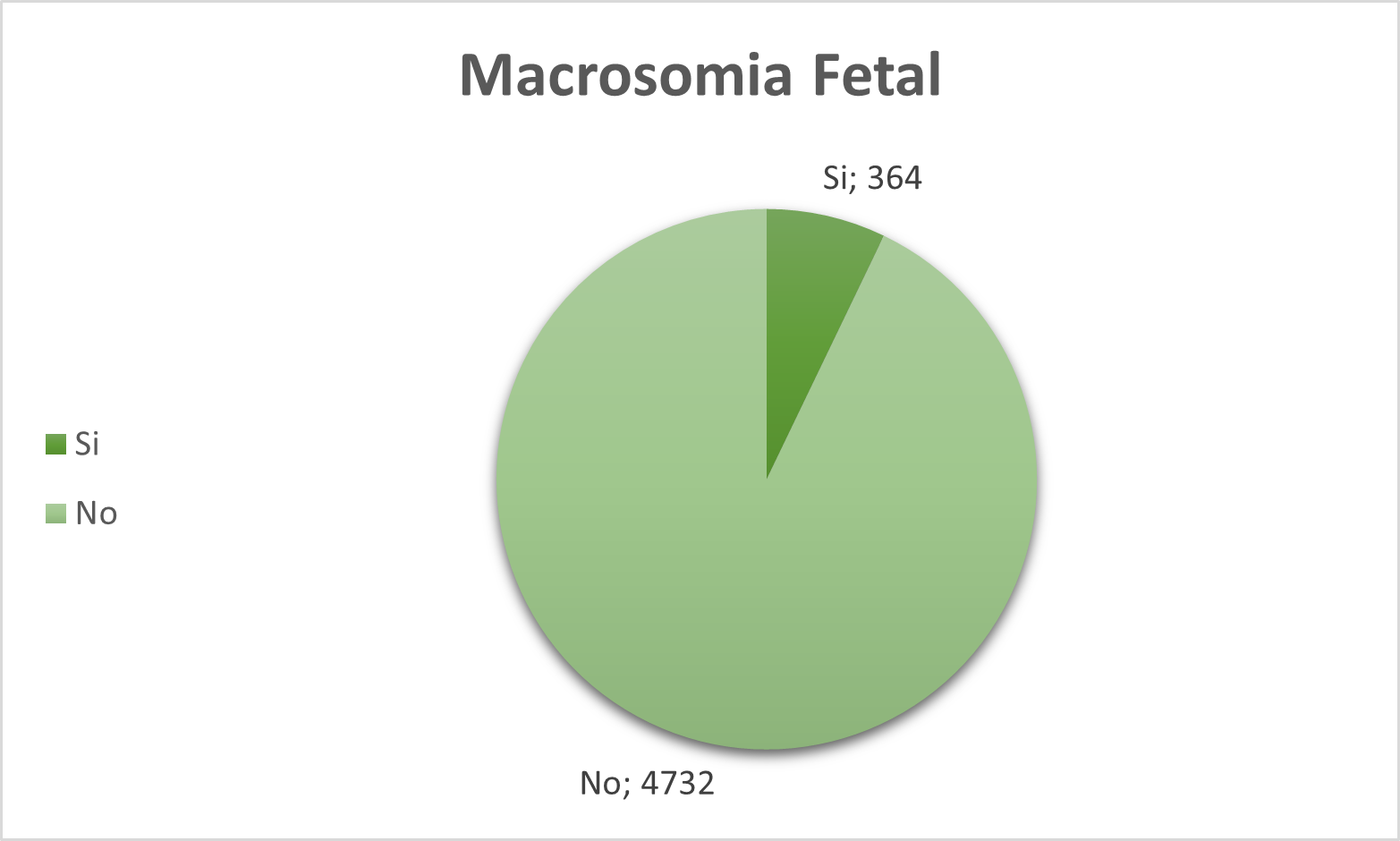
An analysis of 5096 Peruvian women who met the inclusion and exclusion criteria was performed, where it was determined that the prevalence of fetal macrosomia is 7.5% (Figure 1).
In the univariate analysis, it was determined that the most prevalent maternal age is 25-33 years with 47.1%, 74% were multiparous , 30.6% had maternal obesity during pregnancy, 4% had maternal comorbidity during pregnancy, in terms of wealth index 46.5% are poor, 77.2% belong to the urban area, 50.8% are mestizo, 49.7% secondary education level. (Table 1)
Tabla 1. Maternal factors associated with Fetal Macrosomia according to the national demographic and family health survey in 2020.
| Variables | n | % | CI 95% | MRD |
|---|---|---|---|---|
| Maternal Age | ||||
| 15-24 | 1017 | 18.9 | 17.4 - 20.5 | 4.2% |
| 25-33 | 2385 | 47.1 | 44.9 - 49.3 | 2.4% |
| 34 or older | 1694 | 34.1 | 32.1 - 36.1 | 3.0% |
| Multiparity | ||||
| If | 3848 | 74.0 | 72.3 - 75.7 | 1.2% |
| No | 1248 | 26.0 | 24.3 - 27.7 | 3.3% |
| Maternal obesity | ||||
| If | 1536 | 30.6 | 28.6 - 32.7 | 3.4% |
| No | 3560 | 69.4 | 67.3 - 71.4 | 1.5% |
| maternal comorbidity | ||||
| Yes | 216 | 4.0 | 3.3 | 10.2% |
| NO | 4880 | 96 | 95.1 - 96.7 | 0.4% |
| wealth Index | ||||
| Poor | 2817 | 46.5 | 44.4 - 48.5 | 2.2% |
| Average | 1068 | 21.1 | 19.3 - 22.9 | 4.3% |
| Rico | 1211 | 32.4 | 30.3 - 34.7 | 3.4% |
| Residence Area | ||||
| Urban | 3639 | 77.2 | 75.7 - 78.6 | 1.0% |
| Rural | 1457 | 22.8 | 24.3 | 3.3 |
| Ethnicity | ||||
| Black | 540 | 10.7 | 11.8 | 5.3 |
| White | 379 | 8.5 | 7.4 | 7.2 |
| mestiz | _ | _ | - | % |
| _ | _ | _ | _ | % |
| 9.8 | ||||
| 9.6 | 21.4 | - | - | %% |
| Secondary | 2560 | 49.7 | 47.5 - 51.8 | 2.2% |
| Superior | 1651 | 35.7 | 33.6 - 37.9 | 3.1% |
According to the multivariate analysis of personal factors, it was determined that having a maternal age of 34 years or older increases the prevalence of fetal macrosomia by 1.04 times, a statistically significant association (RPa 1.04, CI 95% 1.008 - 1.078). Likewise, it was determined that multiparity had no significant association. (Table 2)
Table 2. Multivariate analysis of maternal personal factors associated with Fetal Macrosomia in the Peruvian population according to the national demographic and family health survey in 2020
| Personal Factors | Crude RP | 95% CI | P value | Adjusted RP | 95% CI | P value |
|---|---|---|---|---|---|---|
| Maternal Age | ||||||
| 34 A MORE | 1.05 | 1.01 - 1.08 | 0.002 | 1.04 | 1.008 - 1,078 | 0.016 |
| 25-33 | 0.99 | 0.97 - 1.02 | 0.845 | 0.99 | 0.968 - 1,021 | 0.668 |
| 15-24 | 1.00 | 1.00 | ||||
| Multiparity | ||||||
| Yes | 1.03 | 1.00 - 1.05 | 0.016 | 1.01 | - | 0.412 NO |
| 1.034 | 1.00 | 1.00 | ||||
| 0.9862020 | ||||||
Regarding the multivariate analysis of the pathological factors, it was determined that suffering from maternal obesity increases the prevalence of fetal macrosomia by 1.05 times, a statistically significant association (RPa 1.05, CI 95% 1.027 – 1.080). In addition, it was determined that having maternal comorbidity had no significant association. (Table 3)
Table 3. Associated Multivariate analysis of maternal pathological factors Fetal with Macrosomia in the Peruvian population according to the national demographic and family health survey in 2020.
| Pathological Factors | Crude RP | 95% CI | P value | adjusted RP | CI 95% | P |
|---|---|---|---|---|---|---|
| Maternal Obesity | ||||||
| Yes | 1.05 | 1.02 - 1.08 | 0.000 | 1.05 | 1.027 - 1,080 | <0.001 |
| No | 1.00 | 1.00 | ||||
| Maternal Comorbidity | ||||||
| If | 1.03 | 0.97 - 1.09 | 0.313 | 1.02 | 0.983 - 1,088 | 0.457 |
| No | 1.00 | 1.00 | ||||
With respect to the data in the analysis in the analysis multivariate analysis of social and demographic factors, it was determined that none of the variables showed statistical significance (Table 4)
Tabla 4. Título 4 de la tabla lorem impsum.
| Sociodemographic factors | Crude RP | 95% CI | P value | Adjusted RP | 95% CI | P value |
|---|---|---|---|---|---|---|
| Wealth Index | ||||||
| RICO | 1.01 | 0.99 - 1.03 | 0.207 | 1.01 | - 1,044 | 0.366 |
| Medium | 1.03 | 1.00 - 1.06 | 0.037 | 1.03 | 0.995 - 1,061 | 0.100 |
| Poor | 1.00 | 1.00 | ||||
| Residence Area | ||||||
| Urban | 1.02 | 1.04 | 0.048 | 1.01 | - 1,044 | 0.314 |
| Rural | 1.00 | 1.00 | ||||
| Ethnic | ||||||
| Black | 0.984 | - | 0.986 | 1.00 | 0.968 - 1.047 | 0.737 |
| Mestizo | 0.98 | 0.96 - 1.01 | 0.327 | 0.98 | 0.962 - 1.012 | 0.293 |
| Blanca | 0.98 | 0.94 - 1.02 | 0.381 | 0.98 | 0.950 - 1.023 | 0.462 |
| Otros | 1.00 | 1.00 | ||||
| Nivel Educativo | ||||||
| Primaria a menos | 1.00 | 0.97 - 1.04 | 0.754 | 1.01 | 0.977 - 1.053 | 0.465 |
| Secundaria | 0.98 | 0.96 - 1.01 | 0.35 | 0.99 | 0.969 - 1.018 | 0.585 |
| Higher | 1.00 | 1.00 |
DISCUSSION
We have identified the factors associated with the higher prevalence of fetal macrosomia, understood as a newborn with a birth weight greater than and equal to 4000 grams, one of the main complications of pregnancy associated with problems of short, medium and long term for the neonate, the fetus and for the mother.(2) Within public health, they have focused on low birth weight; however, with the current change in lifestyle and sedentary lifestyle, neonatal weight gain highlights this problem, which is why it is relevant to determine the maternal factors that are associated with fetal macrosomia to avoid future complications.
In the present investigation, it was determined that the prevalence of fetal macrosomia was 7.5%, data similar to those proposed by the WHO, which shows figures of 7.6% in South America, while in Peru, the figure found was 6.9% (1) Trujillo also carried out a study at the Hospital of Barranca - Cajatambo identifying that 7.16% of newborns presented fetal macrosomia. (12)
Within the personal factors, it was determined that maternal age of 34 years or more increases the prevalence of fetal macrosomia by 1.04 times (RPa 1.04, 95% CI 1.008 – 1.078). Similar data was found in the study by Wang were determined that in the age group over 33 years, there is a higher prevalence of fetal macrosomia (OR = 1.029, 95% CI: 1.012 - 1.046).(7) Also, Aisha Salim, in her article, showed that 55.3% of the mothers who had macrosomic babies belonged to the age group of 30 to 39 years (OR = 2.1 95% CI 1.2 - 3.7), (11), thus evidencing that the older the mother is, the more prevalent a newborn is with macrosomia, this would be based on the fact that advanced age would have an effect on maternal metabolism and thus increase the growth rate of the fetus.(19)
Another personal factor studied was multiparity, which did not show a significant association. In contrast to the study carried out by Salas in Spain, who argues that multiparity has been related to the presence of macrosomia (OR = 1.67, 95% CI 1.2-2.2) (4); which agrees with León who identifies that multiparity is a risk factor associated with fetal macrosomia (OR=2.027 95% CI 1.22-3.54) (14) All this differs from the results obtained in this study because possibly the question "Number of pregnancies" was interpreted subjectively since it did not take into account whether or not it included the current pregnancy.
Among the pathological factors, it was determined that suffering from maternal obesity increases the prevalence of presenting fetal macrosomia by 1.05 times (RPa = 1.05, CI 95%, which is consistent with the cohort study carried out by Lewandowska, where he determined that the prevalence of macrosomia is higher for pregnant women with obesity compared to normal BMI (OR = 3.21 95% 1.69-6.1) (5), similar to that found by Dsouza in his meta-analysis in which argues that women with a BMI >40 kg/m2 have a higher prevalence of fetal macrosomia (9). Likewise, Pereda carried out a study where he determined that macrosomia is more likely in obese women at the end of pregnancy (OR = 2.21; 95% CI 1.90-2.58) (8). Likewise, in her study, Aisha Salim found that women with a birth weight greater than or equal to 80 kg were four times more likely to give birth to macrosomic babies (OR= 4.0 95% CI 2.2–9.1).(13) This would be explained because having a higher consumption of carbohydrates and fats, the glucose values in the mother would rise, which would condition hyperinsulinemia in the fetus, for which large amounts of fat would be formed, causing overgrowth in the fetus. fetus.(17)
The other factor that is recognized is the presence of diabetes and gestational hypertension, which in this investigation had no significant association. In contrast to the Vega study, which determined that maternal diabetes (PR = 5.42 95% CI 4.97 – 5.74), maternal gestational hypertension (PR = 1.40 95% CI 0.90 – 3.50) would be factors associated with the presence of macrosomia.(13)Torres carried out a study of the pathologies that accompany pregnancy, in which he identified that pregnancy-induced hypertension would be associated with a higher prevalence of having a macrosomic fetus (OR = 3.58 95% CI 1.47 – 8.72) ( 3) In the same study, the presence of gestational diabetes did not present statistical significance of having a macrosomic newborn. (3) Because the sample with gestational diabetes was small, which would also explain the result of our study. Another study conducted by Alfadhli found that pregnant women with the highest prevalence of macrosomia were those of the diabetes-obese group (32%) followed by diabetes-non-obese (18%), thus demonstrating the influence of diabetes and obesity alone or combined for the presence of fetal macrosomia. (6)
Within the sociodemographic factors, none of the variables analyzed showed statistical significance. However, multiple studies do identify an association with various variables that were analyzed in this research. Annie Ro carried out an investigation in which the non-Hispanic white ethnic group was identified as having a higher prevalence of fetal macrosomia (16), which contrasts with our study in which the ethnic group did not show an association, which could possibly be explained by a racial difference.
Regarding the area of residence, Vega determines that living in an urban area is a factor associated with a higher prevalence of fetal macrosomia (64.7% and PR = 4.8) (13). This is reinforced by Cunha, who highlights that belonging to the rural area is a protective factor against fetal macrosomia (OR 0.64 CI 95% 0.41 – 0.99)(15) In the same study, as an index of wealth, Cunha determined that an index of wealth not poor would be associated with a higher prevalence of macrosomia (OR 1.10 CI 95% 0.44 - 2.71) (15) This differs from the present investigation since urban residence. The rich wealth index does not present a significant association, probably due to the size of the sample used.
The other aspect Espitia conducts a study in Colombia in which he argues that the secondary-university educational level has a higher prevalence of fetal macrosomia PR 1.06 (0.66–1.69), p: 0.817 (2) , in contrast to our study where the population characteristics studied are different, for which no statistical significance was obtained, likewise Cunha carried out his study in Peru in which the educational level did not present a direct association with fetal macrosomia either.(3)
One limitation of our study was a possible sample bias due to the size of the sample, differences in ethnicity, and the characteristics of the population studied. Another limitation was the type of methodology used in this research, also given that this The study is carried out using a secondary source such as the microdata base of the Demographic and Family Health Survey (ENDES). It is important to consider that this does not aim to identify risk factors that condition fetal macrosomia, for which there are biases typical of the data source, such as false, ambiguous, and incomplete responses.
CONCLUSIONS
This study determined that the maternal factors associated with the prevalence of fetal macrosomia according to the 2020 National Demographic and Family Health Survey were maternal age over 34 years and the presence of maternal obesit
Authorship contributions: Angela Ruiz Canchucaja: Conceptualization, data quality, statistical analysis, project writing, project administration;
Luis Alberto Cano Cardenas: methodological advice, supervision, drafting of the final version, revision of the final version.
Funding sources: self.
Conflicts of interest: The authors declare that they have no conflict of interest.
Received: January 03, 2022
Approved: March 04, 2022
Correspondence: Angela Ruiz Canchucaja.
Address: Avenida Central 997 – Urbanizacion Los alamos de Monterrico , Santiago de Surco.
Telephone number: 992604965
E-mail: angelarc0407@gmail.com
Article published by the Journal of the faculty of Human Medicine of the Ricardo Palma University. It is an open access article, distributed under the terms of the Creatvie Commons license: Creative Commons Attribution 4.0 International, CC BY 4.0(https://creativecommons.org/licenses/by/1.0/), that allows non-commercial use, distribution and reproduction in any medium, provided that the original work is duly cited. For commercial use, please contact revista.medicina@urp.edu.pe.
REFERENCES
