ARTICULO ORIGINAL
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2021 - Universidad Ricardo Palma10.25176/RFMH.v22i2.4796
HOSPITAL MANAGEMENT OF A PUBLIC-PRIVATE PARTNERSHIP MODEL AND A TRADITIONAL MODEL IN TWO HOSPITALS IN CALLAO
GESTIÓN HOSPITALARIA DE UN MODELO DE ASOCIACIONES PÚBLICO PRIVADAS Y UN MODELO TRADICIONAL EN DOS HOSPITALES DEL CALLAO
Humberto Dario Zinelli Reyes1,a
1Hospital Nacional Edgardo Rebagliati Martins-EsSalud. Lima, Perú.
aCirujano Pediatra
ABSTRACT
Introduction: The Peruvian health system usually has deciencies, This is how, since 2008, we have worked on the model of Public-Private Partnerships in Health (PPP), which seeks the best performance of the health system before being applied in the rest of similar hospital centers of the Peruvian health system. Objective: To compare the hospital management of a PPP model and a traditional model in two Essalud level II-2 hospitals. Methods: Mixed, non-experimental, and cross-sectional research carried out in two establishments, Hospital Alberto Barton Thompson (HABT) as PPP model and Hospital Luis Negreiros Vega (HLNV) as the traditional model, during the hospital management period from 2016 to 2018, six public officials and 150 external users. Hospital management was evaluated through hospital efficiency, nancial management, and user satisfaction. Results:In-hospital efficiency, the HABT presented below-standard medical-hour performance (3.31 in 2018), and lower compared to the HLNV (4.74in2018).In financial management,for both models of public-private management,it is agreed that procurement plans must be carried out in advance, with common problems: ignorance of operational plans, poor epidemiological surveillance, and insufficient strengthening of skills and competencies; likewise, the APP modality spends three times more compared to the traditional modality.Conclusion:A PPP modality health facility, such as the HABT, does not seem to present better results than a traditional format facility such as the HLNV
Keywords: Hospital administration; Public-Private Sector Partnership; Patient satisfaction.(fuente: MeSH NLM).
RESUMEN
Introducción: El sistema de salud del Perú suele tener deficiencias, así es como desde el 2008, se trabajó en el modelo de Asociaciones Público Privadas en Salud (APP), el cual busca el mejor rendimiento del sistema de salud antes de ser aplicada en el resto de centros hospitalarios parecidos del sistema de salud peruano. Objetivo: Comparar la gestión hospitalaria de un modelo APP y un modelo tradicional en dos hospitales de nivel II-2 de Essalud. Métodos: Investigación mixta, no experimental y transversal realizada en dos establecimientos, Hospital Alberto Barton Thompson (HABT) como modelo APP y Hospital Luis Negreiros Vega (HLNV) como modelo tradicional, durante el periodo de gestión hospitalaria del 2016 al 2018, seis funcionarios públicos y 150 usuarios externos. La gestión hospitalaria fue evaluada mediante la eficiencia hospitalaria, gestión financiera y satisfacción del usuario. Resultados: En eficiencia hospitalaria el HABT presentó rendimiento hora-médico por debajo del estándar (3.31 en el 2018), y menor respecto al HLNV (4.74 en 2018). En la gestión financiera, para ambos modelos de gestión público-privada, se coincide que los planes de adquisiciones deben realizarse anticipadamente, siendo problemáticas comunes: el desconocimiento de planes operativos, vigilancia epidemiológica deficiente e insuficiente fortalecimiento de capacidades y competencias; asimismo, la modalidad APP gasta tres veces más en comparación a la modalidad tradicional. Conclusión: un establecimiento de salud de la modalidad de APP, como el HABT, no parece presentar mejores resultados que un establecimiento de formato tradicional como el HLNV.
Palabras Clave: Administración hospitalaria; Asociación entre el Sector Público-Privado; satisfacción del paciente.(fuente: DeCS BIREME).
INTRODUCTION
The health system in Peru is characterized by being fragmented, of low production, and of little coordination between the sectors that compose it, with very deficient stewardship(1); moving towards recuperative health and neglects the function of prevention and health promotion. One of the components is the Social Security of Peru (EsSalud), which covers 11.5 million people (30% of the Peruvian population), whose financing comes from the contribution of employers, which corresponds to 9% of the worker's salary and provides health services through its 409 health establishments distributed nationwide(2).
The main problem of EsSalud is the perception of the insured population of poor quality of service that does not find medical appointments when requesting them, either in person, by telephone, or through web platforms. Likewise, many appointments are provided one to two months after being requested, even in some cases, for example, in neurosurgery; they are granted after six months. This causes continuous claims from the population and a double expense for the insured, for having to go to private services, different from EsSalud, to be able to solve their acute health problems, and they end up going to various hospital centers for emergencies, generating overcrowding and long stays. in emergency rooms(3).
It is necessary to consider that the population assigned to EsSalud is similar to that of developed countries since they have a life expectancy that exceeds the national average (> 76 years). This insured population suffers from chronic health problems that lead to repeated medical consultations and an over-demand of emergency services, requiring hospital management to perform optimally to meet the health demands of the population adequately. In addition, EsSalud lacks infrastructural planning, since in recent years it has gone from serving 8 to 11.5 million insured persons with the same infrastructure and a scant increase in human resources, generating an overload of care for health personnel, who it harms organizational performance, prevailing demotivation, adverse work environment and internal user dissatisfaction(4).
To help solve these problems, the best international experiences are observed; This is how in Peru, since 2008, the model of Public-Private Health Associations (PPPs) has been worked on, the national legal framework is created and after the respective learning, two PPP contracts were signed in 2011(5), one of them with the Alberto Leonardo Barton Thompson Hospital in Callao, constituting the first experience that works under this modality in Latin America. This hospital has 25 medical and surgical specialties; In addition, it has 215 beds, 07 operating rooms, 03 delivery rooms, a hemodialysis unit, 100 outpatient clinics, and state-of-the-art equipment, which has 250,000 affiliated insured persons (6).
This APP was conceived as a pilot to seek the best performance of the health system before being applied in the rest of similar hospital centers of the Peruvian health system. Therefore, the objective of this research is to measure the impact of the public-private partnership management model in the hospital management system of Essalud level II, Callao region 2019, to serve as input in decision-making of Peruvian public policies. in health, likewise, as a benchmark in Latin American countries and other low-middle income countries that have deficient health systems with economic income from the state that do not cover the total financing of health, as occurs in developed countries. The objective of this study was to measure the impact of the PPP management model on the EsSalud level II-2 hospital management system.
METHODS
Design and study area
Cross-sectional, non-experimental, mixed approach study in the area of hospital management.
Population and sample
For the analysis of user satisfaction, the population was made up of 500,000 insured persons assigned to the Alberto Barton Thompson Hospital (HABT) and the Luis Negreiros Vega Hospital (HLNV) during the hospital management period from 2016 to 2018, from a sample of 150 was taken non-probabilistic. For the qualitative analysis, the population was made up of all the public officials of the EsSalud II-2 hospital establishments in question; the sample was made up of 6 public officials assigned in equal proportion to the EsSalud establishments under study by non-probabilistic sampling type and sampling technique convenience sampling. For the analysis of hospital efficacy, three consecutive years of the hospital management period from 2016 to 2018 were selected as a universe, and various aspects were evaluated based on hospital management indicators.
Inclusion criteria were considered to be the voluntary acceptance of the insured (member or family member) who attended the HABT or HLNV in the aforementioned periods. Likewise, the main criterion for selecting public officials was the absence of administrative restrictions that prevented their participation.
Variables and instruments
The first study variable was the hospital management model, operationally defined as an EsSalud facility managed under the PPP model (HABT) or the traditional model (HLNV).
The other variables were related to hospital management: hospital efficiency, financial management, and user satisfaction. Hospital efficiency was evaluated using the documentary technique and through 13 indicators of the sixteen cited in the MINSA Working Document(7) on Hospital Management and Evaluation Indicators, for Hospitals, Institutes and DIRESA; which are the following: medical-hour performance, the concentration of consultations, average stay, replacement interval, percentage of bed occupancy, bed performance, emergency reason, operating room performance, cesarean section rate, suspended operations, percentage of patients in the observation room, delivery room performance and average ICU stay.
The evaluation of financial management was carried out using the interview technique and the instrument was the interview guide, made up of 11 open questions addressed to public officials of the HABT and HLNV, which were aimed at inquiring about: i) annual procurement plan, ii) strengthening program; iii) execution of expenses; iv) hospital infrastructure; v) epidemiological surveillance; vi) financial and budget information; vii) job promotion; viii) management and execution of funds; ix) payment compliance; and x) the public-private partnership management model.
On the other hand, user satisfaction was evaluated through the survey as a technique and as an instrument, a questionnaire made up of eight closed questions, with a Likert response option of five levels (from "totally dissatisfied" to "totally satisfied").
Procedures
A data collection form was created for the variables described. Data collection was performed by trained researchers. Once the consent of the insured or public official was obtained, the instrument began to be filled out.
Statistical analysis
The analysis of the interviews was carried out by recording, transcribing, analyzing, and interpreting the interviews within the qualitative methodology of content analysis. The quantitative was performed in Microsoft Excel 2016. For categorical variables, absolute (n) and relative (percentage) frequencies were used, while for the numerical variables, the average was used as the only measure of central tendency.
Ethical aspects
The procedures described in this study were based on the collection of data from documentary sources, which avoided, for the most part, putting human life at risk. With regard to interviews and surveys (carried out with officials and users, respectively), these were carried out after granting consent to participate; however, it is necessary to clarify their anonymous nature and respect for identifiable information during data processing, in accordance with the bioethical principles of the Declaration of Helsinki.
RESULTS
Concerning hospital efficiency, it is observed that the Negreiros Hospital attends to more patients per hour (performance per hour 4.77), the beds are occupied more frequently (replacement interval 0.48), the number of patients who occupy a bed is greater (bed performance 9.93), there is a greater number of surgical interventions (operating room performance 161.63) and a greater number of deliveries per room (delivery room performance 173.81). While the Alberto Barton Hospital has more care per patient (concentration per consultation 2.80), it keeps its patients more days (average stay 4.18), more cesarean sections were performed (41.3% cesarean section rate), more operations were suspended (892.67). Patients were kept in ICU beds for a longer time (8.03). Likewise, a similar trend is observed in bed occupancy between both hospitals (84.2% vs. 88.6%). (Table 1)
Table 1. Hospital efficiency according to the PPP management model (HABT) or under the traditional model (HLNV), 2016-2018
| Hospital Efficiency Hospital | Hospital Luis Negreiros | Hospital Alberto Barton | ||||||
|---|---|---|---|---|---|---|---|---|
| 2016 | 2017 | 2018 | Media | 2016 | 2017 | 2018 | Media | |
| Performance Physician Hour | 4,78 | 4,80 | 4,74 | 4,77 | 3,92 | 4,13 | 3,31 | 3,79 |
| Concentration of consultations | 2,47 | 2,44 | 2,30 | 2,40 | 3,15 | 2,78 | 2,48 | 2,80 |
| Average length of stay | 2,77 | 2,81 | 3,11 | 2,90 | 2,79 | 3,94 | 5,80 | 4,18 |
| Replacement interval | 0,49 | 0,49 | 0,47 | 0,48 | 0,36 | 0,45 | 0,70 | 0,50 |
| % bed occupancy | 84,5% | 83,2% | 84,8% | 84,2% | 88,1% | 90,4% | 87,2% | 88,6% |
| Litter | 9,7 | 10,34 | 9,75 | 9,93 | 10 | 6,57 | 5,55 | 7,37 |
| Emergence | 1,59 | 1,64 | 1,16 | 1,46 | 0,85 | 0,78 | 1,27 | 0,97 |
| Operating room performance | 163,40 | 167,53 | 153,96 | 161,63 | 115,06 | 143,29 | 103,90 | 120,75 |
| Cesarean section rate | 31,3% | 37,5% | 40,5% | 36,4% | 42,1% | 41,1% | 40,6% | 41,3% |
| Suspended operations | 665 | 820 | 692 | 725,67 | 1090 | 1029 | 559 | 892.67 |
| % of patients in observation room | 24,4% | 23,4% | 22,5% | 23,4% | 44,0% | 17,9% | 5,7% | 22,5% |
| Delivery room performance | 177,92 | 167,38 | 176,13 | 173,81 | 71,39 | 78,86 | 77,78 | 76,01 |
| Average ICU stay | 5,98 | 5,35 | 5,44 | 5,59 | 8,38 | 8,21 | 7,5 | 8,03 |
Regarding the management hospital, interviews were conducted, and from the responses provided by the public officials of the HLNV and the HABT in what corresponds to the annual procurement plan, the HLNV carried it out in advance according to the needs of each of its areas, it was consolidated by the Benefit Network and sent to the Headquarters for approval; Similarly, the HABT worked on its annual plan from the middle of the year to have a good programming of materials, supplies, equipment and personnel.
In relation to the execution of expenses according to the activities programmed in the institutional operational plan and budget availability, according to the HLNV officials, there was an operational plan. However, it was not made known to them at the precise moment, the reason for which an adequate execution of the expenses was not carried out; The same thing happened with the Barton Hospital, the lack of knowledge of the operational plan was reflected in the shortage of materials, equipment, supplies, etc.
Regarding hospital infrastructure, HLNV workers mentioned limitations for staff such as lack of ergonomic chairs for administrative areas or uninstalled exhaust fans, while HABT workers stated that the hospital has good infrastructure, but there are problems in some environments such as the waiting room, where there is a risk of cross-infection due to lack of maintenance and ventilation.
Regarding epidemiological surveillance, Negreiros Hospital officials noted that the lack of budget and personnel limits the planning area, and the quality area, which is the only one that has epidemiology personnel. Barton Hospital officials considered that epidemiological surveillance is deficient because favorable behaviors are not complied with, such as submitting reports of nosocomial infections, emerging diseases, and mandatory notification, etc.
Regarding the reports of financial and budget information, according to the norm, the officials of the Negreiros Hospital agreed that there was a delay in the reports because the information after its elaboration goes through the head of services and then by the administration area in coordination with the hospital costs area, this contrasts with the reports issued by the HABT in its beginnings according to what its workers said since these were precise and fully approved. Currently, they believe that the regulations are still being complied with.
Regarding labor promotion, the HLNV workers affirmed that there are personnel training programs and that labor promotion is handled internally in the Human Resources area and in the Central Headquarters.
On the other hand, in the case of HABT, if there is a job promotion, they look for internal staff as the first option, and if they do not find someone with the desired profile, they proceed to external advertising.
As for applying the directives issued by MINSA and the Ministry of Economy and Finance, in terms of management and execution of funds, HLNV officials affirm that there is no direct management of the budget, but they do generate information on their income and hospital costs. Based on the ESSALUD directive, the HABT officials do not have clear knowledge on the subject but presume the existence of mandatory compliance with the issued directives.
Regarding the alternative measures for compliance with payment of debt service, installment of debts, work for service received, follow-up of third parties for the collection, the HLNV workers stated that there was no installment system since the patients served pay according to their possibilities, many of them with debts up to now, however, there is a follow-up by amounts and also a follow-up for the service work received. On the other hand, the workers at Barton Hospital are unaware of the issue.
Concerning the public-private partnership management model, HLNV officials consider that given the high demand from users, for example in the emergency area, the APP serves to meet this type of demand and they qualify the model as fair-good. In the same way, the HABT workers consider that it is a good model because it allows them to offer a better service to EsSalud patients.
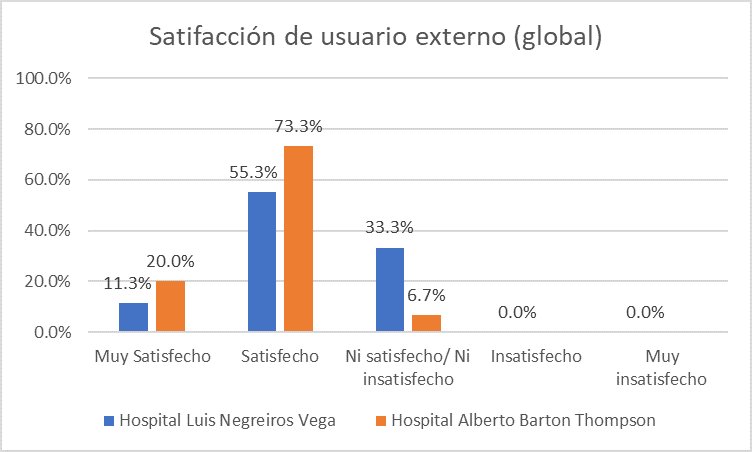
Regarding user satisfaction, Figure 1 describes user satisfaction, where it was found, globally, that the HABT (APP) showed a higher level of satisfaction than the HLNV (93.3% vs 66. 6%), in terms of user satisfaction according to services, it is evident that 12% of users treated at the HABT feel very satisfied with the outpatient service and 8.7% of those who are treated at the HLNV had the same perception of satisfaction, globally 72.7% of HLNV users and 72% of HABT users are satisfied with this service; With regard to satisfaction with the emergency service, 15.3% of users seen at the HABT are very satisfied, and 9.3% of those seen at the HLNV had the same perception of satisfaction. Globally, 63.3% of HLNV users and 64.6% of HABT users are satisfied with this service; On the other hand, in the hospitalization service, 66.7% of users treated at the HABT are delighted, and 55.3% of those who are treated at the HLNV had the same level of satisfaction. Found that 86.6% of HLNV users and 74.0% of HABT users are satisfied with the service.
DISCUSSION
The PPP between the public health sector and the private sector is based on a business model that aims to take advantage of the experience of the private sector to improve the clinical performance of health facilities. Although the financial implications of such partnerships have been explored (8), few studies have examined the impact of PPPs on clinical performance outcomes.
In this research, we evaluate the impact of PPPs, using quantitative measures that reflect hospital efficiency, financial management, and user satisfaction.
Regarding the hospital indicators, it is observed that the behavior is variable in both hospitals. Compared to the national averages, they are below the average in most indicators but with more advantageous results in the HLNV(7).
It has been observed that the health establishment under the public-private association modality has a physician-hour performance below the national standard, with a decreasing trend in recent years, and is lower compared to the HLNV(7). The average number of consultations in both hospitals is below the standard, less than 3.5 consultations on average(7). Regarding the average length of stay or days of stay, this is much higher in the HABT than the HLNV (close to 2 extra days on average).
In both hospitals, programs were developed for job promotion, where the first option is sought among the internal staff and in the case of not finding the person with the profile sought, the external promotion is made. However, there were aspects that were not optimally managed in both hospitals, such as the annual procurement plan, the program to strengthen capacities and skills for the administrative systems (budget, treasury, and accounting), lack of knowledge of the operating plan, and lack of knowledge of the board of directors. issued by MINSA and the Ministry of Economy and Finance in matters of management and execution of funds.
The officials of both health establishments considered that the public-private partnership model was good, since it offers adequate service to EsSalud patients. These results are in agreement with those reported by Pérez et al. (9), who carried out an investigation entitled "Multilevel analysis of the technical efficiency of hospitals in the Spanish National Health System by type of ownership and management", the results suggested that traditional hospitals have a lower average efficiency index compared to hospitals with public-private collaboration. For their part, Franco and Fullana (10), found that PPP management models have greater assistance and spending efficiency than other forms of management. While, traditionally managed hospitals have better research efficiency results compared to other forms of management.
These results correspond to those observed by Jorge et al. (11) who carried out an investigation entitled "Efficient Management of Primary Health Care at the first level of care and its impact on the level of user satisfaction: EsSalud Case" and where it was found that the PPP management model Based on management in Primary Health Care, it improves the satisfaction of the insured, determined by accessibility to appointments, delivery of medicines and medical and non-medical care. For his part, Paripancca (12) found that there was a significant relationship between the dimensions of quality of care and the satisfaction of external users referred in a public-private association hospital.
The results of this research do not confirm the results observed in the international context, where health establishments are administered by a PPP, as in another study by Franco and Fullana(13) where they compare three types of establishments: private management, public-public association private and public management, the former being the one with the best efficiency rates. There are several favorable elements that support the traditional management model as in the Negreiros Hospital, first of all, with more efficient hospital indicators such as medical hour performance, occupancy percentage and performance per bed, operating room performance, suspended operations , delivery room performance and average ICU stay. In the second instance, it is related to financial and budget information, with similar results in both models, however, the hospital by PPP modality spends three times more than one by traditional modality, and, finally, a higher level of global satisfaction to 60% and in many cases as an outpatient clinic and hospitalization with higher satisfaction indicators than the APP model.
The differences are not revealing in both models of hospital management, with weaknesses and strengths in both formats, it is appropriate to establish corrective actions or measures to address these critical aspects and strengthen the favorable aspects, focused on improving the quality of care of the insured patient and consequently raise the quality of life of the same. Likewise, the establishment of a human resource needs plan is recommended to provide sufficient assistance personnel and adequately condition the environments such as the expansion of these in many areas such as waiting, emergency, administrative, epidemiological surveillance, among others, in both hospitals, to meet the great demand of patients in such a way as to optimize hospital efficiency.
Within the limitations of the study, it is found that, having carried out a qualitative analysis and a descriptive quantitative comparison, without carrying out inferential analysis; there is no empirical evidence to show that one model is superior to another; however, what has been observed could make us think that there are no revealing differences between both management models.
CONCLUSIONS
The results showed that a PPP modality health facility such as the HABT does not seem to present better results than a traditional format facility such as the HLNV. The hospital efficiency indicators seem slightly more favorable in a traditional format model compared to the PPP management model, highlighting the hourly medical performance. The financial management indicators favored both models, however, the PPP management modality showed a budget execution three times higher compared to the traditional management model. Finally, the general satisfaction of the user of a health establishment with a PPP management model was higher compared to the traditional model.
Authorship contributions: HDZR: conceived the research idea, manuscript design,
data analysis and interpretation, as well as the preparation of the paper.
Funding sources: self-financed study.
Conflicts of interest: the author declares no conflict of interest.
Received: 15 December, 2021
Approved: 26 February, 2022
Correspondence: Humberto Dario Zinelli Reyes
Address: Calle Antero Aspilaga Nº 130, San Isidro, Lima.
Telephone number: 948194408
E-mail:huzanelli@hotmail.com
REFERENCES
