CASE REPORT
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2023 - Universidad Ricardo Palma10.25176/RFMH.v23i1.5309
GASTROINTESTINAL STROMAL TUMOR (GIST) IN JEJUNUM
TUMOR DEL ESTROMA GASTROINTESTINAL (GIST) EN YEYUNO
Alessandra Canelo
 1,a, Alejandro Llanos-Salirrosas
1,a, Alejandro Llanos-Salirrosas
 1,a, Elver López
1,a, Elver López
 1,a, José
Mantilla
1,a, José
Mantilla
 1,a, Lucero Mejía
1,a, Lucero Mejía
 1,a, Sharon Polo
1,a, Sharon Polo
 1,a
1,a
1Facultad de Medicina de la Universidad Nacional de Trujillo, Trujillo, Perú.
aEstudiante del cuarto año de Medicina.
ABSTRACT
Gastrointestinal stromal tumors (GIST) are mesenchymal neoplasms that represent less than 3% of gastrointestinal neoplasms, with an incidence of 1 to 2 cases per hundred thousand inhabitants. It originates more frequently in the stomach and small intestine and is characterized by the expression of the tyrosine kinase growth factor receptor, CD117. Therefore, its diagnosis requires an immunohischemical study to rule it out from other mesenchymal tumors. However, enteroscopic imaging and analysis of the biopsy may suggest a preoperative diagnosis of probable GIST. The case of a 62-year-old woman with rectorrhagia and recurrent anemia caused by mid-intestinal bleeding observed by capsule endoscopy is reported. Enteroscopy revealed a subepithelial ulcerated lesion in the proximal jejunum, and a biopsy was taken, the anatomopathological study of which suggested a gastrointestinal stromal tumor. The biopsy sample subjected to immunohistochemical studies confirms the suspicion of a cKit/CD117-positive GIST tumor. Surgical resection of the tumor with dimensions 4.2x3 cm is performed. After surgery, the patient was stable and under clinical follow-up until she was discharged. Clinical findings, diagnosis and timely treatment contribute to increasing survival from complications.
Keywords: Gastrointestinal stromal tumor; cKit/CD117; midgastrointestinal hemorrhage. (Source: MeSH NLM).
RESUMEN
Los tumores del estroma gastrointestinal (GIST) son neoplasias mesenquimales que representan menos del 3% de las neoplasias gastrointestinales, con una incidencia de 1 a 2 casos por cien mil habitantes. Se origina con mayor frecuencia en el estómago e intestino delgado y tiene como característica la expresión del receptor de factor de crecimiento de tirosina kinasa, CD117, por lo tanto, su diagnóstico requiere de un estudio inmunohisquímico para descartarlo de otros tumores mesenquimales. Sin embargo, el estudio de imagen por enteroscopia y el análisis de la biopsia puede sugerir un diagnóstico preoperatorio de probable GIST. Se reporta el caso de una mujer de 62 años con rectorragia y anemia recurrente causada por hemorragia intestinal media observada por capsula endoscópica. En la enteroscopia se evidencia una lesión ulcerada subepitelial en yeyuno proximal, y se procede a tomar biopsia cuyo estudio anatomopatológico sugiere tumor del estroma gastrointestinal. La muestra de biopsia sometida a estudios inmunohistoquímicos confirma la sospecha de tumor de GIST positivo para cKit/CD117. Se realiza la resección quirúrgica del tumor con dimensiones 4,2x3 cm. Posterior a la cirugía la paciente se encontraba estable y bajo seguimiento clínico hasta ser dada de alta. Los hallazgos clínicos, el diagnóstico y el tratamiento oportuno contribuyen a aumentar la supervivencia ante las complicaciones.
Palabras Clave: Tumor del estroma gastrointestinal, cKit/CD117, hemorragia digestiva media. (Fuente: DeCS BIREME).
INTRODUCCION
Gastrointestinal Stromal Tumors (GIST) are sarcomas that originate in the interstitial cells of Cajal (1); which are located within the muscle layer and are pacemaker cells of the gastrointestinal tract responsible for its motility (2).
They are mostly caused by oncogenic mutations in the receptor tyrosine kinase (KIT gene) and smaller fractions have mutations in the Platelet Derived Growth Factor Receptor Alpha (PDGFRA) gene (3), which encode members of the family of type III transmembrane receptor tyrosine kinases, central regulators of cell proliferation, differentiation and apoptosis pathways (1).
GISTs are rare and represent 1% to 2% of neoplasias. gastrointestinal (4). They can occur anywhere in the tract gastrointestinal (5); however, they are more frequent in the stomach (51%), followed by the small intestine (36%), the colon (7%), the rectum (5%) and the esophagus (1%) (2). It has a incidence of one to two per 100,000 individuals and a prevalence of 13 per 100,000 individuals, of which which men and women are equally affected (5). These tumors can arise at any age and are most common in people between the ages of 40 and 70, with a median age of 65 years (4,6).
CASE REPORT
It should be noted that the patient gave his informed consent for the report's publication. The article has been reviewed by the ethics committee and institutional permission for publication by the Hospital Regional Docente de Trujillo (HRDT).
A 62-year-old female patient from Magdalena de Cao, with a history of hospitalization at the Hospital Regional Docente de Trujillo (HRDT) from September 10 to 24, 2022, due to fainting, rectal bleeding (twice), hematemesis (three occasions) and abdominal swelling causing acute post-hemorrhagic anemia. Two globular packages were administered. An upper digestive endoscopy was performed, which failed to show evidence of a lesion causing bleeding in the esophagus, stomach, and duodenum. The colonoscopy showed the mucosa of the cecum and rectum conversed without evidence of lesions, and a CT scan revealed a solid nodule with uptake of the substance. of contrast of exophytic growth in the jejunal wall, which suggests ruling out a GIST tumor. (Figure 1)

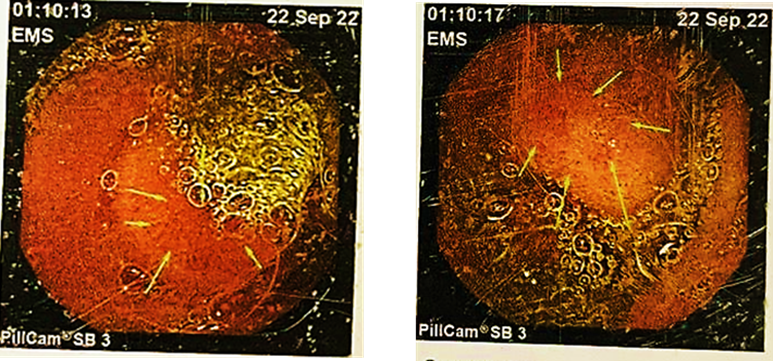
Likewise, an endoscopic capsule examination was performed, finding a lesion with an ulcerous impression and a subepithelial appearance. The HRDT did not have the capacity to perform an enteroscopy that could obtain a biopsy to rule out GIST tumor. (Figure 2)
The recommendations and treatment for discharge were a soft diet and control by an external gastroenterology clinic in 2 weeks.
On October 2, the patient went to the HRDT Emergency Department due to transrectal bleeding of approximately 500cc, vinous red in color and with foul-smelling clots with an evolution time of one day. She was referred to the gastroenterology service for observation and evaluation. On the day of admission, a globular package was administered, giving treatment with omeprazole (40 mg IV every 12 hours for 5 days), dimenhydrinate (50 mg IV Pro Re Nata for 5 days) and tramadol (100 mg via EV Pro Re Nata for 5 days). Two days after the date of admission, he presented 8.9g of hemoglobin and 27.2% of hematocrit. Four days later, his hemoglobin was 11.5% and his hematocrit was 35%; therefore, he was discharged with the diagnosis of inactive midgut bleeding with soft diet treatment, 20cc lactulose orally every 24 hours and referral to Chiclayo for his enteroscopy.
On October 14, an enteroscopy was performed at the Lambayeque Regional Hospital where an ulcerated subepithelial lesion of approximately 3cm in diameter was found with deep ulceration at its apex whose bed presented fibrin and remains of necrosis in the proximal jejunum. A biopsy is taken and surgical treatment is suggested.
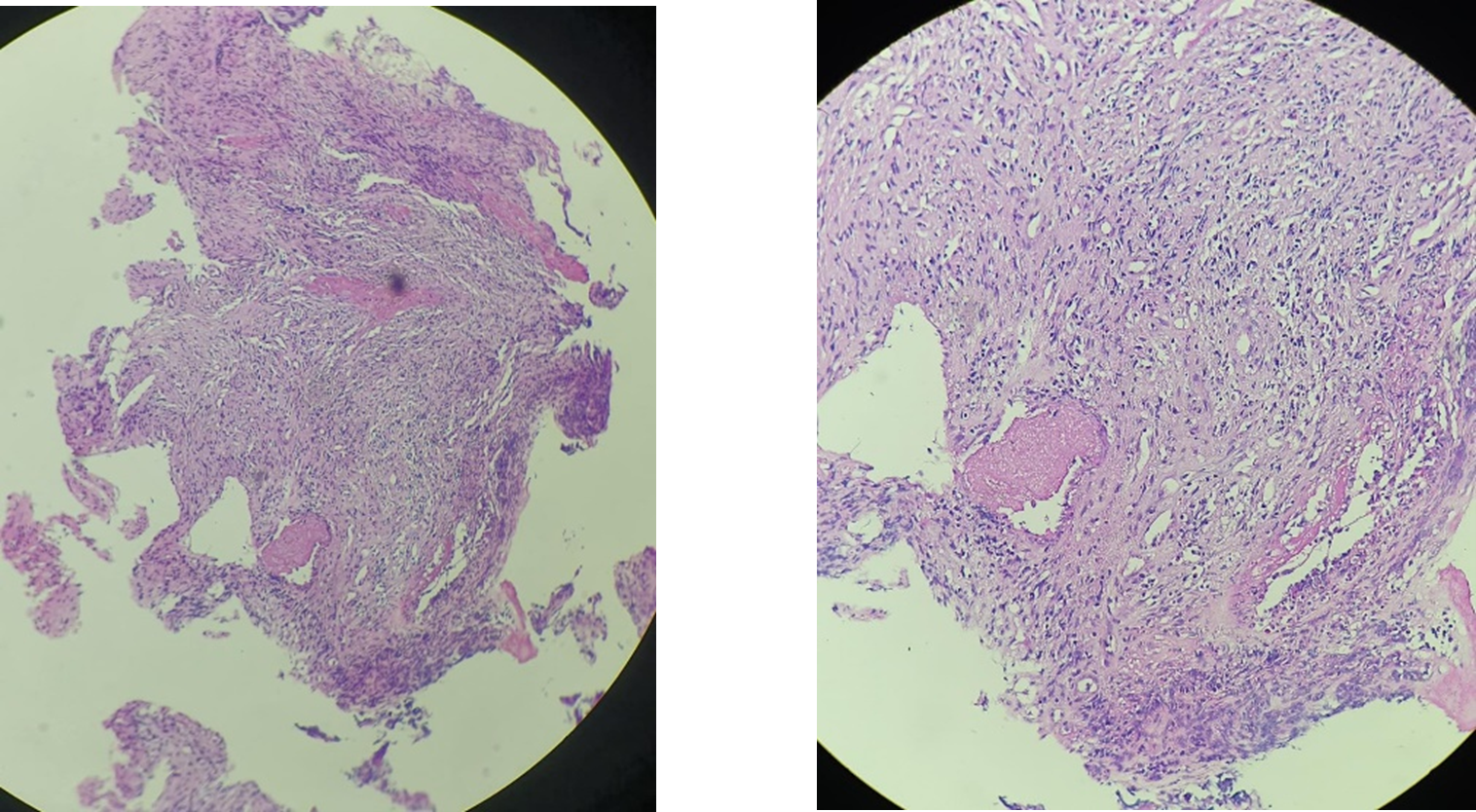
In the anatomopathological study, a spindle cell neoplasm suggestive of a GIST tumor was diagnosed and an immunohistochemical study was indicated to define the lineage of the proliferating cells. (Figure 3)
For the surgery, she was referred to the Instituto Regional de Enfermedades Neoplásicas Norte (IREN Norte) and was admitted as an emergency on November 2 for presenting her 4th rectal bleeding of approximately 250cc. In total, the patient received 7 red blood cells since the onset of the disease.
On November 6, resection of the jejunal GIST tumor was performed. Among the operative findings, a tumor was found 15 cm from the angle of Treitz, a 4x3cm proliferative, extraluminal lesion that compromised 50% of the circumference of the intestinal wall of the first jejunal loop, for which we proceeded with the resection of 4 cm of intestine.
After the surgical procedure, the patient is stable and is hospitalized for follow-up until she is discharged.
The immunohistochemical result of the sample showed a positive gastrointestinal stromal tumor (GIST) for cKit/CD117. (mitotic rate <5 /5 mm). Spindle cells arranged in fascicles of intermediate cellularity with sectors of necrotic and hemorrhagic tissue, moderate-risk lesion with a size of 4.2 cm.
DISCUSSION
GISTs are the most frequent mesenchymal neoplasms of the gastrointestinal tract, representing 0.1 to 3% of digestive tumors. Its incidence varies from 1 to 1.5 cases per 100,000 subjects per year; their age of presentation belongs to the range of 50 to 65 years and they are located in the hollow digestive viscera (80%) and in the retro-peritoneum and minor pelvis (10%) (7,9). In addition, they originate in the interstitial cells of Cajal of the intestinal nerve centers (myenteric plexus) by an activating mutation of the KIT (60-85%) and PDGF (10-15%) tyrosine kinase receptors (10).
In this case report, the patient is a 62-year-old woman who suffers from digestive hemorrhage in the midgut, in addition to partial obstruction and chronic bleeding. It should be noted that approximately 70% of GIST cases are symptomatic at diagnosis, but there is a small percentage that requires emergency surgery as in this case (8). Likewise, the manifestations depend on three parameters, their location, aggressiveness and size. Tumors smaller than 2 cm are usually asymptomatic, limited to the colonic wall, and visible at endoscopy as small submucosal masses (11). Among the operative findings of the case, a tumor was found 15 cm from the angle of Treitz, a 4x3 cm extraluminal proliferative lesion that compromised 50% of the circumference of the intestinal wall of the first jejunal loop.
The most common complication of large GISTs is gastrointestinal bleeding secondary to mucosal ulceration, as occurred in this case, the main reason for the patient's consultation being rectal bleeding caused by the pelvic mass. Because GISTs range from benign to highly aggressive, risk stratification schemes based on prognostic factors such as size, site of origin, mitotic count, and proliferation index have been proposed (12). Also, the diagnosis of bleeding jejunal GISTs is challenging due to their inaccessibility by endoscopy; for this reason, the immunohistochemical analysis of the samples was chosen, where they expressed CD117 (95%), CD34 (60-70%) and smooth muscle actin alpha (20-40%), as well as positive vimentin and negative desmin to differentiate them. of melanomas and plasmacytomas (13). And, given the finding of nonspecific abdominal pain and other nonspecific gastrointestinal signs and symptoms, gastrointestinal bleeding, resistance to treatment, and coexistence of an abdominopelvic mass, this type of tumor should be considered in the differential diagnosis. Timely diagnosis and treatment will help improve the patient's chances of survival.
ACKNOWLEDGMENTS
To doctors Calvo Arana Héctor, Requena Fuentes Víctor Raúl and Diaz Plasencia Juan Alberto, for giving us their valuable support and collaboration in the development of this research work.
Contributions Author: All authors provided the idea. LM prepared the format of the
manuscript. JM, SP, and ML contributed to data collection,
analysis, and manuscript preparation. ALS and AC participated in the data collection, analysis
and preparation of the
figures of the manuscript.
Financing: Self-financed.
Conflicts of interest: No conflicts of interest are declared.
Received: 09/12/2022.
Approved: 12/01/2023.
Correspondent author: Jose Alejandro Mantilla García.
Adress: Los diamantes 471 urbanizacion Santa Ines.
Phone: (+51) 995492358
E-mail: jmantillag@unitru.edu.pe
Article published by the Journal of the faculty of Human Medicine of the Ricardo Palma University. It is an open access article, distributed under the terms of the Creatvie Commons license: Creative Commons Attribution 4.0 International, CC BY 4.0(https://creativecommons.org/licenses/by/1.0/), that allows non-commercial use, distribution and reproduction in any medium, provided that the original work is duly cited. For commercial use, please contact revista.medicina@urp.edu.pe.
BIBLIOGRAPHIC REFERENCES