EDITORIAL
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2021 - Universidad Ricardo Palma10.25176/RFMH.v23i1.5534
IMPORTANT ADVANCES IN REGENERATIVE MEDICINE. A VISION TO THE FUTURE OF OPHTHALMOLOGY
AVANCES IMPORTANTES EN MEDICINA REGENERATIVA. UNA VISIÓN AL FUTURO DE LA OFTALMOLOGÍA
Dr. Rafael Iván Hernández
 1,2, Dr. Eduardo Alan Borobio Guede
1,2, Dr. Eduardo Alan Borobio Guede
 2,3, Catherine Suárez Egóavil
2,3, Catherine Suárez Egóavil
 1,2
1,2
, Dr. Jhony A. De La Cruz Vargas
 1,2
1,2
1Instituto de investigaciones en ciencias Biomédicas. Facultad de Medicina Humana, Universidad
Ricardo Palma. Lima,
Perú.
2Instituto peruano de ingeniería celular y manufactura tisular A.C. – INGECEL. Lima, Perú
3Oftalmología avanzada S.R.L. Lima, Perú.
The treatment of corneal lesions continues to be a topic of great interest. However, despite the development of new technologies and due to the slow evolution and uncertain healing of corneal lesions, they still represent a public health problem since patients can be affected for life, affecting the family and the health system due to the costly and uncertain response to treatment. For this reason, the need arises to seek therapeutic alternatives to treat these patients.
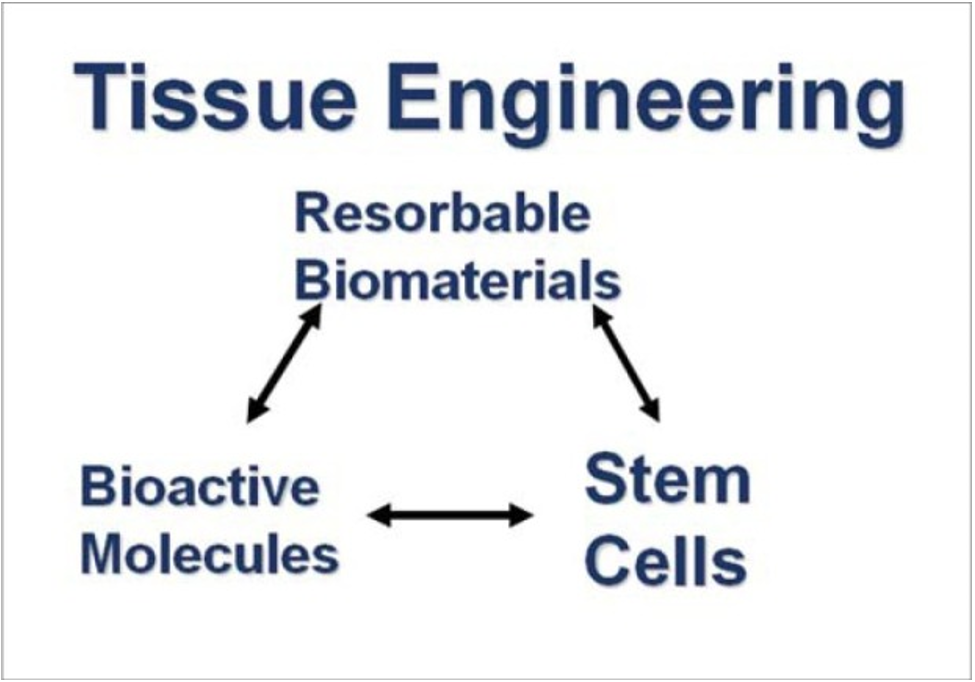
Cellular therapy based on bioactive molecules, scaffolds, an d stem cells is a rescue treatment for lesions with a torpid evolution. We must be present in the current context, where regenerative medicine today is changing the perspective of the traditional concept of "fighting the disease" and the increasingly actionable paradigm of "restoring health"1. Currently, we dare to say that there is no important educational Medical Institution that does not have a team dedicated to research in this area (Figura 1), since, although we can indeed generate bioactive molecules through manufacturing and scaffolding with 3D technology, cells are the high point within this triad2 (Figura 2).
In this sense, the Universidad Ricardo Palma is no stranger to these advances; and it is that, through the Instituto de Investigaciones en Ciencias Biomédicas (INICIB), articulated with other faculties and national and international health institutions, it has been developing protocols, processes pre-clinical and clinical studies within its tissue engineering laboratories for 4 years.
After working with autologous bioactive molecules, it was possible, under research protocols, to recover traumatic corneal lesions initially in rabbits3 and later in humans4.
Nowadays, at the INICIB of the Universidad Ricardo Palma, using state-of-the-art technology and with adequate human resources for these purposes (RENACYT-CONCYTEC researchers), we are taking an important step by leading a pilot study of clinical experience with the objective of determining the clinical efficacy of the systematic use of CD34+ and CD 105+ stem cells from autologous bone marrow in the repair of traumatic lesions of the corneal surface that are candidates for corneal transplantation.
This pilot clinical experience study measured best-corrected visual acuity on admission using slit-lamp biomicroscopy, corneal optical coherence tomography, and fluorescence testing. Mononuclear cell eye drops obtained and isolated from bone marrow with a CD 34+ cell count greater than 900cel/um and by flow cytometry were applied to all of them under protocol.
We can say that the recovery of vision, in this preliminary progress, measured with the tests described, has been satisfactory and promising without the need for a transplant or any subsequent bloody procedure. This work is the product of a project financed by the INICIB - Universidad Ricardo Palma and the ophthalmology institutes involved, where we formally set a precedent for the preliminary results that support us.
Correspondence: Dr. Rafael Iván Hernández.
Address: INICIB, Facultad de Medicina Humana, Edificio I-208. 2do piso. Avenida
Benavides 5440, Surco, Lima-Perú.
Telephone number: 708-0000 / Anexo: 6016
E-mail: ivan.hernandez@urp.edu.pe
Article published by the Journal of the faculty of Human Medicine of the Ricardo Palma University. It is an open access article, distributed under the terms of the Creatvie Commons license: Creative Commons Attribution 4.0 International, CC BY 4.0(https://creativecommons.org/licenses/by/1.0/), that allows non-commercial use, distribution and reproduction in any medium, provided that the original work is duly cited. For commercial use, please contact revista.medicina@urp.edu.pe.
BIBLIOGRAPHIC REFERENCES