EDITORIAL
DOI 10.25176/RFMH.v19.n1.1799LINGUA CONDYLOMA: CASE REPORT PRESENTATION AND LITERATURE REVIEW
CONDILOMA VIRAL EN LENGUA: PRESENTACIÓN DE UN CASO CLÍNICO Y REVISIÓN BIBLIOGRÁFICA
Rubén Rozas-Llerena1,a,
Raúl Sebastian-Ayala1
1 Facultad de Medicina Humana, Universidad Ricardo Palma, Lima-Perú.
a Anatomopatólogo.
ABSTRACT:
The acuminated condyloma is a sexually transmissible disease caused by the Papilomavirus (HPV). It is
frequently found in the anus-genital region and rare in the mouth cavity. However, the increase of the oralsexual
activity has even more favored the occurrence of the PVH in the oral mucous. This report describes a
condyloma I the oral cavity (tongue) of a 43 year old man with a history of oral sex practice, which diagnostic
was confirmed by a biopsy.
Key words: Epithelioid hemangioendothelioma. (source: MeSH NLM)
RESUMEN:
El condiloma acuminado es una enfermedad de transmisión sexual causada por el virus del papiloma
(VPH). Se encuentra con frecuencia en la región ano-genital y es poco frecuente en la cavidad bucal.
Sin embargo, el aumento de la actividad sexual oral ha favorecido aún más la aparición de PVH en la
mucosa oral. Este informe describe un condiloma en la cavidad oral (lengua) de un hombre de 43 años con
antecedentes de práctica sexual oral, cuyo diagnóstico se confirmó mediante una biopsia.
Palabras clave: Hemangioendotelioma epitelioide. (fuente: DeCS BIREME)
INTRODUCTION
Condyloma is a term to describe a sexually transmitted disease, which is transmitted by the human papilloma virus (HPV) also is called condylomata acuminata, a similar lesion to an irregular meaty wart. This disease affects men and women who are sexually active. It is spread by sexual, anal, oral, and vaginal contact with infected people. This virus is usually contagious however there is no evidence of being infected, the wart-like or condylomata-like lesions appear on a lower percentage with visible lesions on the penis, vulva, cervical neck, anus and even in the oropharynx cavity. The diagnose is made by biopsy, removing the complete lesion. Avoid partner exchange, use a condom, performing a Pap smear cytological diagnosis are preventive measures.
CASE REPORT
43-year-old male patient, who refers in the last 6 months has noticed a small lump on the back of the tongue, with slow growth, painless and currently refers that the tumor measures 4 cm diameter, no other hassles.
The physical exam is noticing an injury in dorsal region tongue raised grayish color, ragged edges, no ulcerated and measuring 4 cm diameter
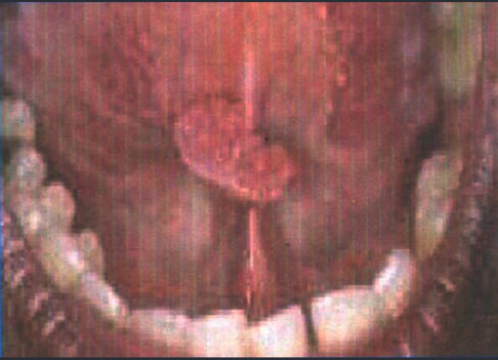
Figure 1. Macroscopy
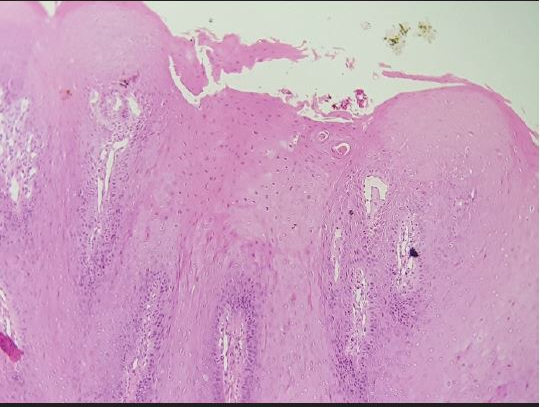
Figure 2. Microscopy: Hyperkeratosis, Parakeratosis, Acanthosis, Papillomatosis, Choilocytes.
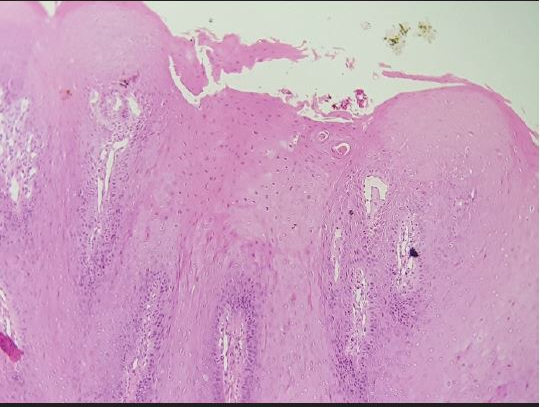
Figure 2. Microscopy: Hyperkeratosis, Parakeratosis, Acanthosis, Papillomatosis, Choilocytes.
DISCUSSION
The Human Papilloma Virus (HPV) is a DNA virus from the Papovaviridae family, of the genus Papilloma virus.
More than 160 different genotypes have been described, which are defined by the variability of their Eg, L1 genes. The incubation period varies from 3 weeks to 8 months with an average of 3 months.1-4 Clinically the papilloma virus presence is often seen in the superior lip, lingual frenulum, back of tongue as in the present case, lower lip and commissures.5-8 Condylomas are the most frequent clinical lesions which are characterized by having the cauliflower formation or present as common warts. The transmission route is caused by HPV-infected orogenital practices from more than 100 HPV genotypes, 16 have been found with oral lesionss1,2,3,4,6,7,10,11,13,16,18,31,32,33,35,57; the 13 and 32 are oral cavity exclusive. Most of those viruses, are low risk (not oncogenic) associated to benign papillomatous lesions: 6 and 11 are associated with buccal papilloma, 6 and 4 to common wart, 11 to condylomata acuminata, 13 and 32 to focal epithelial hyperplasia(with progression malignant low potential) In contrast, high-risk genotypes (oncogenic) such as 16, 18, 31, 33 and 35 are associated with leukoplakia and squamous cell carcinoma. Types 16 and 18 are found in most oral squamous cell carcinomas (80%), while genotypes 31,33 and 35 are less frequent (3%). Tobacco and alcohol have been shown to be oral cancer associated factors9,10,11,12,13.
To diagnose the appropriate identification of the viral types the following techniques are used:
- In situ hybridization
- The Southern Blot test
- The polymerase chain reaction technique (high sensitivity range) can detect less than a DNA viral copy per cell
CONCLUSION
The patient presented non conclusive clinical manifestations of viral condyloma due to HPV, therefore biopsy was performed for proper diagnosis.
It is important to take a complete medical history where sexual habits and customs are questioned in both women and men.
Authorship contributions: The authors participated in the conception, design, writing, critical review and approval of the final version of the article.
Financing: Self-financed.
Conflict of interest: The authors declare not having any conflict of interest in this article publication.
Received: November 07, 2018
Approved: December 18, 2018
Correspondence: Rubén Rozas Llerena
Address: Calle Monserrate Este-Urb. The Gardenias Santiago de Surco
Telephone: +51 999725616
Email: rubenrozasllerena1@hotmail.com
BIBLIOGRAPHIC REFERENCES
- Delgado Quiñones EG. Residente Medicina Familiar. Instituto Mexicano del Seguro Social (1955) Guadalajara Jalisco. México
- Profesora Titular Curso de Especialización en Medicina Familiar IMSS. México
- Director del Centro de Investigacion Educativa y Formacion Docente. IMSS. Jalisco. México
- Médico Encargado de APAEDOM – ISSSTE. Jalisco. México
- Palma I. Epidemiología del virus del Papiloma Humano. Rev Paceña Med Fam 2006; 3(4):67-70.
- Fernandez E, Obanza W. Condiloma Acuminados. Guías Clínicas 2003; 3 (33)
- Ronell E. Bologna-Molina R; Castañeda-Castaneira N.Virus del Papiloma humano y su asociación con cáncer bucal. Rev. Med. Inst. Mex Seguro Soc 2006; 44 (2): 147 – 153
- Carr J, Gyorfi T. Human papilloma virus. Epidemiology, transmission and pathogenesis. Clin Lab Med 2000; 20: 235 – 255
- Lazzari CM, Krug LP, Quadros OF, Baldi CB, Bozzetti MC, Human papillomavirus frequency in oral ephitelial lesions. J Oral Pathol Med 2004; 33 (5): 260 – 263.
- Premoli-de-Percoco G, Christensen R, Human Papillomavirus in Oral Verrucal-PApillary Lesions. Pathologica 1992; 84:383-92
- Camargos AF, Hugo de Melo V. Ginecología ambulatorial. Belo Horizonte: Coopamed; 2001 : 397 – 400.
- Tatti SA, Belardi G, Marini MA, Eiriz A, Chase LA, Ojeda J et al. Consenso en la metodología diagnóstica y terapéutica para las verrugas anogenitales. Revista Obstetricia y Ginecología Latino – americanas 2001; 59 (3): 117 – 31.



