ARTÍCULO ORIGINAL
DOI 10.25176/RFMH.v19i3.2166
1 Emergency Department, Rebagliati-EsSalud Hospital, Lima-Peru.
2 Department of Medicine, Almenara-EsSalud Hospital, Lima-Peru.
3 Faculty of Medicine, National University of San Marcos, Lima-Peru.
4 Research Center of the University of San Martín de Porres, Lima-Peru.
a Internist physician.
b Emergency physician.
c Licentiate nurse.
d Magister in teaching and research about health.
e Doctor of medicine.
ABSTRACT
Introduction: Patients with chronic terminal
disease frequently come to emergency department of reference hospitals. Objectives: To determine frequency of chronic terminal disease in patients admitted to emergency department, identify invasive procedures and compare oncological with non-oncological patients. Methods: Cross-sectional study in patients older than 18 years old, admitted to emergency department of a tertiary hospital, November 2017. Criteria for terminal disease: Clinical stage IV cancer, severe cognitive deterioration or total functional dependence plus diagnosis of dementia, neurological sequelae, dependence of oxygen, glomerular filtration rate <30 ml / min, Child C cirrhosis, or left ventricular ejection fraction <20%. Statistical analysis with Mann-Whitney U and Chi square tests. Results:10.7% (172 of 1604 admissions) of admitted patients presented criteria of chronic terminal disease, with oncological cause 21.5% (37/172) and non-oncological 78.5% (135/172). In oncological patients, the median age was 70 years and was female 59.5%, while in non-oncological 84 years and 57% of women (p <0.01 and 0.79, respectively). 41% (71/172) were admitted by shock-trauma unit, more frequently due to drowsiness and dyspnea. Invasive procedures, probably unnecessary, were identified in 21.5% (37/172 patients), orotracheal intubation and central venous catheter for inotropic were the most frequent. The average stay in emergency department was eight days, with 32% of oncological deaths and 24% of non-oncological deaths in emergency department (p = 0.43). Conclusions: 10% of patients admitted to the emergency department of a tertiary hospital have chronic terminal disease, with a greater frequency of non-oncology, probably performing unnecessary procedures in one fifth of these.
Keywords: Chronic terminal disease, admission, emergency department.source: MeSH NLM)
RESUMEN
Introducción:Pacientes con enfermedad crónica terminal acuden con frecuencia a emergencia de hospitales de referencia. Objetivos: Determinar la frecuencia de enfermedad crónica terminal en pacientes admitidos a emergencia, identificar procedimientos invasivos y comparar oncológicos con no oncológicos. Métodos:Estudio de corte transversal, en mayores de 18 años admitidos a emergencia de un hospital terciario, noviembre 2017. Se consideró enfermedad terminal al cáncer en estadio clínico IV, deterioro cognitivo severo o dependencia funcional total más diagnóstico de demencia, secuela neurológica, dependencia de oxígeno, índice de filtración glomerular < 30 ml/min, cirrosis hepática Child C o fracción de eyección ventricular izquierda < 20%. Análisis estadístico con U de Mann-Whitney y Chi cuadrado. Resultados: El 10,7% (172 de 1604 admisiones) de los pacientes admitidos presentaron criterios de enfermedad crónica terminal, de causa oncológica 21,5% (37/172) y no oncológica 78,5% (135/172). En oncológicos la mediana de edad fue 70 años y sexo femenino 59,5%, mientras que en no oncológicos 84 años y 57% de mujeres (p<0,01 y 0,79 respectivamente). El 41% (71/172) ingresó por unidad de shock trauma, con mayor frecuencia por somnolencia y disnea. Se identificó procedimiento invasivos probablemente innecesarios en 21,5% (37/172 pacientes), intubación orotraqueal y catéter venoso central para inotrópicos fueron los más frecuentes. La estancia promedio en emergencia fue ocho días, falleciendo en emergencia 32% de oncológicos y 24% de no oncológicos (p=0,43). Conclusiones: El 10% de los pacientes admitidos a emergencia de un hospital terciario presenta enfermedad crónica terminal, con mayor frecuencia no oncológica, realizándose procedimientos probablemente innecesarios en la quinta parte de estos.
Palabras clave: Enfermedad crónica terminal, admisión, servicio de emergencia. (fuente: DeCS BIREME)
INTRODUCTION
The emergency service (Urgency) of a hospital is designed and equipped to provide immediate assistance to patients with health problems that may be life-risking or that may produce incapacitating sequelae. The main objective of this service is to save the patient’s life, stabilizing him/her for further definitive treatment1.
In recent decades, the increase in the demand for care, due to population increase (because of technological progress, epidemiological transition and migration) has produced saturation of these services, mainly in the large reference hospitals, predominantly old-aged patients with chronic complex diseases, diverting diagnostic and therapeutic efforts2,3.
In an international level, some criteria have been defined for the final or terminal phase of chronic diseases (oncological and non-oncological) where irreversible damage has occurred, with multiple symptomatology, limited life prognosis and a great emotional impact for the patient, his/her family and the health staff. WHO recommends palliative care in this phase of the disease and international organizations have specified that certain invasive procedures are unnecessary, rather than helping the patient, prolong their suffering and the family’s4-6.
The frequency of terminal illness in emergency services is variable and underestimated6; Studies carried out in North America, Europe and Asia have shown that the use of palliative care in patients with terminal illnesses (institutionalized and home follow-up), reduces hospital admissions, admissions to intensive care and frequent visits to urgency room, with no significant difference in the survival time of these patients; greatly improving patient and family conditions7-14. Nevertheless, there is also a high frequency of care of these patients in emergency room, where many die without receiving palliative care15,16.
In Latin America and Peru there are fewer reports on this. In our environment the following items were reported: an important frequency of end-stage disease (30%) among the patients readmitted to emergencies during last year, prolonged hospital stay, frequent readmission and a high mortality rate2,3,17,18.
This reflects problems in the national health system, with a deficiency in the focus of palliative care, being part of the solution to improve the selection of patients and refer these patients to adequate services, avoiding subjecting them to unnecessary procedures in emergency services and provide a better quality of life to these patients and their families, without therapeutic extreme cruelty11,19,20. This means integrating emergency palliative care, as has been done in Europe, Oceania and North America4,21,22.
The objective of this study is to determine the frequency of chronic terminal illness in patients admitted to the emergency service of adults of a tertiary hospital, to identify the types of disease and invasive procedure established.
METHODS
Cross-sectional study in patients older than 18 years of age admitted to emergency at a tertiary hospital in Lima-Peru, which has 200 observation beds and reported 164370 attentions and 22883 admissions per year in 20152. The sample was collected between November 1 and 30, 2017.
A terminal oncological disease was considered to be a histological diagnosis confirmed in clinical stage IV or multiple cerebral, hepatic or pulmonary metastases. In non-oncological patients, it was considered a terminal illness if it presented severe cognitive damage (Pfeiffer test) or total functional dependence (Katz scale) plus diagnosis of dementia, neurological sequelae, renal failure with glomerular filtration rate <30 ml / min, respiratory disease with continuous home oxygen, stage C liver cirrhosis of Child-Pugh scale or heart failure with left ventricular ejection fraction < 20%15,16,23,24. The following patients were excluded: Those with incomplete data, readmitted during follow-up, deceased or transferred before the first 24 hours of admission.
For initial identification of patients, the daily medical reports were reviewed, in the possible participants a clinical history was reviewed and the patient and / or primary caregiver was interviewed / evaluated by one of two nurses trained in the subject. The selected patients were evaluated by one of three emergency service specialists, trained in end-stage disease criteria. The doubts were resolved in consensus with the principal researcher. Follow-up was done in the institutional statistical system.
The data was collected in a card that was pre-designed, coded, typed in Microsoft Excel 2010 and processed with IBM SPSS 25.00. To compare the oncological and non-oncological groups, qualitative bivariate analysis was applied with Chi-square test; in the quantitative variables, Kolmogorov-Smirnov test was applied to identify normal distribution and U Mann-Whitney for independent samples in non-normal distribution. It was considered significant p < 0.05 and 95% confidence interval.
Approval was obtained from the institutional research committee. The patients were evaluated following the principles of good clinical practice and the declaration of Helsinki, with prior verbal informed consent of the patient or primary caretaker.
RESULTS
In the evaluated period, the emergency service registered 14386 attendances and 1604 admissions. We identified 172 patients with criteria of chronic terminal disease (21.5% of oncological cause and 78.5% non-oncological), determining a prevalence of 10.7% of patients with chronic disease in terminal phase among patients admitted to this service. The characteristics of patients according to etiology are presented in Table 1, the age ranged between 19 and 101 years. The most reported pain was abdominal, lumbar and limb pain.
| Characteristics | Oncological (37) |
Non-Oncological (135) |
Total (172) |
P |
|---|---|---|---|---|
| Age in years: middle (IR &) | 70(16) | 84(17) | 79,5(19) | <0,01* |
| Female sex | 22(59,5%) | 77(57%) | 99(58%) | 0,79** |
| In palliative services: | 0,10** | |||
| COPHOES (Spanish Initials for Program of Post Hospital Specialized Control) | 2,7% | 0,7% | 1,2% | |
| PADOMI (Spanish Initials for Program of Home Attention) | 0 | 9,6% | 7,6% | |
| Place of origin: | 0,04** | |||
| • Home | 37%(100%) | 110(81,5%) | 110(81,5%) | |
| • Rest house | - | 18(13,3%) | 18(10,5%) | |
| • Hospital or Clinic | - | 7(5,2%) | 7(4%) | |
| Admission area: | 0,03** | |||
| • Shock Trauma | 9(24,3%) | 62 (45,9%) | 71 | |
| • Medicine | 27(73%) | 61 (45,2%) | (41,3%) | |
| • Surgery/Traumatology | 1(2,7%) | 12 (8,9%) | 88 (51,2%);13 (7,5%) | |
| Reason for admission: | 0,21** | |||
| • Drowsiness | 4 (10,8%) | 30 (22,2%) | 34 | |
| • Dyspnea | 7 (19%) | 20 (14,8%) | (19,8%) | |
| • Pain | 6 (16,2%) | 8 (6) | 27 | |
| • Fever | 2 (5,4%) | 5 (3,7%) | (15,7%);14 (8,1%);7 (4,1) |
Graphic 1, presents the main groups of pathologies. The most frequent specific causes in cancer patients were breast cancer, pulmonary adenocarcinoma and hepatocarcinoma. In the non-oncological: vascular dementia, sequelae of cerebrovascular disease and the total dependent category (without further information on the reason for prostration). Cachexia was identified in 11% of patients with chronic disease in oncological final phase and 13% non-oncological; and pressure ulcers of III or IV degree in 5% of the oncological and 17% of the non-oncological, being their most frequent sacral, heel and trochanter locations.
Graphic 1. Type of disease in terminal phase in patients admitted to emergency of a tertiary hospital.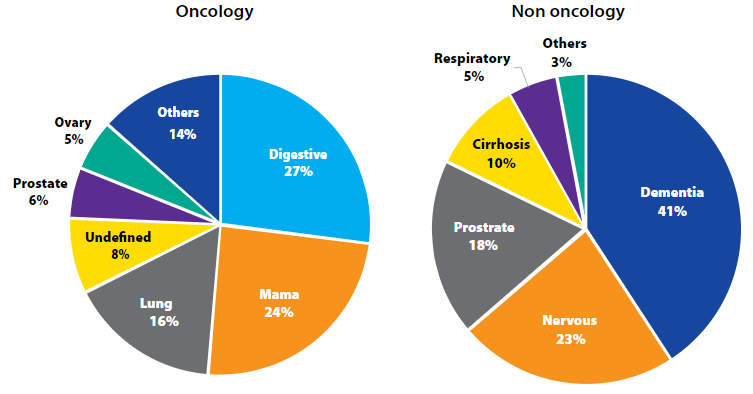
Chronic illness time and terminal illness time were identified in 46% of oncological patients and 21% of non-oncological patients, with a median of 5 months (two months in terminal state) and 02 years (one year in terminal phase) respectively (p = 0.03). Initially, all patients were admitted to common emergency observation rooms, but in the course of their hospitalization, 02 oncological cases (5.4%) and 11 non-oncological cases (8.1%) were transferred to the emergency intermediate care unit, one of which stayed in the intensive care unit for 34 days, where he finally died.
The identified invasive procedures are presented in Table 2. The performance of an invasive procedure, probably unnecessary, was identified in 37 patients with chronic disease in the terminal phase (21.5%), corresponding to 13.5% of the oncological cases and 23,7% of non-cancer patients. The destination of patients with probably unnecessary procedures was high 11%, mortuary 35% and hospitalization 54%.
Figure 2 shows the destination of patients upon leaving the emergency (p = 0.43), we found an average stay in emergency of 8.46 (+/- 5,7) days in oncological and 8,3 (+/- 5,8) days in non-oncological; median 8 and 7 days respectively (interquartile range 7) (p = 0.90).
| Procedure | Oncological (37) |
Non Oncological (135) |
Total (172) |
|---|---|---|---|
| Probably unnecessary | |||
| Orotracheal intubation | 2 (5,4%) | 18 (13,3%) | 20 (11,6%) |
| Inotropic by CVC && | 2 (5,4%) | 18 (13,3%) | 20 (11,6%) |
| Hemodialysis | 1 (2,7%) | 6 (4,4%) | 7 (4,1%) |
| Invasive mechanical ventilation | 0 | 2 (1,5%) | 2(1,2%) |
| Other procedures | |||
| Peripheral venous catheter | 37 (100%) | 135 (100%) | 172 (100%) |
| Nasogastric tube | 5 (13,5%) | 66 (48,9%) | 71 (41,0%) |
| Urinary catheter | 3 (8,1%) | 34 (25,2%) | 37 (21,5%) |
| Paracentesis | 1 (2,7%) | 2 (1,5%) | 3 (1,7%) |
| Thoracic drainage | 1 (2,7%) | 1 (0,7%) | 2 (1,2%) |
| Tracheostomy | 0 | 2 (1,5%) | 2 (1,2%) |
| Other | 3 (8,1%) | 1 (0,7%) | 4 (2,3%) |

DISCUSSION
Patients with chronic diseases in the terminal phase often go to the emergency service of third level hospitals4,14,18,25, an important percentage (41%) did it for the shock trauma unit, an area destined to maintain the patient's life through invasive procedures. A considerable proportion (8%) was sent to a critical care ward (intermediate care), similar to that reported in Australia, with unfavorable results23.
The research was conducted at a single hospital overcrowded patient for a short period of intervention, pertaining to social security (which includes symptoms found were similar to other studies26. Featuring high frequency of pressure ulcers and cachexia, similar to other These patients had a prolonged stay in emergency (eight days), longer than the general stay and the recommended standards2, probably due to deficiencies of the entire health system, almost half of these patients were referred to other inpatient services, where they also remain for a long time and most die18.
The emergency service is an opportunity to identify these types of patients and include them in palliative care programs (ambulatory or domiciliary)16. Although in our environment the offer of palliative care is inadequate and insufficient, this intervention significantly reduced the emergency stay and the admission to other hospital services, including critical units.
An important percentage of invasive procedures considered unnecessary was found, which would prolong the suffering of the patient and is considered inadequate in the quality of the health service. In this regard, there are few publications in our environment, due to lack of staff training and ignorance of the family, which often requires such procedures with the wrong intention to help the patient27. If we consider the approach of palliative care, other minor invasive procedures (intravenous route, nasogastric or bladder tube) should not be performed in patients at the end of life5,9,15.
The admission of patients with terminal illness to the shock trauma unit should be avoided, since unnecessary invasive procedures can increase the suffering of the patient and the family. For this, better communication is needed, rather than making the diagnosis or determining the prognosis at that moment is to detect the antecedent and the life expectancy that many times has already been previously defined.
It is necessary to have trained personnel or consult a palliative care team, before deciding invasive life support measures in patients with well-defined antecedents. However, it is complex, from the ethical point of view and in the country, there are no clear legal bases. This intervention would allow critical areas to be available for patients with other pathologies and needs.
Non-oncological diseases, such as organ failure or neurodegenerative sequelae, were more frequent, similar to that described in other countries. However, they are less studied than oncological cases, despite presenting greater survival and use of health services21,28,29.
The research was carried out in one only hospital with a stacking of patients, during a short period of intervention, belonging to Social Security (which includes approximately 40% of the national population). There is no clear legislation in our midst regarding end-of-life decisions and palliative care, and there are moral doubts in decision-making. Sometimes the information provided was incomplete or contradictory. The knowledge of the patient, family and health personnel regarding criteria of terminality in chronic diseases is not clear, especially in matters related to death.
CONCLUSION
In conclusion, 10% of patients admitted to the emergency in a tertiary hospital have a chronic terminal disease, more often than not oncological, performing probably unnecessary procedures in a fifth of these, with prolonged stay and high death rate.
It is recommended to improve the uptake of patients with chronic disease in a terminal phase, taking advantage of the opportunity of their assistance to emergency services of tertiary hospitals and coordinate with palliative care services for monitoring and control. Evaluating the relevance of invasive procedures in these patients that could prolong the suffering and keep in mind the need to administer palliative care. Train health personnel in the emergency service on these issues or implement a special care system for these patients, integrated into the palliative care unit. At the regional and national levels, it is necessary to promote the palliative approach for chronic, advanced, oncological and non-oncological diseases.
Authorship contributions: José Amado-Tineo: a, b, c, d, f, g; Waldo Taype-Huamaní: a, b, d, e, g; Rolando Vasquez-Alva: b, d, e, g; Fiorella Siccha-Del Campo: b, d, e, g; Teodoro Oscanoa-Espinoza: a, b, c, d, e, g
(a) Conception and design of the work, b) Collection / obtaining of data, c) Statistical contribution, Analysis and interpretation of data, e) Critical review of the manuscript, f) Writing the manuscript, g) Approval of the final version.
Financing: Kaelin Award in health sciences - Research Protocols 2016. Institute of Health Technology and Re-search Evaluation (IETSI) - EsSalud.
Conflicts of interest: The authors declare that they have no conflicts of interest.
Correspondence: José Percy Amado Tineo
Address: Jr. Belisario Flores 238 Dpto 301. Lince, Lima.
Phone: +1990452547
E-mail: jpamadot@gmail.com; jpamadot@hotmail.com
Received: April 06, 2019.
Approved: May 16, 2019.
