ARTÍCULO ORIGINAL
DOI 10.25176/RFMH.v19i3.2167
1 Edgardo Rebagliati Martins-EsSalud National Hospital, Lima-Peru.
a Pediatrician Intensivist of the Pediatric Intensive Care Unit
ABSTRACT
Introduction: Ventilator-associated pneumonia (VAP) increases the risk of mortality by 2 to 3 times. Objectives: To know characteristics of VAP, determining VAP infection rates, analyze related factors, isolated germs, antibiotic sensitivity and mortality.
Methods: Descriptive, retrospective study in patients with VAP 2015-2018. The data was obtained from the Rikchary program of a pediatric intensive care unit, analyzed with SPSS 24.00
Results:There were 60 cases of VAP, with average annual rates of 9.8 per 1000 days of mechanical ventilation (MV). 65% of the VAPs were late, diagnosed after 5 days of MV, 38% were those under 6 months, and those under 3 years of age added 68%, male gender constituted 53%, average MV days were 15, 25% of the patients were re-admitted to MV, the days of central venous catheter 13 and urinary catheter 10.5 days. The average hospitalization was 31 days. 30% of patients were malnourished and 30% post-operated (mainly neurosurgical), 57% had comorbidities, with the prevalent cardiac ones (33%), 45% had neurological disability. The main admission diagnosis was septic shock. The most frequent germs were Stenotrophomona maltophilia sensitive 81% to Cotrimoxazol and Pseudomona aureginosa sensitive 80% to cefepime, 90% to Amikacin and between 50% to 60% to carbapenemens. The mortality was 15%.
Conclusions: The average annual rate of VAP in the evaluated service is within international standards, the most frequent type is late, was more frequent in children under 6 months and male. Malnutrition, congenital heart disease, mechanical ventilation time, days of hospitalization and surgeries were found in a greater proportion in patients with VAP. The most frequent negative gram and 15% mortality.
Keywords: Pneumonia, Ventilator-Associated; Cross Infection; Intensive Care Units, Pediatric (source: MeSH NLM)
RESUMEN
Introducción:La Neumonía asociada a ventilador (NAV) aumenta 2 a 3 veces el riesgo de mortalidad.
Objetivos: Conocer características de NAV, determinando tasas de infección NAV, analizar factores relacionados, gérmenes aislados, sensibilidad antibiótica y mortalidad.
Métodos:Estudio descriptivo, retrospectivo en pacientes con NAV 2015-2018. Los datos se obtuvieron del programa Rikchary, de una unidad de cuidados intensivos pediátricos, se analizó con SPSS 24.00.
Resultados: Se registraron 60 casos de NAV, con tasas promedio anuales de 9.8 por 1000 días ventilación mecánica (VM). El 65 % de las NAV fueron tardías, diagnosticadas después de 5 días de VM, El 38% fueron los menores de 6 meses, y los menores de 3 años sumaron 68%, el sexo masculino constituyó el 53%, los días de VM promedio fueron de 15, reingresaron a VM el 25% de los pacientes, los días de catéter venoso central 13 y de sonda urinaria 10.5 días. El promedio de hospitalización fue 31 días. 30% de pacientes fueron desnutridos y 30% post-operados (principalmente neuroquirúrgicos), 57% tuvieron comorbilidades siendo las cardíacas preponderantes (33%), 45 % tuvo discapacidad neurológica. El diagnóstico de ingreso principal fue choque séptico. Los gérmenes más frecuentes fueron Stenotrophomona maltophilia sensible 81% al Cotrimoxazol y Pseudomona aureginosa sensible 80% al cefepime, 90% a Amikacina y entre el 50% a 60% a los carbapenemens. La mortalidad fue 15%.
Conclusiones: La tasa anual promedio de NAV en el servicio evaluado se encuentra dentro de estándares internacionales, el tipo más frecuente la tardía, Fue más frecuente en menores de 6 meses y sexo masculino. La desnutrición, cardiopatía congénita, tiempo de ventilación mecánica, días de hospitalización y cirugías se encontraron en mayor proporción en pacientes con NAV. Los gram negativos los más frecuentes y mortalidad 15%.
Palabras clave: Neumonía Asociada al Ventilador; Infección Hospitalaria; Unidades de Cuidado Intensivo Pediátrico. (fuente: DeCS BIREME)
INTRODUCCIÓN
Mechanical ventilation is a vital intervention that is commonly used in the critical care setting because of the nature of its invasiveness it’s associated with infectious complications like ventilator associated pneumonia (VAP), which can be defined as hospital acquired pneumonia that occurs in patients after 48 hours of being intubated (tracheostomy or endotracheal intubation) and it wasn’t present at the time of intubation or at the time of admission; or that it is diagnosed within 72 hours after extubation and when mechanical ventilation is stopped1-3.
VAP is one of the most frequent hospital acquired infections in the Pediatric Intensive care unit: children who develop this complication are at 2 to 3 times higher mortality risk, prolonged hospital stays, and increased antimicrobial use (50%) with the associated risk of increased antibiotic resistance3. The mortality attributed to VAP is controversial, due to the vulnerable state of health of patients in the intensive care unit, estimated to be 5-25%. The rates of infection secondary to VAP oscillate between 8-12/1000 days of mechanical ventilation3,4.
VAP continues to be a major public health concern. It occurs through distinct mechanisms, mostly via the endotracheal tube or tracheostomy, but also through aspiration of secretions that colonize the oropharynx, and through hematogenous spread from distant foci of infection or from intestinal flora through bacterial translocation or from contiguous infections that are adjacent to the lungs4. Knowledge of your pathogenesis, epidemiological characteristics and risk factors, allow us to take preventive measures to reduce cases, knowing that the prevention of VAP is a national patient safety objective, as it constitutes an indicator of quality of care4-6.
Early onset VAP occurs during the first four days of mechanical ventilation and generally is caused by pansensitive bacteria. Late onset VAP which develops ≥ 5 days post mechanical ventilation and is caused by Multi-drug resistant organisms (MDR). Early diagnosis and appropriate management of VAP can reduce the emergence of MDR organisms7,8.
Acknowledging this problem will allow us to take preventive measures to reduce infection rates and quality care for our critical pediatric patients9, therefore the main purpose of this study is to recognize the characteristics of ventilator-associated pneumonia in our Pediatric Intensive Care Unit (PICU) in the period 2015 to 2018, determine the rates of NAV infection as well as isolated organisms, its sensitivity and mortality due to VAP.
METHODS
We chose a descriptive, retrospective study of the patients diagnosed with pneumonia associated with fan at the PICU of the Edgardo Rebagliati Hospital Martins (HNERM) between January-2015 and December-2018. The Pediatric Intensive Care Unit of HNERM, attends critical patients of high complexity, transferred from all over the country, it has nine beds for children of ages one month to age fourteen reporting 254, 282, 298 and 318 expenditures per year (2015, 2016, 2017 and 2018 respectively).
The definition of VAP was taken from the Technical Standard of the Ministry of Health of Peru 2016 and the Standard of ESSALUD 2016 surveillance10,11. The infection rate of ventilator associated pneumonia is obtained by dividing the episodes of VAP between the days of mechanical ventilation per 1000. Early VAP is defined as pneumonia less 5 days and late VAP more than 5 days2,12.
The data was obtained from the Rikchary program, a computer program designed to record data of hospitalized patients in the PICU service. He developed a database in Microsoft Excel 2010, and for the analysis descriptive statistics was used with IBM SPSS Statistics 24.00, following the ethical principles of investigation.
RESULTS
Registered 60 cases of ventilator associated pneumonia in the period 2015 to 2018, of a total 1152 expenses, the annual VAP rates are shown in the Figure 1, the total rate of these 4 years being 9.8 cases for 1000 days of mechanical ventilation.
The number of episodes and the total mechanical ventilation time per year are shown in Table 1. Three patients presented two episodes of VAP during his hospitalization in PICU having the times of hospitalization 38, 48 and 207 days each. A patient presented 3 episodes of VAP taking 142 days of hospitalization in PICU.
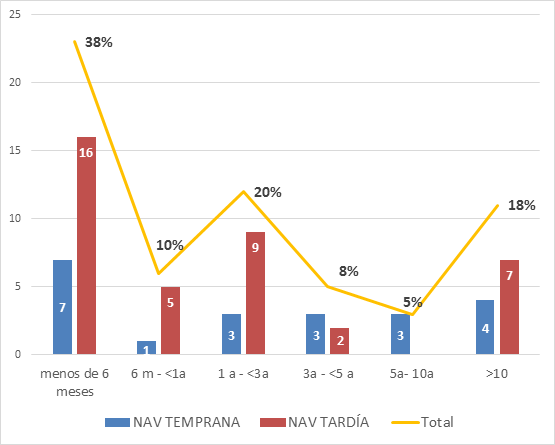
The frequency of early VAP was 21 and late was 39. The median days of presentation of VAP is 7 days in all cases, being 3 days for early VAP and 14 days for late VAP. 53% (32) were male. 38% of the VAPs were presented in children under 6 months, being able to observe in the Figure 3, VAP frequency according to age group in relation to early and late VAP and the total percentage according to age group, having a median age of 15 months (24 months for early VAP and 10 months for late VAP).
The characteristics of factors for VAP are indicated in Table 2. 30% of patients with VAP were malnourished, 30% of patients were post-op and 57% of VAP had cardiac and oncologic comorbidities most frequently, with some others being neurological (5%) and respiratory (5%) comorbidities.
Los principales diagnósticos de ingreso que presentaron los pacientes con NAV se resumen en la tabla N°3. Figure 4 shows the positive cultures isolated tracheal aspirates with VAP. Organisms isolated in patients with VAP and their pattern of sensitivities respectively are shown in table 4 and 5. Nine patients died out of the 60. That were diagnosed with VAP equivalent to 15%.

Tabla 01: Number of cases per year of VAP and days of annual use of Mechanical Ventilation in the Pediatric Intensive Care Unit of Rebagliati Hospital 2015-2018
| 2015 | 2016 | 2017 | 2018 | |
|---|---|---|---|---|
| Expenditures per year | 254 | 282 | 298 | 318 |
| Number of cases VAP* | 15 | 19 | 8 | 18 |
| Days of use VM** | 1390 | 1644 | 1436 | 1440 |
| NAV Temprana (n=21) | NAV tardia (n=39) | Total (n=60) | |
|---|---|---|---|
| Device Days | |||
| VM days * (median) | 11(3-142) | 15,5(3-88) | 15 |
| Days CVC ** (medium) | 12(5-40) | 14(6-43) | 13 |
| Days Foley Probe (medium) | 9( 3- 35 d) | 14(3- 66 d) | 10.5 d |
| Reingresos de VM | |||
| Yes (patient frequency) | 2(3%) | 13(22%) | 15(25%) |
| Nutritional status | |||
| Undernourished | 6(10%) | 12(20%) | 18(30%) |
| Eutrophic | 12(20%) | 22(37%) | 34(57%) |
| Overweight / Obesity | 3(5%) | 5(8%) | 8(13%) |
| Days of hospitalization in PICU# | |||
| Average days and range | 19(8-142 d) | 38(8- 207d) | 31.5 d |
| Post operated | |||
| Yes | 10(17%) | 8(13%) | 18(30%) |
| Surgery | |||
| NeuroQX + | 5(8%) | 2(3%) | 7(11%) |
| CT y CV ++ | 2(3%) | 4(7%) | 6(10%) |
| Abdominal | 3(5%) | 2(3%) | 5(8%) |
| Comorbidities | |||
| Cardiac | 6(10%) | 14(23%) | 20(33%) |
| Oncology and immunosuppression | 4(7%) | 4(7%) | 8(13%) |
| Other | 3(5%) | 3(5%) | 6(10%) |
| Source Service | |||
| Pediatrics | 4(7%) | 8(13%) | 12(20%) |
| Emergency | 11(18%) | 26(43%) | 37(61%) |
| Others | 3(5%) | 3(5%) | 6(10%) |
| Neurological function | |||
| Normal | 8(13%) | 25(42%) | 33(55%) |
| Disability | 13(22%) | 14(23%) | 27(45%) |
| DIAGNOSIS | FREQUENCY | PERCENTAGE |
|---|---|---|
| Septic shock | 12 | 20 |
| Pneumonia | 11 | 18 |
| Heart failure + cardiac malformation | 9 | 15 |
| Convulsive state | 6 | 10 |
| Whooping cough | 4 | 7 |
| Brain tumor | 3 | 5 |
| MAV | 3 | 5 |
| TEC | 3 | 5 |
| Peritonitis | 3 | 5 |
| Post stop | 2 | 3 |
| Others | 4 | 7 |
| Total | 60 | 100 |
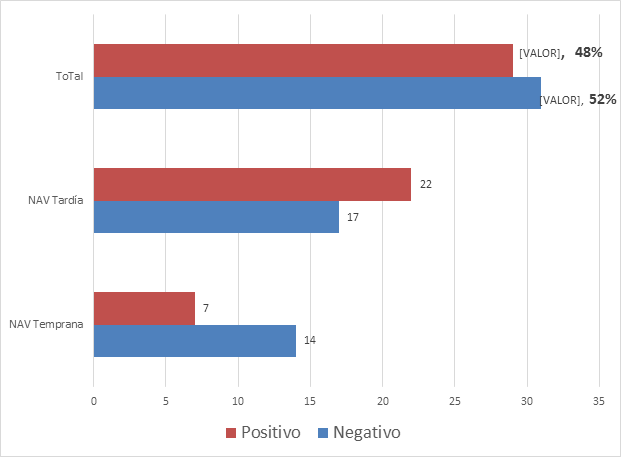
Organisms isolated in patients with VAP and their pattern of sensitivities respectively are shown in table 4 and 5. Nine patients died out of the 60. That were diagnosed with VAP equivalent to 15%.
Tabla N° 4 Isolated organisms in those diagnosed with Ventilator- associated Pneumonia ( VAP) in the pediatric intensive care unit of Rebagliati Hospital 2015-2018.
| GERM | EARLY NAV | LATE NAV | TOTAL | PERCENTAGE |
|---|---|---|---|---|
| Stenotrophomona maltophilia | 3 | 10 | 13 | 45% |
| Pseudomona aureginosa | 1 | 5 | 6 | 21% |
| Klebsiella pneumoniae | 0 | 2 | 2 | 7% |
| Staphylococcus aureus | 1 | 1 | 2 | 7% |
| Acinetobacter iwoffii | 2 | 0 | 2 | 7% |
| Acinetobacter baumannii | 0 | 1 | 1 | 3% |
| Enterococcus faecalis | 0 | 1 | 1 | 3% |
| Escherichia coli | 0 | 1 | 1 | 3% |
| Serratia marcescens | 0 | 1 | 1 | 3% |
| Total | 7 | 22 | 29 | 100% |
| Microorganism | AMK | CTX | CTZ | CEF | CFTX | IMI | MER | CTMX | CIP | PIP/TAZ | COLI | ERT |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| P. AERUGINOSA | 90.5% | 0 | 0 | 78.9% | - | 50% | 62% | - | 95% | 0% | 94.4% | |
| ACINETOBACTER BAUMANI | 0% | - | 0% | 0% | 0% | 0% | 100% | 0% | 0% | - | - | - |
| K. PNEUMONIAE | 100% | - | 25% | 25% | 22% | 100% | 100% | 0% | 50% | 100% | 100% | 100% |
| STENOTROPHONA M | - | - | 63% | - | - | - | - | 81% | 100% | - | - | - |
| E. COLI | 100% | 0% | 33% | 0% | 33% | 100% | 100% | 33% | 33% | 67% | 100% | 100% |
| ACINETOBACTER WOFFI | 100% | - | 0% | 0% | 0% | 100% | 0% | 0% | 0% | - | - | - |
DISCUSSION
The most frequent cause of device associated infection in our PICU is Ventilator associated (VAP), that in the past four years has remained below the standard of 12 per 1000 days of MV, even having a rate of 5.6 in 2017. In Peru, notification of establishments that report in hospital infections since 2005 to date has been increasing every year, as reported in our PICU, the highest incidence rate with device associated infections, corresponded to VAP in adult itensive care unit 11.67 x 1000 days of exposure to mechanical ventilation, while in neonatology it was 5.43 x 1000 days of exposure to mechanical ventilation13
In Spain, through a national Nosocomial Infection Surveillance study with data from 26 pediatric ICUs in 2014, the VAP rate was 8.51/1000 days of MV. However, there are publications with much lower rate, 0.9-2.6 episodes per 1000 days MV, this is due to preventive measures put in place in such institutions, however, in some studies, up to 61 per 1000 days MV3,12,14 are reported.
The classification of early and late VAP allows to look for and avoid some risk factors, and in the case of late VAP, the resistant organisms that were isolated occur due to exposure to previous antibiotics, selective pressure, cross transmission, and colonization of environmental sources of ICU. In our study, 65% of VAPs were late, unlike others who report that approximately more than half of all episodes of VAP occur early. In other studies the early VAP is greater than 70%; this could be due to the results we observed, on the days of hospitalization and MV in our PICU, due to the complexity of the patients we manage, the comorbidities they present, complex surgeries performed, could determine a higher frequency of late VAPs3,8,15.
There are different factors that favor the emergence of the VAP. These are related to extrinsic or intrinsic factors to the host. Age, as an intrinsic factor, is an important factor for VAP. In our results, a higher percentage of patients under 6 months with episodes of VAP are observed, in total those under 3 years constitute 68%, and of these, late VAP is more frequent, coinciding with various reports in which age less than 1 year is an important risk factor for VAP, others report that the age group of 0 to 5 years was twice that of the age group of 5 to 12 years14,15.
Other intrinsic factors are the nutritional status, the presence of comorbidities and neurological function of the patient. In the present study, 30% of patients are malnourished, with a higher percentage of malnourished late NAVs. Obesity and overweight are present in 13% of VAPs; nutritional status directly affects the response to an infectious process and makes them more susceptible to suffering from malnourished patients (malnourished and obese)9. In our study, 18% of malnourished people are registered, which shows that in patients with VAP, malnutrition is much higher. 56% of the VAP were from patients with comorbidities, the most frequent being cardiac patients with 33% and 45% with some degree of neurological disability. The most frequently reported admission diagnosis was the septic schock, being the case that other studies report respiratory distress syndrome (ARDS) as the most frequent3,8,9,16.
Within extrinsic factors, multiple studies have linked a longer duration of mechanical ventilation of 5–11 days, and some consider this the greatest risk factor for VAP, occurring in 94% of cases in the first week of MV. Apostolopoulou et al. reports VAP peaks between day 5 and day 9 of mechanical ventilation. We reported a median of 15-day MV days, the MV days being late in late pneumonia, so its higher frequency would also be explained. 25% of patients re-entered MV, this was associated with reintubations, which is indicated as another risk factor for VAP3,8,15,17.
It is also important to point out the other invasive devices that patients who developed VAP had, in the case of the central venous catheter (CVC) it had an average duration of 13 days, being similar in early and late VAP; and the days of urinary catheter is 9 days in early VAP compared to 14 days late.
A long stay in PICU is also another risk factor reported because it could condition to have greater colonization with in-hospital organisms; In the present study, the average days of hospitalization of patients with VAP was more than 30 days in all VAPs, and in the late 38 days, the upper range was 207 days. This stay could explain the higher frequency of late VAP: some of the reports show a higher risk with average stays 20 to 34 days. The average days of hospitalized patients in our PICU is 8, so the VAP considerably increases hospital stay14.
Other extrinsic factors mentioned are the surgeries performed. In our study, 30% of the VAPs were post-op and more frequently the neurosurgical ones, mentioning that the service evaluated is a general PICU and more than 50% of the patients it receives are post-op. In a study conducted by Garibaldi et al., It was found that 17% of postop patients had pneumonia9,17.
48% of the cultures were positive, with positivity being more frequent in late VAP. The most frequent organisms isolated were Stenotrophomona maltophilia and Pseudomonas aeuriginosa, that being the case that these were mainly isolated in late VAP. The isolation of the latter coincides with the majority of studies in which the most frequently isolated organisms are reported to gram negative, led by Pseudomona aeuriginosa, acinetobacter baumani, and klebsiella pneumoniae17. Our PICU reports quarterly on the organisms isolated in our flora.
CONCLUSION
The average annual VAP rate in the service evaluated was 9.8 per 1000 days of MV, according to international standards, the most frequent rate being the late one (65%). The most frequent VAP was among children under 6 months and male sex.
Malnutrition, congenital heart disease, mechanical ventilation time, days of hospitalization and surgeries were found in greater proportion in patients with VAP.
The most frequently isolated germs were Stenotrophomona maltophilia and Pseudomonas aeuriginosa, with a low proportion of multidrug resistance. Finally, VAP mortality was 15%.
Correspondence: Liliana Paola Cieza Yamunaqué
Address: Jr. Belisario Flores 238 Dpto 301 – Lince. Lima 14. Lima – Perú
Telephone: +51-990452547
E-mail: liciya04@hotmail.com.
Financing: Self-financed.
Conflict of interest: The authors declare no conflict of interest in the publication of this article.
