ARTÍCULO ORIGINAL
DOI 10.25176/RFMH.v19i3.2159
1 Faculty of Human Medicine - UPSMP, Lima-Peru.
2 Faculty of Public Health and Administration - UPCH, Lima-Peru.
a Medical specialist in administration.
b Medical specialist in administration, specialty of public health with mention in epidemiology.
ABSTRACT
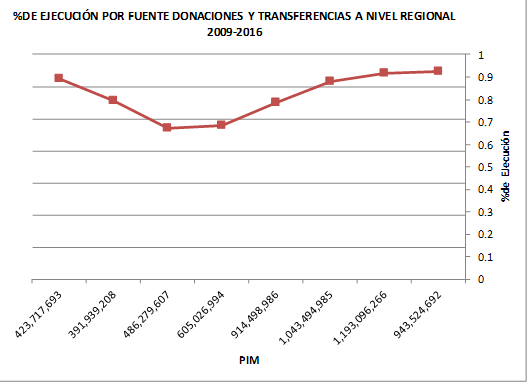
Objective: To Assess the impact of the capitated payment mechanism, implemented by the Comprehensive Health Insurance (SIS), in the execution of resources from the source of financing, donations and transfers, during the years 2012 to 2016, Peru. Methods: Assessment of the execution percentages of the regions, the number of preventive benefits versus the number of recuperative benefits and the impact on the increase of preventive care in the pilot regions versus the counterfactual regions was measured. A retrospective descriptive study was carried out pre post and difference of differences between the pilot regions Apurímac, Amazonas, Ayacucho, Callao and Huancavelica compared with a counterfactual paired by the Human Development Index; In addition, the regions of Moquegua, Loreto, Puno, Cajamarca and Huánuco were considered. Results: An increase in the average percentage of execution was observed, prior to the capitated mechanism, from 68.5% in 2012 to 92.3% in 2016; likewise, the increase at the national level of preventive benefits versus recuperative benefits, with the specific weight of preventive benefits being invested in favor of them and, using the difference in differences method, it was evident that the pilot regions had a positive difference of 1551 preventive benefits for every 10,000 insured persons versus the counterfactual regions.
Keywords: Impact; Payment Mechanism; Capitated; Pre Post; Sanitary Results; Intermediate results; Capitated; Payment mechanisms; Impact; Difference in differences; Health results; Intermediate results; Public insurance system. (source: MeSH NLM)
RESUMEN
Objetivo:Evaluar el impacto del mecanismo de pago capitado, implementado por el Seguro Integral de Salud (SIS), en la ejecución de los recursos provenientes de la fuente de financiamiento donaciones y transferencias, durante los años 2012 al 2016, Perú. Métodos: Se evaluó los porcentajes de ejecución de las regiones, el número de prestaciones preventivas versus el número de prestaciones recuperativas y se midió el impacto en el incremento de las atenciones preventivas en las regiones piloto versus las regiones del contrafactual. Se realizó un estudio descriptivo retrospectivo pre post y diferencia de diferencias entre las regiones piloto Apurímac, Amazonas, Ayacucho, Callao y Huancavelica comparados con un contrafactual apareado por Índice de Desarrollo Humano; además, se consideró a las regiones de Moquegua, Loreto, Puno, Cajamarca y Huánuco. Resultados: Se observó un incremento del porcentaje promedio de ejecución, previo al mecanismo capitado, de 68,5% en el 2012 al 92.3% el 2016; asimismo, el incremento a nivel nacional de las prestaciones preventivas versus las prestaciones recuperativas, llegando invertirse el peso específico de las prestaciones preventivas a favor de las mismas y mediante el método de diferencias en diferencias se evidenció que las regiones piloto tuvieron una diferencia positiva de 1551 prestaciones preventivas por cada 10 000 asegurados sobre las regiones del contrafactual.
Palabras clave: Impacto; Mecanismo de Pago; Capitado; Pre Post; Resultados Sanitarios; Resultados Intermedios; Impacto; Diferencia en diferencias; Sistema de Aseguramiento Público (fuente: DeCS BIREME).
INTRODUCTION
One of the main problems faced by the Health System in Peru is the efficient use of the resources allocated to the operation of health facilities at the different levels of government; whether they are managed by the Ministry of Health, EsSalud, other ministries or regional governments. However, as of 2015, the National Agreement of Peru recognizes universal access to health services and social security as a State policy3.
This state policy led during these years to an increase in the budget of the health sector and the access of more Peruvians to health services through the Comprehensive Health Insurance (SIS). This progressive increase, between the years 2013 - 2015, meant an important step in the strengthening of access to health, but at the same time, it represented a series of challenges that managers had to face, both from the scope of the public financier SIS and from the providers of health services, so it was necessary to reevaluate the forms of relationship developed from the year 2002 onward.
Since then in Peru, strategies have been implemented aimed at defining a model of public financing in health based on taxes, due to the slow growth of formality that would serve as a source of financing for a Bismarckian model in the field of Peruvian social security.
In 2009, Law 29344, Framework Law for Universal Health Insurance and its Regulations was enacted, establishing funding roles for public and private Health Fund Management Institutions (IAFAS, acronym in Spanish); as well as, the provider role for the Institutions that Provide Health Services (IPRESS, acronym in Spanish) of a public or private nature. The aforementioned law defines the SIS as an IAFAS, under the principle of irreversibility; that is, it is outside the scope of social programs. Within this framework, a series of actions was initiated aimed at establishing a contractual type of link or agreement between the SIS and the public IPRESS5.
The relationships between IAFAS and IPRESS are strongly related to the payment mechanism and the way in which it is remunerated to the IPRESS. Therefore, the way in which the resources collected, in a Health System, become services for people is a critical element in the equation between health and money. "This is the so-called purchasing function, which consists of making the resources collected from any of the sources mentioned be converted into services in the most efficient way possible."6
It is known that there are different types of payment mechanisms in the relationship between funders and health providers. In this regard, the present study will focus on analyzing the payment mechanism capitalized, consisting of financial transfers made by the SIS, to the health establishments in advance, taking as calculation an amount for each insured.
This mechanism "has proven to discourage the excess of services that if observed in the case of fee for service payment".7
The payment mechanism began as a pilot in the Huancavelica Region in 2011; the following year the regions of Amazonas, Ayacucho, Apurimac, and Callao were replicated. In the same fiscal year, the Resolution Jefatural 149-2012-SIS8 was issued, which establishes the procedure for calculating transfers from the SIS to public IPRESS, under the prospective capitated modality, and for 2013 the capital spread to the whole country. Subsequently, in 2016, some procedures of the capita are modified by means of Jefatural Resolution 009-2016 / SIS9, since the SIS only transferred budgets.
In the principal agent relationships, which mark the way in which public IPRESS interacts with the public IAFAS-SIS, the payment mechanism based on capitation was chosen in a closed budget framework, which only meant around 6% of the public budget assigned to the function about Health Area of the sector and regional governments.10. The capitated payment of the Comprehensive Health Insurance exercised a mechanism of distribution and containment of costs when betting on prevention and sharing the risk with the IPRESS, which were aimed at achieving, in the chain of causality, achievements at the level of intermediate results. Defined in three objectives:
1° Predictability of the value to be transferred to Public IPRESS, which allowed the provider to plan in a more real way the purchases of pharmaceutical products, medical devices, and medical devices.
2° Increase preventive care versus recuperative care, since the incentive to execute benefits, did not depend on the consumption of pharmaceutical products or medical devices; rather, it was incentivized to provide the preventive package for each stage of life.
3° Percentage increase in the execution of the resources transferred to the regions by Donations and Transfers through the SIS; as well as the budget allocated and executed in the first level of care versus the second and third levels of care
These objectives, unlike traditional capitated payments in the private health insurance market, were not designed solely to transfer risk but to modulate the behavior of IPRESS.
The SIS defines the payment mechanism capitated as a type of contract that creates specific incentives in relation to the medical benefit. These contracts are important tools for health managers, as there is evidence that they modify the behavior of another agent by altering the productivity, quality, and composition of the benefits, the distribution of the offer, the predictability in relation to the cost of the provider, among others.
The capitated payment is prospective and is made at the first level of attention. The power of the mentioned modeling lies in two financial components: the fixed, conditioned only to the signing of the agreement and that guarantees the benefits and; the variable, conditioned to compliance with performance indicators in the framework of Budget for Results. Additionally, it seeks to modify prestational behaviors, promoting preventive activity over the recuperative and strengthening the first level of attention. Finally, improvements in health outcomes and Public Health are expected.
Therefore, the SIS did not propose indicators aimed at improving the quality of service or final results such as the reduction of maternal mortality or anemia, since these objectives depended on other sources of funding, mainly from the Ordinary Resources transferred by the MEF to the Ministry of Health and regional governments; of the Directly Raised Resources, including the intervention of other sectors and other externalities that were not controlled through the Comprehensive Health Insurance. However, not only was it necessary to achieve objectives linked to transfers but also to encourage efficiency in the distribution of such transfers. In addition, to relate them to the fulfillment of the national sanitary objectives, inasmuch as the budget of the Integral Health Insurance experienced a very important increase during the years 2013 to 2015.
Among the difficulties encountered, we have:
1. Cumbersome procedures in the executing units, which did not necessarily facilitate the resources, assigned by the SIS prospectively, to reach directly the health facilities.
2. The lack of sufficient human resources that can reach the dispersed population
3. The lack of planned purchases for the achievement of the proposed goal. In this logic, other variables were included, such as the distribution of medicines and supplies to the health establishment and not only to the regional store.
4. Lack of management skills, which was why the incorporation of the management committees was necessary, which would authorize the expenses for the agreements taken from the health facilities of an executing unit.
5. The need to incorporate financial control figures through the mandatory filling of SIGA records, in addition to the SIASIS to be able to monitor spending.
Methodology of calculation of the capitated mechanism:
For the calculation of the capitated mechanism, from 2012 to 2015, two calculation methods were used:
i) By historical estimate and projection for the allocation of the budget for the recuperative benefits (attention and care) and the historical average use intensity, and
ii) By parametric estimation for preventive services based on the number of benefits that should be performed to comply with the provisions of current regulations of the Ministry of Health.
This last parameter was influenced by two indicators, extension of use and intensity of use, which was part of the negotiation with each region.
In this regard, in 2007, it should be mentioned that Chilean literature was found where a similar calculation model is analyzed, based on the calculation of programmable benefits and the benefits linked to morbidity or spontaneously named11
Another peculiarity of the methodology is that the calculation of the transfer, called capita, was developed by each region, it was not a national calculation. The reality of each region was considered and scenarios of increase of affiliation were modeled, among others12.
Once the projections of the health benefits were calculated, they were valued according to the SIS rate. This fee did not mean the total cost of the benefit; because, as we have defined previously, the allocation of resources through the SIS source (Donations and Transfers) covered only about 7% of the public budget for the health function.
P= Projected health benefits.
Q= Unit cost per SIS rate benefit.
Subsequently, the resulting value of (P * Q) was subject to adjustments by indicators; for example, the increase in membership during the following year, the extension of use in preventive benefits, the percentage of insured with complete packages in preventive benefits and other risk adjusters such as: rurality, poverty index and migration that were negotiated with the health service provider. Then, the result of the said equation was divided by the number of policyholders in the region, with which the per capita value was established. Finally, since 2016 the mechanism was substantially modified and eliminated by 2018.
Total cost / Number of insured = Cost per capita
Financial and performance indicators were adjusted, progressively, in the following years. The main characteristics of these indicators were related to reproductive health and pregnancy, to children and to priority noncommunicable and transmissible diseases.
Object of the study:
Carry out an evaluation of the payment mechanism called capita, developed in the Comprehensive Health Insurance between 2012 and 2016.
For this, two types of analysis will be developed:
A descriptive evaluation of the fulfillment of the objectives of the implementation of the payment mechanism called "capita of the Integral Health Insurance" at level I, for the percentage of execution by the funding source Donations and Transfers at the level of activities and the evolution of the number of preventive and recuperative benefits during the previous years and during the implementation of the mechanism evaluated.
Likewise, a quasi-experimental evaluation to compare the increase in preventive benefits during the pilot period of the payment mechanism capitated between the included regions versus those that were not included, taking as a base the benefits of 2011 and comparing them with those of 2012.
METHODS:
A secondary analysis of the budgetary execution of the regional governments of Apurímac, Amazonas, Ayacucho, Callao, Huancavelica, Moquegua, Loreto, Puno, Cajamarca and Huánuco will be carried out regarding the sources of financing. Donations and Transfers and Ordinary Resources, period 2009 - 2016, from the following sources of information_
1. Friendly consultation of the MEF.
2. Data entered into the SIS Assurance System (SIASIS) by health service providers nationwide.
3. Data of the number of insured to the SIS13
The method for the evaluation of the percentage of execution of the resources transferred by the SIS to the regions will be the following:
The information of the MEF Friendly Consultation will be analyzed for the period 2009 - 2016, comparing the levels of execution of the years prior to the implementation of the capita and the years of implementation at the level of the regional governments, for the resources transferred in the function health by the funding source Donations and Transfers, only activities, and will be compared with resources allocated by Ordinary Resources for the same years, under the same criteria.
For the comparison between capita and non-capita regions between 2011 and 2012, the information from the SIASIS of the Comprehensive Health Insurance will be used and to evaluate the impact we will use the methodology called Difference of Differences. In addition, the regions that will be part of the counterfactual will be paired by the Human Development Index with the Regions that are in the intervention group.
In order to standardize the results, the absolute number of benefits will not be used but the rate of benefits for ten thousand insured SIS.
The formula used for each comparison will be the following:
X=(Yt1-YT0)-(Yc1-YC0)
Where:
X = Impact in relation to the increase in the number of preventive benefits.
Yt1-YT0 : Number of benefits at the end and at the beginning in the regions of the intervention.
Yc1-YC0: Number of benefits at the end and at the beginning in the regions in which the intervention was not developed.
RESULTS
Percentage of execution:
Graphic 1 shows that, as of 2013, there has been a significant increase in the execution of transferred resources until reaching 92.36% in 2015.
.
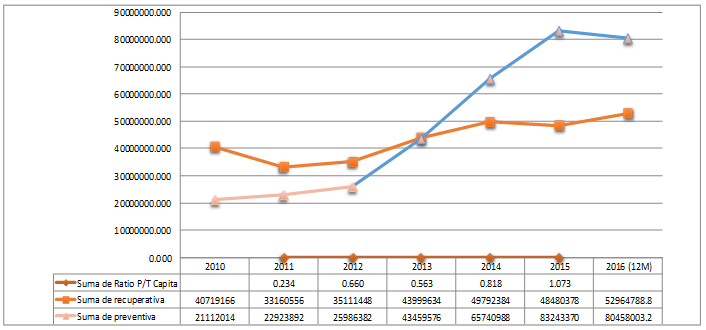
When assessing the growth of benefits from 2010 to 2016, it is observed that from the year 2013 there is an intersection between the lines of recuperative care and preventive care. This demonstrates, for the first time, the investment in relation to preventive benefits versus the recuperative financed by the SIS. In addition, this increase was four times more than the number of preventive benefits admitted to the SIASIS in 2012.
Comparison group of regions of intervention vs contrafactual:
The counterfactual regions were paired by the Human Development Index calculated for 2012, with the regions that were under the intervention.
| Ubigeo 2010 | Region | Population | Index of Human Development | Life expectancy at birth | Population with completed secondary school | Years of education (population aged 25 and older) | Family Income per capita |
|---|---|---|---|---|---|---|---|
| 070100 | Callao | 969,170 | 0.5863 | 79.16 | 81.01 | 10.35 | 822.6 |
| 010000 | Amazonas | 417,508 | 0.3846 | 73.99 | 53.65 | 6.66 | 435.7 |
| 030000 | Apurimac | 451,881 | 0.3444 | 72.41 | 60.57 | 6.15 | 330.8 |
| 050000 | Ayacucho | 666,029 | 0.3336 | 70.22 | 43.59 | 6.38 | 317.2 |
| 090000 | Huancavelica | 483,580 | 0.2962 | 65.16 | 43.16 | 5.58 | 317.2 |
| Ubigeo 2010 | Region | Population | Index of Human Development | Life expectancy at birth | Population with completed secondary school | Years of education (population aged 25 and older) | Family Income per capita |
|---|---|---|---|---|---|---|---|
| 180000 | Moquegua | 174,859 | 0.6215 | 77.76 | 80.74 | 9.64 | 1042.5 |
| 160000 | Loreto | 1,006,953 | 0.3977 | 70.49 | 43.61 | 8.09 | 500.1 |
| 210000 | Puno | 1,377,122 | 0.3942 | 67.52 | 74.04 | 7.49 | 426.3 |
| 060000 | Cajamarca | 1,513,892 | 0.3773 | 73.83 | 54.78 | 6.4 | 421.3 |
| 100000 | Huanuco | 840,984 | 0.3746 | 72.33 | 45.47 | 6.73 | 448.4 |
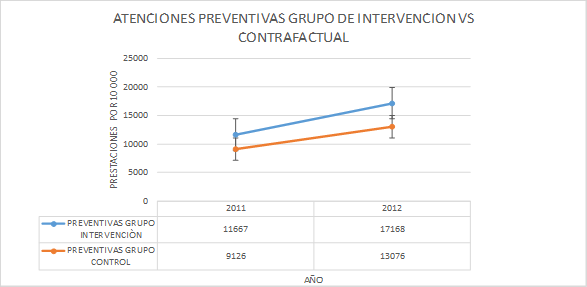
The result of the comparison between the intervention group and the counterfactual group shows a positive difference of 1551 more preventive attentions for every 10000 insured of the Comprehensive Health Insurance in favor of the group of regions of the intervention during the first year in comparison with the preventive attentions of the counterfactual group.
DISCUSSION
The results show that the capitation mechanism developed by the Comprehensive Health Insurance generated a significant increase in the total budget execution at the source of Donations and Transfers by the regions at the national level, as well as a significant increase in preventive activities versus recuperative, these results are consistent with what was expressed in a recent publication14 in Ecuador, which has also taken into account the positive factor that has a mechanism of payment by capitation in the increase of preventive benefits.
Also, although not to the same extent, they agree in part with an article published in July 201815, in which a methodology similar to that used in this study was used; Results were analyzed at the level of acute diarrheal disease, respiratory infection in children, anemia, maternal death avoided in pregnant women, coverage of growth and development and control of the healthy child, in this study only a significant impact on the indicators of acute diarrheal disease was observed. The lack of impact on the results at the other variables level would be related to the fact that the achievement of these results depends not only on financing through the Comprehensive Health Insurance but mainly on the budget transferred directly to the regions by Ordinary Resources from the MEF.
The Comprehensive Health Insurance for the implementation of the mechanism capitated in the Comprehensive Health Insurance, did not foresee the development of a prospective evaluation under the experimental methodology of an intervention group and a control group, so the decision to scale the mechanism of payment to 2013 for the whole country, was mainly due to the observation of the increase in preventive benefits in the regions of the capita area during the year 2012, assuming that this increase was due to intervention.
This premise on the part of the Comprehensive Health Insurance, was not necessarily true, as it was assumed under a pre-post evaluation; that the situation in these regions was to continue exactly the same for 2012 with respect to 2011.
Simple designs pretest-posttest. They are perhaps the best known and are a viable alternative when measurements of the relevant variables can be obtained prior to the intervention. However, from the point of view of internal validity, it provides few guarantees. The difference between the pre and post measures may be due to factors outside the intervention itself and this type of design does not allow to determine the net effect of the program16.
Therefore, although there were data that reasonably led to the conclusion that the intervention was generating the increase in the production of preventive care in the regions, the internal validity of this conclusion was not guaranteed, as well as the escalation at the country level in the year 2013 did not allow for a group of regions that are outside the mechanism capitated for more time.
In this context, we opt for the choice of this methodology to explain the increase in preventive benefits that occurred from 2013 to 2016 from the capitated mechanism.
In this regard, there is a Difference of Differences evaluation methodology that has clear advantages for the evaluation. It controls for all the characteristics that do not change over time (both observable and unobservable) and for all the changes in the time that affect the treated group and not treated in the same way17.
For greater validity, a group of counterfactual regions matched by an HDI Indicator was still chosen.
Therefore, the results obtained have significant internal validity and could be used to explain the reason why they were achieved from a causal relationship.
The positive effect of the mechanism capitated in the Comprehensive Health Insurance had also been observed in previous years. The first achievement clearly observed after the implementation, was the investment in the frequency of preventive benefits in front of the recuperative as well as the maintenance of the address of the preventive/recuperative ratio. These results represent a change in behavior in the provider that directs greater efforts in relation to the prevention and ceases to consider the provision as the center, to seek the health result that is achieved with good management of financing18.
Due to the specific weight of the financing of the Comprehensive Health Insurance, it is not pertinent to try to explain behaviors at the level of final health indicators, since these goals are financed mostly from Ordinary Resources by the Ministry of Economy and Finance.
Conclusiones:
The execution of the budget to the regions, by the funding source Donations and Transfers from the Comprehensive Health Insurance, increased from 68.5% in 2012 to 92.3% in 2016.
In relation to preventive benefits, based on the results of 2013, there is an increase in preventive benefits. The same thing also happens with the inversion of the preventive/recuperative relationship, keeping the trend in the following years evaluated.
The regions selected as pilot capita, during the year 2012, achieved a difference of 1,551 preventive benefits, for every ten thousand insured, versus regions that were not included in the said pilot.
From the observed, it can be indicated that the payment mechanism capitated by the SIS confirms three expected results: i) Increase in the percentage of execution in the regions of the resources transferred by the Donations and Transfers Source, ii) Generated the investment of the preventive /recuperative relationship in favor of preventive benefits; and iii) Results of an increase in preventive benefits were higher in the pilot versus the counterfactual regions.
This information is made available to be taken into account by the different public IAFAS and especially by the Comprehensive Health Insurance for making decisions regarding the decision to resume the capitalized mechanism developed during the years 2012 to 2016.
Authorship Contributions: The authors participated in the genesis of the idea, project design, data collection and interpretation, analysis of results and preparation of the manuscript of this research paper.
Financing: Self-financed.
nterest conflict: The authors declare no conflict of interest in the publication of this article
Received: March 20, 2019
Approved: May 20, 2019
Correspondence: Pedro Grillo-Rojas. Evaluación del mecanismo de pago capitado en el seguro integral de salud del Perú.
Address: Alameda del Corregidor 1502, La Molina 15024
Phone: 995039075
E-mail: drgrillorojas@yahoo.com
