REVIEW ARTICLE
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2019 - Universidad Ricardo PalmaDOI 10.25176/RFMH.v20i1.2558
ASSOCIATION BETWEEN PRE-HOSPITAL CARE TIME AND HOSPITAL MORTALITY IN VICTIMS OF TRAFFIC ACCIDENTS
ASOCIACIÓN ENTRE TIEMPO DE ATENCIÓN PRE HOSPITALARIA Y LA MORTALIDAD HOSPITALARIA EN VÍCTIMAS DE ACCIDENTES DE TRÁNSITO
María Jesús G. Fernandez-Sandoval1, Bryam J. Vasquez-Zavala1.
1 Research Institute in Biomedical Sciences, INICIB, Ricardo Palma University. Lima, Peru.S
ABSTRACT:
Introduction: Traffic accidents (AT) are the first priority in health research in Peru, According to the World Health Organization (WHO) it is estimated that the economic costs of vehicle impact and injuries due to AT are 1 % and 1.5% of the Gross National Product (GNP) in low and middle income countries; In Peru it is approximately 1.5 - 2% of the Gross Domestic Product (GDP).
Objective: To determine if there is an association between the time of prehospital care and hospital mortality in victims of traffic accidents.
Methods: A systematic review was carried out through the literature search of related articles in indexing sources such as PubMed and BIREME.
Results: Delays in the transfer of patients to the hospital and the lack of pre-hospital Emergency Medical System (SME) were significantly associated with an increase in mortality (P: 0.000) and the need for an SME as a prehospital care provider was significant predictor of emergency mortality with an adjusted odds ratio [OR] 2.19; 95% CI [1.88–2.55], and in the first 24 hours of admission with an adjusted OR 2.31; 95% CI [1.95–2.73].
Conclusions: The time of pre-hospital care in traffic accidents is significantly associated with hospital mortality, therefore, it is proposed to study factors associated with the longtime of pre-hospital care.
Keywords: Accidents, Traffic; Disaster Victims; Time; Emergency Medical Services; Emergency Care, Prehospital; Prehospital Emergency Care; Mortality. (Sources: DeCS Pubmed; BIREME)
RESUMEN
Introducción: Los accidentes de tránsito (AT) se encuentran como la primera prioridad en investigación de salud en el Perú, Según la Organización Mundial de la Salud (OMS) se estima que los costos económicos por impacto de vehículos y lesiones por AT son de 1% y 1.5% del Producto Nacional Bruto (PNB) en países de bajos y medianos ingresos; En el Perú es aproximadamente el 1.5 – 2% del Producto Bruto Interno (PBI).
Objetivo: Determinar si existe asociación entre el tiempo de atención prehospitalaria y la mortalidad hospitalaria en víctimas de accidentes de tránsito.
Métodos: Se realizó una revisión sistemática mediante la búsqueda bibliográfica de artículos relacionados en fuentes de indexación tales como PubMed y BIREME.
Resultados: Los retrasos en las transferencias de pacientes al hospital y la falta Sistema Médico de Emergencia (SME) pre hospitalarios se asociaron significativamente con un aumento de la mortalidad (P: 0.000) así mismo la necesidad de un SME como proveedor de atención prehospitalaria fue predictor significativo de mortalidad en emergencia con un odds ratio [OR] ajustado 2.19; IC del 95% [1.88–2.55], y en las primeras 24 horas de ingreso con un OR ajustado 2.31; IC del 95% [ 1.95–2.73].
Conclusión: El tiempo de atención pre hospitalaria en accidentes de tránsito se encuentra significativamente asociada a la mortalidad hospitalaria, por ello, se propone estudiar factores asociados al largo tiempo de atención pre hospitalaria.
Palabras Clave: Accidentes, tráfico; Tiempo; Servicios médicos de emergencia; Atención de emergencia, prehospitalaria; Atención prehospitalaria de emergencia; Mortalidad. (Fuentes: DeCS/BIREME)
Currently traffic accidents (TA) are the first priority in health research in Peru, due to the high mortality that this represents as well as the large number of affected who are left with irreversible injuries, this causes a high socioeconomic cost both for rehabilitation and the care of the injuries themselves. It is estimated that every year in the world 1.2 million people fail due to accidents on public roads and 50 million are injured and that if prevention and impact reduction systems are not improved and strengthened, it would increase by 65% in 20 years (1).
The economic costs of vehicle impact and AT injuries are 1% and 1.5% of Gross National Product (GNP) in low and middle income countries respectively and the annual global cost is close to US$ 518 000 million (1), in Peru, according to the National Road Safety Council (NRSC), every year there are approximately 70,000 traffic accidents with more than 3,000 deaths and more than 45,000 injuries, of which hundreds develop some kind of permanent disability(2).
In addition, the costs of traffic accidents in Peru could amount to one billion dollars per year, approximately 1.5 to 2% of GDP, according to the general office of statistics and informatics and the national rehabilitation institute, members of the National Sanitary Strategy for Traffic Accidents (ESNAT) of the Ministry of Health(3).
The response to traffic accidents is through emergency medical services, in Peru the main responsible for this are the SAMU and firefighters, among other emergency response bodies, from their prompt and timely response depends on the survival of the affected population. The prehospital care time is divided into four parts, the first in relation to the call from the place of the accident and the departure of the assistance service, the second between the departure of the assistance service and the arrival at the accident, the third the time of assistance in the same place of the accident and the fourth from the point of the accident to the arrival at the hospital for the appropriate management of the patient(4).
It is suggested that rapid pre-hospital care is associated with a decrease in mortality due to timely and effective hospital care. The objective of the study is to know the association between prehospital care time and hospital mortality in traffic accident victims.
METHODS
The question was asked: what is the association between prehospital care time and hospital mortality in vehicle accident victims? And the PEO question is: P: victims of traffic accidents; E: long time of prehospital care; O: mortality. For this, a systematic review was performed by searching related articles in indexing sources such as PubMed and BIREME.
The terms used for the PubMed search were: Accidents, Traffic; Traffic Accidents; Accident, Traffic; Traffic Accident; Time; Long-term Effect; Emergency Medical Services; Prehospital Emergency Care; Emergency Care, Prehospital; Mortality; Case Fatality Rates; Excess Mortality; Mortality Decline; Mortality Determinants; Differential Mortality; Death Rate; Mortality Rate. The following syntax was used: (((((("Accidents, Traffic”[mh]) OR Traffic Accidents*[tiab]) OR Accident, Traffic*[tiab]) OR Traffic Accident*[tiab])) AND ((((("Time”[mh]) OR Longterm Effect*[tiab]) AND "Emergency Medical Services”[mh]) OR Prehospital Emergency Care*[tiab]) OR Emergency Care, Prehospital*[tiab])) AND (((((((("Mortality”[mh]) OR Case Fatality Rates*[tiab]) OR Excess Mortality*[tiab]) OR Mortality Decline*[tiab]) OR Mortality Determinants*[tiab]) OR Differential Mortality*[tiab]) OR Death Rate*[tiab]) OR Mortality Rate*[tiab]), other terms were also used, such as “Prehospital time association”. For the search on BIREME the following terms were used: Emergency Care, Prehospital; Traffic Accident and mortality, being the syntax: (tw:(Emergency Care, Prehospital)) AND (tw:(Traffic Accident)) AND (tw:(mortality)).
A database was created from the program EXCEL.2013, where the results of the review were tabulated in tables.
Studies with less than 10 years reporting hospital stay and hospital mortality were included; excluding studies that repeated the systematic search.
RESULTS
Two search engines were used, both with different number of studies found in relation to the systematic search, in PubMed, with the syntax mentioned above and exclusion criteria 35 studies were found, of which only 4 were useful for our review, as well as other terms such as "prehospital time association" where we found 6 studies containing relevant data for our review. In the search engine BIREME, with the syntax and exclusion criteria presented above, 134 articles were found, 3 of which contained the information required for this study. The exclusion of other studies in this systematic search was due to the presence of other pathologies, not associated with car accidents or motor vehicle collisions, whose mortalities were associated with prehospital care time. Of these 13 studies, 2 are prospective and 11 are retrospective.
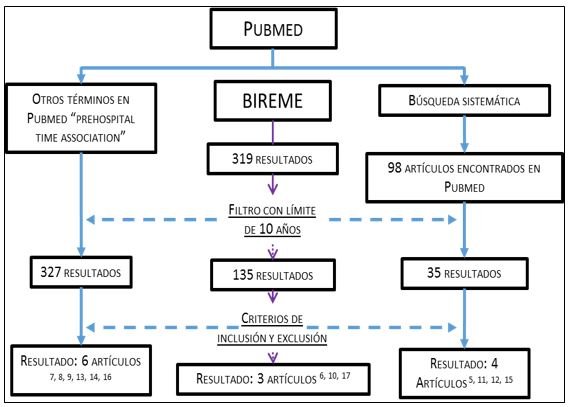
Illustration 1.Article selection flow diagram
| AUTHORS | POPULATION | COUNTRY | TYPE OF STUDY |
| TOHME et al.(5) | 589 | Switzerland | Prospective cohort study |
| Chandrasekharan et al.(6) | 773 | India | Observational prospective |
| MILLS et al.(7) | 18 709 | Denmark | Retrospective cohort |
| BROWN et al.(8) | 1625 | Australia | Retrospective cohort |
| BYRNE et al.(9) | 119740 | EE.UU | Retrospective cohort |
| GONZALEZ et al.(10) | 45,763 | EE.UU | Retrospective study |
| LOVELY et al.(11) | 3980 | EE.UU | Retrospective study |
| RIYAPAN et al.(12) | 39.761 | Thailand | Retrospective cohort |
| GAUSS et al.(13) | 6441 | France | Retrospective cohort |
| VERA-LOPEZ et al.(14) | 2,575 | Mexico | Case and control study |
| TANSLEY et al.(15) | 1568 | Canada | Analytical observational study |
| CHAMPION et al.(16) | 55537 | EE.UU | Analytical observational study |
| BONIFACE et al.(17) | 9316 | Tanzania | Cross-sectional study |
| YEAR | TITLE | AUTHORS | FINDINGS | RESULTS | IMPORTANCE | STRENGHTS | WEAKNESSES |
| 2019 | Prehospital time and mortality in patients requiring a highest priority emergency medical response: a Danish registry-based cohort study. | MILLS et al. (7) | Mortality from 1 to 30 days was not associated with prehospital time in traffic accidents. | OR 0,65 (IC 95% 0,29 a 1,48) | Studies the influence of the total prehospital time, in the mortality of 1 day as in that of 30 days | He managed to find that prehospital time does not affect mortality by up to 80 minutes. | The significant findings are merely associations and not causal. |
| 2019 | Association of Prehospital Time to In-Hospital Trauma Mortality in a Physician-Staffed Emergency Medicine System | GAUSS et al.(13) | The odds of death increased by 9% for each 10 minutes increase in prehospital time. | (OR, 1.09 [95% CI, 1.07-1.11]) and after adjustment by 4% (odds ratio, 1.04 [95% CI, 1.01-1.07]). | The association between prehospital care time (TAPH) and mortality. | Total prehospital time was the primary exposure variable | Existing comparative data are limited and conflicting. |
| 2019 | Longer Prehospital Time was not Associated with Mortality in Major Trauma: A Retrospective Cohort Study. | BROWN et al.(8) | No association was found between TAPH and 30 day mortality. But in 30 day survivors, the one-minute increase in time at the scene was associated with 1.16 times longer duration of hospitalization. | (Adjusted OR 1.10, 95% confidence interval (CI) 0.71-1.69) and odds ratio 1.16 (95% CI 1.03-1.31) respectively. | TAPH was associated with a longer hospital stay. | Reduced the risk of confusion | The study is subject to potential survivor bias. |
| 2019 | Injury Severity Score alone predicts mortality when compared to EMS scene time and transport time for motor vehicle trauma patients who arrive alive to hospital | LOVELY et al.(11) | Prehospital transport time (TTPH) was not significantly associated with mortality. | (P=0,458) | Mortality was significantly predicted. | Lots of scenes with prolonged TAPH. | Prehospital deaths could not be captured. |
| 2019 | Effect of predicted travel time to trauma care on mortality in major trauma patients in Nova Scotia. | TANSLEY et al.(15) | Lack of TTPH to care centers within 30 minutes was associated with a 66% higher risk of death | (OR 1.66, 95% confidence interval [CI] 1.09-2.52. P = 0.018) | The long TAPH was associated with worse outcomes for AT victims. | Reliability that prevented the inclusion of inaccurate data in the analysis. | Residual confusion due to unidentified factors is possible. |
| 2018 | The response of the Emergency Medical System and its relationship with different health outcomes in people injured by traffic in two Mexican cities. | VERA-LOPEZ et al.(14) | Association between opportunity for intervention (TAPH) with mortality and prehospital care associated with negative health consequences | OR 0,99;IC95%(0,97-1,01); p= 0,318 y OR 28,30; IC 95% (3,60-222,58); p=0,001 | Timeliness of care was associated with a shorter hospital stay. | Significant results and great association for the study. | The sample size for disability and mortality cases is small. |
| 2017 | Outcomes of Emergency Medical Service Usage in Severe Road Traffic Injury during Thai Holidays | RIYAPAN et al.(12) | Use of the emergency medical system as a prehospital care provider was a significant predictor of emergency and 24-hour mortality. | [Adjusted OR] 2.19; 95% CI [1.88-2.55], and in the first 24 hours of admission adjusted OR 2.31; 95% CI [1.95-2.73]. | The association between prehospital care system, and mortality. | Analyzed the country's largest registry in AT. | It did not collect data on confounding variables that could affect clinical outcomes. |
| 2016 | Factors Impacting Mortality in the Pre-Hospital Period After Road Traffic Accidents in Urban India. | Chandrasekharan A et al.(6) | Delays in patient transfers to the hospital and lack of prehospital emergency services were significantly associated with increased mortality. | (P = 0,000) | Late arrival at the hospital had a significant impact on mortality. | It contains the necessary data for association with morbidity and mortality. | Mortality is an outcome affected by several variables. In-hospital. |
| 2016 | The impact of short prehospital times on trauma center performance benchmarking: An ecologic study. | BYRNE et al.(9) | The odds of death with the shorter PHT were significantly higher than in the centers with the longer PHT. | (OR, 2.00; 95% confidence interval (CI), 1.43-2.78) | To assess the relationship of TAPH and adjusted mortality. | Excellent selection and calibration in risk adjustment models. | No conclusions can be drawn about the causal relationship. |
| 2016 | Time and place of death from automobile crashes: Research endpoint implications. |
CHAMPIONn et al.(16) | The risk of death after the accident is 0.4% per minute in the first 30 minutes, rising to 1% per minute in the next 60 minutes. | The resulting curve Y = 908.99e-0.013x establishes the relationship between time and mortality, RR = 0.967 | Assess whether there is an opportunity to reduce mortality from traffic accidents. | Establish the relationship between time after injury and death. | The study was limited to patients who were injured before 4 hours and after 5 minutes. |
| 2014 | Prehospital risk factors of mortality and impaired consciousness after severe traumatic brain injury: an epidemiological study | TOHME et al.(3) | Prehospital time was not identified as a risk or protective factor Mortality factors. | P= 0,264 | Hypothermia and hypotension were associated with short-term mortality. | The results had few losses in the follow-up. | The results are associations and therefore may not be causal. |
| 2013 | INJURY EXPERIENCE IN TANZANIA- NEED FOR INTERVENTION. | BONIFACE et al.(17) | One of the factors associated with mortality was the time of attention from the accident to the arrival to the hospital of 2-10 hours. | P=0,000 | Factors associated with mortality in six hospitals in Tanzania. | We found that AT is the most frequent cause of injury in this country. | The importance of AT itself is not emphasized. |
| 2009 | Does increased emergency medical services prehospital time affect patient mortality in rural motor vehicle crashes? A statewide analysis | GONZALES et al.(10) | Higher mortality was associated with a longer response time in rural rather than urban areas. | P=0,0001 | Seeks association between rural prehospital times in relation to mortality. | It emphasizes the time variable. | It does not take into account other variables that the patient may have. |
Prospective studies:
In the study by Chandrasekharan A. et al.(6) the mortality with a prehospital care time of less than one hour, of the 69 patients transported was 7, whose value is less than in an interval of 1 to 6 hours, where of the 197 patients 44 died, the same occurs with the interval of 6 to 24 hours, on roads away from the health center, where of the 416 patients 96 died, the mortality was higher than the survivors in a prehospital care time greater than 24 hours where of the 91 victims, 31 survived and 60 died. It was then found that delay greater than 24 hours was significantly associated with higher mortality (P =.00). Unlike the prospective cohort study by Tohme et al.(5) it was found that in trauma mechanisms such as AT, falls and other mechanisms, time as a prehospital risk factor for mortality is negligible (P =0.264), however hypotension (P =0.009), Hypoxemia (P = <0.0001) and hypothermia (P = <0.0001) were prehospital risk factors significantly associated with mortality and altered consciousness after a severe traumatic brain injury.
Retrospective studies:
In the study by Mills et al.(7) of 18709 patients studied, only 1687 were victims of traffic accidents, it was found that the total prehospital time, in urban areas, of 0 to 30 minutes versus >60 minutes is not significantly associated with hospital mortality at 1 day or 30 days, as in the analysis by Lovely et al.(11) who found that time at the scene of the accident and transportation time was not significantly associated with mortality (P = 0.31 and P = 0.458), as well as in the study by Brown et al(8) where there was also no association between a prehospital time of ≥60 minutes and a longer hospital stay, however, here the 30-day survivors, one minute delay in time at the scene of the incident was associated with 1.16 times (95% CI 1.03-1.31) a longer hospital stay. All interactions were significant (p> 0.05).
In the study by Gonzalez et al.(10) and Gauss et al (13) an association was shown with the significant and progressive increase in mortality with the total prehospital time. It was also found that an increase in prehospital time greater than 30 minutes was associated with a large increase in the risk of death in the hospital as well as a delay greater than 180 minutes. Tansley et al(15) also found that a delay greater than 30 minutes TTPH was associated with a 66% increase in the risk of death after adjustment for the confounding variables of age, sex, injury severity scale identified a priori (odds ratio [OR] 1.66, 95% confidence interval [CI] : 1.09-2.52, p = 0.018). However, this association was lost when scene deaths were excluded from the analysis (OR 0.93; 95% CI: 0.58 to 1.46, p = 0.78). In addition, the probability of death in these patients was associated with male gender (OR 1.45, p = 0.034), increased age (OR 1.02, p <0.001) and increased severity of injury scale (OR 1.11, p <0.001).
In the case-control study of Vera-Lopez et al.(14)it was found that there was no significant association between prehospital care time and mortality (OR 0.99; 95% CI 0.97-1.01; However, a large significant association with mortality was found for those patients who required prehospital medical care (OR 28.30; 95% CI 3.60-222.58; P=.001), as in the case of the study by Boniface et al.(17) and that by Riyapan et al.(12) where the use of emergency medical services as a means of prehospital transport in AT was associated 2.19 times more with mortality in emergency and referral (Adjusted OR 2.19; 95% CI [1.88-2.55]), as well as significantly increased mortality in the first 24 hours after admission to the emergency room (Adjusted OR 2.31; 95% CI [1.95-2.73]). We also found that the rate of mortality in emergency departments and during referral in patients with severe AT injuries who required transportation through the emergency medical service was significantly higher than in those who were not (2.00% vs. 0.78%; P <0.001).
In the retrospective cohort by Byrne et al(9) ,the odds of death in trauma centers with shorter prehospital time were found to be significantly higher than in centers with longer total prehospital times (odds ratio [OR], 2.00; 95% confidence interval (CI), 1.43-2.78). In the end, it was determined that there was no relationship between prehospital time and overall mortality. Therefore, there is no evidence of the inclusion of prehospital time of emergency medical services in the comparative performance evaluation analysis.
In the study by Champion et al. (16) 55537 deaths were analyzed within the range of 5 minutes to 4 hours of the accident, finding that the greatest number of deaths after the accident were in the prehospital period more than in the hospital period, showing that the risk of death after the accident per minute during the first 30 minutes was 0.4%, which increased to 1% per minute in the 60 minutes following the accident, which was gradually stabilized, for this reason they emphasize the early SME response, the resuscitation system and the importance of early action by the trauma center.
DISCUSSION
This review looked the association between the time of prehospital care and mortality in AT victims, which has been the first priority in health due to the high mortality that AT represent. It was found that while prolonged prehospital care time until arrival at an emergency center is an important factor in mortality and if a significant association is shown as shown in the studies of Chandrasekharan et al.(6), Gauss et al.(5), Tansley et al. (15), Boniface et al. (17), Champion et al. (16) or Gonzalez et al. (10) , Several studies found a significant association, the presence of other factors such as type of transport, age, sex, type of injury, severity of injury, state of consciousness, as well as the use of safety devices such as helmets or seatbelts, alcohol consumption, vulnerable road users, characteristics of the environment, whether rural or urban, as well as the distance between the accident site and the emergency center and the use or not of an emergency system for prehospital transport, this shows in various studies a significant association with mortality (11) as well as a minor association in other studies(9,10),This variation may be due to the severity of the trauma presented by the patient, this being the most important factor and constantly significantly associated with higher mortality.
It is expected that the result of transportation by a more qualified emergency medical service will be more effective due to handling by personnel prepared to intervene in this kind of emergency with safe and appropriate handling, with the application of protective equipment to prevent further injury or sudden worsening of the current condition, as well as specialized life support for prehospital care such as hemorrhage control, respiratory tract and the speed of arrival from the SME call to the victim's arrival at a center of attention, although there are studies such as that of Vera-Lopez et al. (14) that associate the provision of prehospital services in traffic accident victims with higher mortality and yet find no association between a long prehospital response time and this, it is mostly because, as demonstrated in the study of Lovely et al.(11),There are other factors, such as those mentioned above, that are associated with higher mortality, such as the severity of the injury.
However, it is not the only reason associated with hospital mortality, with the level of the care center and its ability to respond to this kind of emergency and serious injuries being an important factor, as found in the study by Mills et al.(7) that there is an association with lower mortality in non-tertiary hospitals than in tertiary hospitals, being the capacity of the health center where it is carried, an important factor in the mortality of AT victims.
Although there are studies that do not find an association between prehospital care time and mortality in AT victims, it should be noted that prehospital care also depends on other factors, in a systematic review Harmsen et al. (4)found that rapid transportation seems beneficial for patients suffering from severe trauma with blood pressure involvement, more in patients with milder injuries and hemodynamically stable, there is no greater increase in mortality compared to prehospital care time.
One aspect to consider is the limited availability of studies that contribute to the association of these variables at the national level, being necessary to strengthen research in this area.
CONCLUSIONS
The time of prehospital care in AT is significantly associated with hospital mortality of patients due to the need for early stabilization of the patient's condition. However, this depends on several factors inherent to the accident, and the severity of the patient at the scene, the appropriate removal of the AT victim from the scene that may require more time than expected due to the limitations of the service that provides care or the difficulty of the procedure, for this reason some studies showed lower mortality in longer pre-hospital times. Given the results it is proposed to study factors associated with long prehospital care.
Thanks: To Dr. Jhony A. De La Cruz-Vargas for his patience and contribution as supervisor and reviewer of this article.
Authorship contributions: The authors participate in the genesis of the idea, project design, data collecti on and interpretation, analysis of results, preparation of the manuscript.
Financing: Self-financed.
Conflict of interest: Authors declare no conflict of interest.
Received: 09 December del 2019
Approved: 27 December del 2019
Correspondent author: María Jesús de Guadalupe Fernández Sandoval
Address: Av. Los Gorriones 365, La campiña-Chorrillos, Lima, Perú.
Telephone: (+51) 935859812
E-mail: majus_1996@hotmail.com
REFERENCIAS BIBLIOGRÁFICAS
