ORIGINAL ARTICLE
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2020 - Universidad Ricardo PalmaDOI 10.25176/RFMH.v20i4.3219
BODY MASS INDEX AN ANTHROPOMETRIC MEASURE ASSOCIATED TO INDEX TG/HDL, A NOVEL CARDIOMETABOLIC RISK FACTOR
ÍNDICE DE MASA CORPORAL UNA MEDIDA ANTROPOMÉTRICA ASOCIADA A ÍNDICE TG/HDL, UN NOVEL FACTOR DE RIESGO CARDIO-METABÓLICO
Pamela Vasquez1,a, Rafael Ricra2,a, Liliana Cruz3,b,c, Nathalie Vargas3,d
1Universidad Ricardo Palma, Facultad de Medicina, Lima-Perú
2Hospital EsSalud Talara II, Piura-Perú
3Instituto Nacional de Salud, Lima-Perú
4Universidad Privada San Martin de Porres, Lima-Perú
aSurgeon
bMaster's Degree in Epidemiology and Biostatistics
cMedical Technologist
dMedical Student
Objective: To determine the relationship between obesity and TG/HDL index in patients attended in the endocrinology outpatient service of the Sergio Bernales National Hospital in 2018. Methods: The study was observational, analytical, case-control type unpaired at a 4: 1 ratio, with a total of 288 study subjects, 230 controls, and 58 cases who met the selection criteria, involved the patients seen in the endocrinology outpatient service. The sample was simply random, the variables were included: gender, age, Body mass index, total cholesterol, total triglycerides, HDL-c, LDL-c, TG / HDL index. A logistic regression model was used to obtain an Odds Ratio for the strength of association. Results: The relative frequency of obesity was 65.52% and 29.13%, for cases and controls respectively, in turn, a statistical significance with Fisher's exact test, P-value 0.000. A relationship between obesity and the TG / HDL-c index (OR 4.62, p = 0.000, 95% CI 2.51-8.52) was found by bivariate logistic regression. Conclusion: A relationship was found between Obesity and the TG/HDL-c index, which could be extrapolated to the adult population attended in the endocrinology service of Metropolitan Lima, this is the first article published in this regard at the national level, prospective studies are recommended to determine causality.
Key words: Body Mass Index, HDL-Cholesterol, Cholesterol, LDL-Cholesterol, Cardiovascular diseases(Source: MeSH NLM).
Obesity is defined as the excessive accumulation of adipose tissue, which can compromise health(1), currently, the Body Mass Index is used, with values greater than or equal to 30 kg / m2 compatible with its diagnosis. Obesity, with a worldwide prevalence of 19.5%, has reached pandemic levels, being a known risk factor in multiple non-communicable diseases(2). In 2017, the Pan American Health Organization reported a prevalence of obesity of 26.8% in the continent of South America, this being higher than the world prevalence(3). At the national level, the national institute of statistics and informatics in its latest report on noncommunicable diseases found a national prevalence of 22.7%(4).
Dyslipidemia is defined as the alteration of the plasma levels of cholesterol and/or triglycerides(5,6), with three types, hypercholesterolemia, hypertriglyceridemia, and mixed hyperlipidemia(5), with hypercholesterolemia the most frequent(5,7,8). Few studies in Latin America have sought to explore the prevalence of dyslipidemia at the national level, Mexico reported a prevalence of 18.3% in its national health survey(9), on the other hand in the United States, between 2009 and 2012, more than 311 million cases of hypercholesterolemia(10). Among its complications, the atherogenesis responsible for the development of coronary artery disease leads to a high cardiovascular risk in these patients(11,12). At present, it has been identified that the main lipoprotein involved in the atherogenic mechanism is the small and concentrated low-density lipoprotein (LDL-c), which is not measurable with conventional serological tests, which is why in order to estimate it, the TG / HDL-c index, which has been shown to correlate significantly with its values, taking values higher than 4 as a cut-off point as cardiovascular risk(13,14,15).
At present, immuno-endocrine functions have been discovered in adipose tissue, especially that of visceral location, which presents a dysregulation in the production of adipokines leading to insulin-resistance mechanism and alteration in the lipid profile of the patient(16,17). In the studies reviewed found discrepancies results for the association between obesity and index TG / HDL-c(18-21). Due to the aforementioned pathophysiological and epidemiological connections regarding obesity and dyslipidemia, this article aims to determine the relationship between obesity and the TG / HDL index in patients treated at the endocrinology outpatient service of the Sergio Bernales National Hospital in 2018, expecting to find an association between these 2 variables.
METHODS
Design
An observational, analytical, retrospective, case-control type unpaired study design was carried out, at a ratio of 4: 1 with a total of 288 study subjects, 230 controls, and 58 cases who met the selection criteria. The present study was carried out at the Sergio Bernales National Hospital in 2019, where data was collected from patients treated in 2018. The target population was adult patients over 18 years of age with outpatient care from the endocrinology service, being patients with Obesity, ausingnd the controls being non-obese patients.
Procedures and variables
Within the selection criteria for cases and controls, patients older than 18 years with a complete medical history were taken as inclusion criteria; The exclusion criteria were gestation, oncological pathologies, rheumatic pathologies, thyroid diseases, type 1 and type 2 diabetes mellitus, psychiatric disorders, diagnosed heart disease, and diagnosed kidney disease.
The independent variables in the study were Total cholesterol, Triglycerides, HDL-c, LDL-c, Age, Gender. The dependent variable, TG / HDL-c index. A BMI> = 30 was taken as values for obesity, as values for hypercholesterolemia I took> 200mg / dl and high LDL-c> 130mg / dl. They were taken from the anamnesis and antecedents present in the secondary information source, the clinical history is taken to performed by endocrinologists from the outpatient service. All the data present in the clinical history were stored in personal data collection files, which were stored for later draining and study.
Population and Sample
To calculate the sample size, a confidence interval of 95% was taken, statistical power of 80%, a ratio of 4: 1 for cases and controls respectively, for a proportion of exposed controls of 40%, a proportion of controls exposed 60.53% and an Odds ratio of 2.30, the epidemiological package OpenEpi of free access was used for the sample calculation where a total of 288 patients was obtained, being 58 cases and 230 controls respectively using the Kelsey formula. A one-stage probabilistic sampling was carried out where the population was stratified in patients with a TG / HDL-c index greater than 4 and a TG / HDL-c index less than or equal to 4, a simple random sampling was carried out in each of these strata, without replacement of study subjects.
Ethical Issues
The confidentiality of the patients included in the study was respected, personal information was not disclosed or worked with names, there was approval for execution by the authorities of the Sergio National Hospital Bernales, as well as the approval by the Ricardo Palma institution, Faculty of Human Medicine.
Statistical analysis
The data collection sheets were emptied into an Excel spreadsheet, which was later transferred to the statistical package STATA version 15 for statistical analysis.
Descriptive statistics will be presented for cases and controls, reporting the mean and standard deviation for quantitative variables such as age, BMI, Total Cholesterol, triglycerides, HDL-c, LDL-c, TG / HDL index, LDL / HDL index. As well as the absolute and relative frequency of the qualitative variables, gender, and categorical BMI, Older Adult, Hypercholesterolemia, elevated LDL-c, the Shapiro-France statistical test of normality was used to calculate the normality of each quantitative variable.
For inferential statistics, Fisher's exact nonparametric statistical test was performed for qualitative variables and a contrast test of medians, Mann Whitney's U test, for quantitative variables with respect to cases and controls. A bivariate logistic regression model was performed to obtain the Odds ratio and 95% confidence intervals.
RESULTS
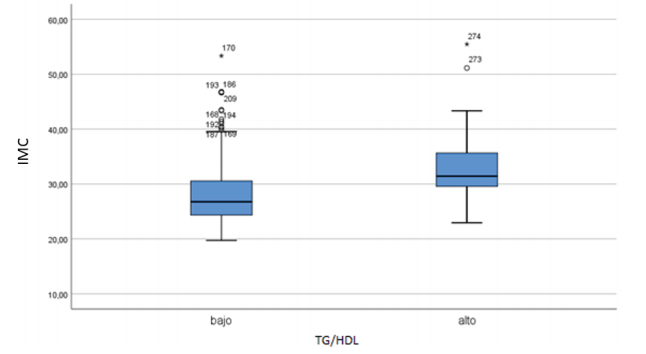
Of the total sample of 288 patients, 58 case-patients who presented a high TG/HDL index and 230 control patients who presented a low TG / HDL index. There was no missing information in the medical records. The mean and standard deviation of BMI were calculated for the cases and controls being 33.32 +/- 6.45 and 28.24 +/- 5.47 respectively, the BMI variable did not present a distribution using the Shapiro-France test, with a P-value of 0.000, so the Mann U- test was used Whitney for 2 independent samples finding a statistically significant association with a or P-value of 0.000, it was represented in a Box and Whisker graph (Graph 1). In turn, from qualitative statistical analysis, a relative and absolute frequency of obesity was found for the cases and controls of 65.52% and 29.13%, respectively, by means of Fisher's exact non-parametric test, a statistically significant association was found with a P-value of 0.000. The results of the other variables were reported in Tables 1 and 2.
Table 1. Quantitative univariate analysis
| Controls (N:)%(n) | Cases (N:)%(n) | P-value normality | test P-value statistical test | |
| BMI | 28.24 +/- 5.47 | 33.32 +/- 6.45 | 0.000 | 0.000 |
| AGE | 48.18 +/- 15.42 | 46.36 +/- 14.14 | 0.241 | 0.48 |
| Total Cholesterol | 171.65 +/- 27.18 | 199.21 +/- 30.41 | 0.000 | 0.000 |
| Triglycerides | 131.23 +/- 26.13 | 210 +/- 64.87 | 0.000 | 0.000 |
| LDL-c | 108.10 +/- 23.07 | 133.85 +/- 25.64 | 0.000 | 0.000 |
| HDL-c | 50.12 +/- 6.86 | 37.59 +/- 7.47 | 0.001 | 0.000 |
Table 2. Economic aspects in times of quarantine due to COVID-19 in the Peruvian population in 2020.
| Controls (N:)%(n) | Cases (N:)%(n) | p-value | |
| Obesity (BMI >=30) | 29.13% (67) | 65.52% (38) | 0.000 |
| Older adult (age >=60) | 24.78% (57) | 20.69% (12) | 0.321 |
| Gender | |||
| Male | 83.48% (192) | 77.59% (45) | 0.194 |
| Female | 16.52% (38) | 22.41% (13) | |
| Hypercholesterolemia | 10.87% (25) | 50% (29) | 0.000 |
| LDL-c alto | 10% (23) | 46.55% (27) | 0.000 |
A logistic regression model was used for the strength of association between the independent variables Obesity (OR 4.62, p = 0.000, 95% CI 2.51-8.52), gender (OR 0.69, p = 0.295, 95% CI 0.34-1.40) and Older Adult (OR = 0.79, p = 0.515, 95% CI 0.40-1.60) for the dependent variable TG / HDL Index (Table 3), where only the obesity variable presented statistical significance through an Odds Ratio greater than 1 whose intervals were also greater a 1.
Table 3. Economic aspects in times of quarantine due to COVID-19 in the Peruvian population in 2020.
| Variables | Odds Ratio | P-value | Confidence interval |
| Obesity | 4.62 | 0.000 | 2.51 – 8.52 |
| Gender | 0.69 | 0.295 | 0.34 – 1.40 |
| Elderly | 0.79 | 0.515 | 040. – 1.60 |
DISCUSSION
A relationship was found for the variables Obesity (BMI> = 30) and TG / HDL-c index in the adult population attended in the service of endocrinology of the Sergio Bernales National Hospital in 2018. This can be supported by the directly proportional relationship between adipose tissue (especially visceral tissue) and lipoproteins present in the blood, explained by the metabolic dysregulation generated by an increase in the number of adipokines generated that lead to insulin resistance(11-14).
Our study is in line with the results presented by Weiss et al who found a statistically significant association for a BMI equal to or greater than 30 with the TG/HDL-c Index, with a P-value of 0.001 in the Palestinian and Israeli population(18) as well such as Ozturk et al who reported a statistically significant association between elevated TG / HDL-c and Body Mass Index, with a P-value <0.01. Unlike the study presented by Marotta et al, who did not find a significant association between elevated TG / HDL-c values with BMI, more if they found an association with the waist-hip index with a P-value of <0.001(19). García et al reported a statistically significant association for elevated TG / HDL-c values and visceral fat volume, reporting a statistically significant association by a linear regression model(20).
As part of the limitations of the study, it is reported that it was single-center, in a single hospital in Metropolitan Lima. Its population was limited to patients treated in single outpatient service, endocrinology and of a middle to lower socioeconomic class, which It only allows us to extrapolate to patients with these characteristics, which reduces its external validity. For the genesis of the reported information, the information was not generated, a secondary source of information was used, the medical records, which could affect the internal validity of the study. There was no information regarding anthropometric measures of visceral obesity such as abdominal circumference, waist-height index, and waist-hip index, which is more associated with dyslipidemic states and immune dysregulation(23) the variables required to generate the variable were not available. compound metabolic syndrome, which affected the internal validity of the study. The present study can be generalized to the adult population of lower-middle socio-economic stratum attended in outpatient endocrinology consultation at the level of Metropolitan Lima.
Studies are recommended that can evaluate the sensitivity and specificity of the TG / HDL-c index with respect to metabolic syndrome and cardiovascular risk scores. In turn, prospective studies are recommended that can include the missing anthropometric measures in our study to estimate which of these is the one with the greatest relationship with the TG / HDLc index.
CONCLUSION
A relationship was found between Obesity and TG / HDL-index. c being able to extrapolate to the adult population treated in the endocrinology service of Metropolitan Lima, this is the first article published in this regard at the national level, prospective studies are recommended to determine causality.
Author’s Contributions: The authors participated in the genesis of the idea, project design, data collection and interpretation, analysis of results, and preparation of the manuscript of this research work.
Funding: Self-financed..
Conflicts of interest: The authors declare that they have no conflict of interest.
Received: May 15, 2020
Approved: June 15, 2020
Correspondence: Pamela Daria Vásquez Rosales
Address: Av. 1ero de Mayo 323 - Chancay, Lima-Perú.
Telephone: 981573165
Email: pamela_782@hotmail.com
REFERENCES