ARTICULO ORIGINAL
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2021 - Universidad Ricardo PalmaDOI 10.25176/RFMH.v21i1.3345
PERINATAL LOW FIVE-MINUTES APGAR PREDICTORS AT IN A PERUVIAN HOSPITAL
PREDICTORES PERINATALES DE APGAR PERSISTENTEMENTE BAJO A LOS 5 MINUTOS EN UN HOSPITAL PERUANO
Marco Antonio Chilipio Chiclla1,a, Karla Estefany Atencio Castillo1,b,John Paul Santillán Árias2,c
1Institute of Development Research for Professionals. Lima, Perú.
2Sanidad del Ejército del Perú. Loreto, Perú.
aBachelor of Obstetrics
bDegree in Obstetrics
cSurgeon
Background: Neonatal asphyxia is an important cause of mortality and neurological sequelaes. Objective: To determine the perinatal predictors of persistently low Apgar at 5 minutes in an EsSalud hospital. Material and methods: Observational, analytical case-control study. A census analysis of 889 neonates with low Apgar ( <7) at the first minute treated at the Octavio Mongrut Muñoz Hospital from 2009-2018 was carried out, after verification of the inclusion and exclusion criteria. The EsSalud Perinatal Surveillance System (SVP) was used. The Chi square test and crude odds ratio (ORc) were used as a measure of association. Likewise, binary logistic regression was applied to estimate adjusted odds ratios (ORa). Results: There were 17 780 live births during the study period, of which 889 (11.9%) had low Apgar scores at one minute. The incidence of persistently low Apgar score at five minutes was 5.68 per 1 000 live births. In the multivariate analysis, the only perinatal predictors of a persistently low Apgar score at 5 minutes were aspiration of meconium amniotic fluid (ORa=7 .82; p <0.01) and the presence of a congenital anomaly (ORa=3 .19; p <0.01). Conclusion: meconium amniotic fluid aspiration and the presence of a congenital anomaly are perinatal predictors of a persistently low Apgar score at the fifth minute of extrauterine life in an EsSalud hospital.
Key Words: Apgar score, Newborn, Premature birth (fuente: MeSH NLM).
In 1953, the American physician Virginia Apgar (1) research findings were published. They proposed evaluating the need for neonatal resuscitation through the systematic observation of five parameters: skin color, muscle tone, reflexes, respiration, and heart rate. (2). Although the initially proposed scoring system had some resistance to its application, in the mid-50's it was already applied in thousands of newborns, persistently and by 1960, it was already widely used in thousands of hospitals around the world because of its simplicity and utility (3). Although this score was designed to assess neonatal status at the minute of life, some began to use it at five minutes of life as an indicator of response to interventions applied, later becoming the standard of neonatal care (4).
Despite the limitations of the Apgar score, it currently continues to be a tool of proven utility and practicality, as it is indicative of the need to opt for a timely neonatal resuscitation (5), especially if it is a sustained neonatal depression evidenced by Persistent low Apgar scores at 5 minutes. Unlike Apgar at one minute, this indicator increases the probability of requiring mechanical ventilation by eighteen times, almost five times the risk of intraventricular hemorrhage, among other adverse neonatal outcomes (6). Furthermore, research shows that a persistently low Apgar increases the risk of neonatal mortality at least five times (7); Studies even indicate that the impact of low Apgar persistence transcends the childhood stage by generating vulnerability in development (8). Given the unfavorable repercussions of a persistently low Apgar at 5 minutes, it is essential to anticipate an event of this type by timely recognition of the factors that predict its occurrence.
In Peru, Acero et al. (9) reported low 1ꞌ Apgar scores in up to 4.1% of newborns, figures that according to Yaipén et al. (10) risp to 27% of neonates previously exposed to fetal distress. The Apgar per minute is often not the best predictor of morbidity and mortality, but rather an expression of the newborn’s immediate physiological condition; instead, persistent low Apgar at 5 minutes is a more sensitive marker for predicting adverse neonatal outcomes. The Hospital I-4 Octavio Mongrut Muñoz has not been exempt from reporting low Apgar scores in many neonates seen; in some cases, the score’s low persistence at five minutes anticipates the case’s seriousness. Based on these details, the purpose of this research was to determine the perinatal factors that predict a persistently low Apgar at 5 minutes in a Social Security establishment in Peru.
METHODS
Design and study area
Observational, retrospective, and analytical investigation of cases and controls; carried out from a database of newborns from Hospital I-4 Octavio Mongrut Muñoz.
Population and sample
The population was made up of all neonates with low Apgar ( < 7) per minute of extrauterine life attended at the Hospital I-4 Octavio Mongrut Muñoz, who were children of users attended at this establishment from 2009 to 2018.
No sample size calculation was performed, given that access was made to the database of the Perinatal Surveillance System (SVP) EsSalud of the establishment in question. A total of 889 newborns (population) with a low Apgar score at one minute were identified, out of a total of 17,780 live births (universe) for that period. Of the neonates with low Apgar population at one minute, 101 (11.3%) had persistently low Apgar at five minutes of extrauterine life.
Neonates with persistently low Apgar at 5 minutes were defined as cases; that is, newborns with an Apgar score less than 7 evaluated at the first and fifth minute after delivery. While the controls were those with an Apgar score initially low at the first minute, but recovered (> 7) at the fifth minute, as it has been operationally defined in previous investigations (11,12,13).
The inclusion of newborns include i) Apgar score less than 7 at the first minute of extrauterine life was considered, ii) gestational age > 28 weeks, iii) present Apgar assessment records at the first and fifth minute of life, and ii) from pregnancies with a single fetus.
Neonates were excluded: i) extremely premature (age at birth <28 weeks); ii) with congenital anomalies incompatible with life (anencephaly, laryngeal atresia, hydranencephaly, bilateral renal agenesis, among others described in the medical literature (14)); and iii) those in a stillbirth condition or that were referred to other establishments with greater resolution capacity, from which it was not possible to obtain information.
Variables and instruments
The dependent variable was the persistently low Apgar at 5ꞌ, defined as an initially low Apgar at one minute that remains below 7 until the fifth minute of extrauterine life, as has been operationally defined in previous research (11,12,13). Complementarily, recovered low Apgar is defined as obtaining an initially low score (less than 7 at 1ꞌ) but above 7 at five minutes (15).
As perinatal factors, male, nocturnal birth (7:00 p.m. - 7:00 a.m.), presence of congenital anomaly, neonatal weight (were evaluated <1499 g, 1500-2499 g, 2500-3999 g, and>4000 g), aspiration of meconium in the amniotic fluid, birth trauma, and intrauterine infection. Additionally, the main in-hospital outcomes were described, such as the number of neonatal resuscitation maneuvers (NRM), hospitalization time (in days), and neonatal condition at discharge (alive, deceased, or referred to another health facility).
Procedures
The data collection technique was documentary since secondary sources of information were used. In this case, the Sistema de Vigilancia Perinatal (SVP) of the Hospital Octavio Mongrut Muñoz of EsSalud. SVP is a computerized tool implemented in all Social Security establishments in Peru for epidemiological surveillance purposes, and is currently a provider of maternal-neonatal information.
Statistical
analysis Data processing and analysis were performed in the Statistical Package for Social Sciences (SPSS) version 25 in Spanish. The descriptive analysis of qualitative variables used absolute and relative frequencies. In the bivariate analysis, Pearson's Chi-square test of independence with a 95% confidence level was used to determine the association between variables. The crude Odds Ratio (ORc) was used for its quantification.
In the multivariate analysis, the binary logistic regression was used, from which adjusted Odds Ratio (ORa) was obtained for each of the evaluated factors, also adjusting these for the confounding variable age at birth (in weeks), since the premature infant could receive scores Low Apgar scores due to their biological immaturity and not because of their actual well-being condition at birth, as indicated by the American College of Pediatrics (16). Additionally, the goodness of fit of the resulting model was verified (according to the Hosmer-Lemeshow test), considering p <0.05 as significant. Also, multiple correspondence analysis (MCA) was used to show an exploratory and multivariate way the interrelation between perinatal results and persistently low Apgar score at five minutes.
Ethical aspects
The procedures described in this study were based on data collection from documentary sources, which avoided informed consent. However, it is necessary to clarify the full respect of identifiable information during data processing, in accordance with the principles of the Declaration of Helsinki. Likewise, this research corresponds to a secondary analysis of data collected from previous research (17), which at the time was approved by the Ethics Committee of the Universidad Nacional Mayor de San Marcos (UNMSM).
RESULTS
Eight hundred eighty-nine neonates with low minute Apgar were analyzed, out of 17,780 live births from 2009 to 2018. Of the neonates population with low minute Apgar, 11.4% (101/889) presented scores persistently low 5 minutes, while 88.6% (788/889) recovered the low Apgar score initially obtained at 5'. The incidence of persistently low Apgar score at five minutes was 5.68 per 1,000 live births for the ten consecutive year period in which the analysis was delineated.
The neonates studied were male and female in 61.0% and 39.0% of cases, respectively. Likewise, the gestational age at birth was predominantly at term in 81.7% of cases, followed by preterm (17.1%) and post-term (1.2%) births. Regarding the minute Apgar, 81.6% of neonates had scores between 4 to 6 points and 18.4%, between 1 to 3 (Table 1).
The congenital anomaly was present in 65.3% of neonates with persistently low Apgar at 5ꞌ and only in 24.5% of those with recovered low Apgar, which showed that the congenital anomaly is a risk factor for Apgar persistently low (ORc = 5.81; p <0.01). A higher percentage of birth weight was observed <1499 grams (32.7% vs 2.7%) and from 1500 to 2499 grams (11.9% vs 7.2%) in cases compared to controls, which showed that a neonatal weight <1499 grams (ORc=1 8.77; p <0.01) and 1500 to 1499 grams (ORc=2 .51; p <0.01) are risk factors for a persistently low Apgar score. aspiration of Meconium in the amniotic fluid was a more frequent attribute in neonates with persistently low Apgar compared to those with recovered Apgar (10.9% vs. 2.5%), turning out to be a risk factor for persistently low Apgar at 5ꞌ (ORc=4 .69; p <0.01). Likewise, intrauterine infection showed a higher prevalence in cases than in controls (10.9% vs 4.9%), being also a persistently low risk factor for Apgar at 5ꞌ (ORc=2 .34; p=0 .01 ) (table 2).
The perinatal characteristics that were not risk factors for persistently low Apgar at the fifth minute of extrauterine life were neonatal male (ORc = 1.02; p = 0.93), nocturnal birth (ORc = 1.46; p = 0.08), neonatal macrosomia (ORc = 0.46; p = 0.19), and the presence of trauma at birth (ORc = 0.91; p = 1.00) (Table 2).
In the multivariate analysis, and also considering the adjustment for gestational age (in weeks), it was found that only persistently perinatal predictors of Apgar under aspiration of meconium amniotic fluid (ORa = 7.82; p <0.01) and the presence of some congenital anomaly (ORa=3 .19; p <0.01). On the other hand, perinatal factors that did not predict a persistently low Apgar score at the fifth minute were neonatal male, nocturnal birth, neonatal weight, birth trauma, and the presence of intrauterine infection (Table 3).
It was found that only 21.4% of newborns required only 1 neonatal resuscitation maneuver (NRM), 55.0% from 2 to 3 NRM, and 23.6% from 4 to 5 NRM. Most neonates required hospital stays of 0 to 6 days (84.6%); only 8.8% and 6.6% were hospitalized for 7 to 13 and more than 14 days. In 92.1% of cases, the neonatal condition at discharge was alive, in 4.9%, it was deceased, and only 2.9% of neonates needed to be referred to other hospital establishments with greater resolution capacity (Table 4).
In the multiple correspondence analysis (MCA), inertia (or accumulated variance) of 82.7% was found for two dimensions, which indicates that it is possible to represent the interaction between neonatal outcomes and Apgar status at five minutes (persistently low or recovered). Given that the accumulated inertia is greater for dimension 1 (39.6%), it is recommended that the interpretation be made in the direction of the axis it represents (vertical axis 0). In this way, it is possible to distinguish two differentiated neonatal profiles. The first (red circle) shows neonates with persistently low Apgar and the second, neonates with recovered low Apgar (green circle). In the figure in question, the degree of closeness between points (objects) is understood as the magnitude of the association between the categories of variables; thus, the recovered low Apgar is closely associated (almost superimposed) with the live category of a neonatal condition at discharge. The recovered low Apgar category is immediately associated with short hospital stays (0-6 days) and requirements of at least 1 neonatal resuscitation maneuver (NRM). However, note how the persistently low Apgar category at 5ꞌ is immediately associated –because of its proximity– with the neonatal condition of death at discharge; then, the persistently low Apgar score is associated with the need for 4 to 5 NRM, referral to another health facility, and long hospital stays of (7-13 days and >14 days). Newborns with low Apgar recovered at the fifth minute presented very homogeneous neonatal results, mainly characterized by being alive at discharge, had short hospital stays, and required few NRMs. In contrast, the persistently low Apgar score at 5ꞌ was associated with worse outcomes, among which mortality stands out.
Table 1.Characteristics of newborns with low Apgar from the Hospital Octavio Mongrut Muñoz of EsSalud.
| Neonatal characteristics | n | % |
|---|---|---|
| Sex | ||
| Male | 542 | 61.0 |
| Female | 347 | 39.0 |
| Gestational age | ||
| Preterm | 152 | 17.1 |
| At term | 726 | 81.7 |
| Post term | 11 | 1.2 |
| Apgar at minute | ||
| 1 a 3 | 164 | 18.4 |
| 4 a 6 | 725 | 81.6 |
| Total | 889 | 100.0 |
Table 2. Risk factors for persistently low Apgar at 5 minutes in newborns from the Hospital Octavio Mongrut Muñoz of EsSalud.
| Perinatal factors | Low Apgar at 5ꞌ | Orc* | 95% CI | p-value** | |||
| Persistent
(cases) |
Recovered
(controls) |
||||||
| n | % | N | % | ||||
| Male | |||||||
|---|---|---|---|---|---|---|---|
| Yes | 62 | 61.4 | 480 | 60.9 | 1.02 | (0.67 - 1.56) | 0.93 |
| No | 39 | 38.6 | 308 | 39.1 | |||
| Nocturnal birth | |||||||
| Yes | 67 | 66.3 | 452 | 57.4 | 1.46 | (0.94- 2.26) | 0.08 |
| No | 34 | 33.7 | 336 | 42.6 | |||
| Congenital anomaly | |||||||
| Yes | 66 | 65.3 | 193 | 24.5 | 5.81 | (3.74 - 9.03) | <0.01 |
| No | 35 | 34.7 | 595 | 75.5 | |||
| Neonatal weight | |||||||
| < 1499 g | 33 | 32.7 | 21 | 2.7 | 18.77 | (10.1 - 34.7) | < 0.01 |
| 1500 - 2499 g | 12 | 11.9 | 57 | 7.2 | 2.51 | (1.27 - 4.97) | < 0.01 |
| 2500 - 3999 g | 53 | 52.5 | 633 | 80.3 | Ref. | ||
| > 4000 g | 3 | 2.9 | 77 | 9.8 | 0.46 | (0.14 - 1.52) | 0.19 |
| LAM aspiration | |||||||
| Si | 11 | 10.9 | 20 | 2.5 | 4.69 | (2.17 - 10-11) | <0.01*** |
| No | 90 | 89.1 | 768 | 97.5 | |||
| Trauma at birth | |||||||
| Si | 2 | 2.0 | 17 | 2.2 | 0.91 | (0.20 - 4.02) | 1.00*** |
| No | 99 | 98.0 | 771 | 97.8 | |||
| Intrauterine infection | |||||||
| Yes | 11 | 10.9 | 39 | 4.9 | 2.34 | (1.16 - 4.74) | 0.01 |
| No | 90 | 89.1 | 749 | 95.1 | |||
| Total | 101 | 100.0 | 788 | 100.0 | |||
Table 3. Perinatal predictors of persistently low Apgar at 5 minutes in newborns from the Hospital Octavio Mongrut Muñoz of EsSalud.
| Perinatal factors | ORa* | 95% CI | p-value |
|---|---|---|---|
| Male | 1.31 | (0.78 - 2.16) | 0.30 |
| Nocturnal birth | 0.76 | (0.45 - 1.29) | 0.31 |
| Congenital anomaly | 3.19 | (1.88 - 5.43) | < 0.01 |
| PN: < 1499 g | 1.26 | (0.28 - 5.56) | 0.75 |
| PN: 1500 - 2499 g | 0.76 | (0.30 - 1.93) | 0.57 |
| PN: > 4000 g | 0.48 | (0.13 - 1.70) | 0.26 |
| LAM aspiration | 7.82 | (3.37 - 18.11) | < 0.01 |
| Trauma at birth | 1.51 | (0.25 - 9.09) | 0.64 |
| Intrauterine infection | 1.10 | (0.44 - 2.72) | 0.82 |
Table 4. Neonatal outcomes in newborns from the Hospital Octavio Mongrut Muñozof EsSalud.
| Resultados neonatales | N | % |
| Neonatal resuscitation maneuvers | ||
|---|---|---|
| 1 MRN | 190 | 21.4 |
| 2 - 3 MRN | 489 | 55.0 |
| 4 - 5 MRN | 210 | 23.6 |
| Hospitalization time | ||
| 0 - 6 días | 752 | 84.6 |
| 7 - 13 días | 78 | 8.8 |
| > 14 días | 59 | 6.6 |
| Neonatal condition at discharge | ||
| Alive | 819 | 92.1 |
| Deceased | 44 | 4.9 |
| Referred to another EESS | 26 | 2.9 |
| Total | 889 | 100.0 |
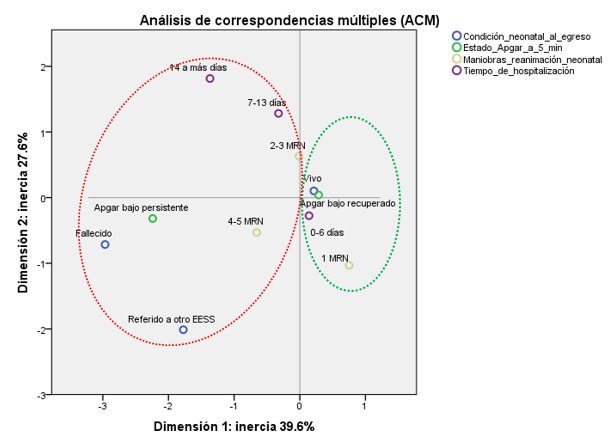
Figure 1. Multiple correlations of neonatal results and Apgar at five minutes in newborns from the Hospital I-4 Octavio Mongrut Muñoz of EsSalud.
DISCUSIÓN
According to the American College of Gynecology and Obstetrics (ACOG) and the American Academy of Pediatrics (AAP), the neonatal Minute Apgar should not be used or is not sufficiently capable of predicting future complications in the neonate (16). On the other hand, studies indicate that Apgar scores at 5 minutes do have a greater predictive utility for mortality (7), increasing their probability of occurrence up to 15 times (18); likewise, it is also predictive of neonatal morbidity (8,19), mainly neurological (20,21). Therefore, the anticipation of low Apgar scores by the fifth minute of extrauterine life is important, which can only be achieved by knowing its predictive factors. These will allow the health professional to adopt rigorously expectant attitudes towards those pregnancies where said predictive factors are identified.
The present study gives continuity to the findings reported in a previously published research (22), differing in the event of interest evaluated; While in this previous study, the “outcome” was only low Apgar at 1ꞌ, in the present investigation, the persistence of low Apgar was evaluated up to the fifth minute. As is naturally understandable, a more specific event requires a longer period to be properly observed; therefore, this research extends the analysis period to ten consecutive years (2009-2018). This procedure allowed us to find a persistently low Apgar score incidence at 5 minutes of 5.68 per 1,000 live births, a finding rarely reported in Peruvian research. Likewise, this figure is below the incidences reported in Asian countries such as Thailand, where the incidence of persistently low Apgar reaches 7.98 cases per 1 000 live births (12), which is to be expected since it is also -as Peru– from a developing country with little distant health indicators (23).
In the bivariate analysis, it was found that neonatal weight < 1499 grams (very low birth weight: VLBW) was the leading risk factor for persistently low Apgar at the fifth minute (ORc=1 8.7; p <0.01); while the weight between 1500 and 2499 (low birth weight: LBW) increased this risk to a lesser extent (ORc=2 .51; p <0.01), which is naturally understandable since the lower the birth weight, the greater It will be the degree of neonatal frailty; therefore, it is more likely to find newborns whose well-being is compromised, as has been reported in previous research (24,25). Likewise, other factors that increased the risk of persistently low Apgar were the presence of congenital anomalies (ORc = 5.81; p <0.01), aspiration of meconium amniotic fluid (ORc=4 .69; p <0.01), and antepartum intrauterine infection (ORc=2 .34; p <0.01), variables that have also been reported in previous studies as factors that can increase the risk of persistently low Apgar (26,9,27). However, bivariate evaluations are not sufficient, since a health phenomenon (persistent low Apgar, in this case) very rarely responds to a unicausal model, being necessary multivariate evaluations where the confluence of various potentially predictive factors (perinatal factors, in this case) are analyzed, as explained by Berea et al. (28) in a publication.
After the multivariate analysis, which consisted of the application of binary logistic regression, it was found that neonatal weight (VLBW and LBW) was not a predictor of a persistently low Apgar score at the fifth minute, which is most likely due to the inclusion of age gestational at birth (confounding variable) in the statistical model. The decision was made to include gestational age at birth in the model, since preterm infants may have received persistently low Apgar scores due to their biological immaturity and not because of their actual well-being condition at birth, as indicated in a publication of the College American College of Pediatrics (ACP) and American College of Obstetrics and Gynecology (ACOG) (16). Therefore, after multivariate adjustment, which includes gestational age at birth, neonatal weight is no longer a factor that increases the probability of obtaining persistently low Apgar scores at the fifth minute of extrauterine life.
Aspiration of meconium amniotic fluid (LAM) was the main perinatal predictor of a persistent low Apgar score at 5ꞌ (ORa = 7.82; p <0.01), which is consistent with that reported by Liran et al. (29) for whom the mere presence of meconium amniotic fluid adequately predicts Apgar scores <7 persistent up to 5ꞌ (ORa=8 .31; p <0.001). Likewise, for Sori et al. (30), a meconium amniotic fluid of thick consistency perfectly predicts low Apgar scores that last up to 5ꞌ (ORa = 14.9; p <0.05). Even for researchers in Europe, a meconium-stained amniotic fluid can predict extremely low Apgar scores (<3) and persistent at the fifth minute of extrauterine life (ORa=3 .7; p <0.001) (31). The expulsion of meconium is an indicator of maturity of the intestinal tract’s maturity and the parasympathetic system; However, in hypoxic situations, it is a fetal reflex in response to intrauterine distress, and aspiration may occur if said hypoxia occurs in a severe and sustained manner (32). This explains not only the close link found between LAM aspiration and low Apgar scores that last to the fifth minute, but also its predictive capacity.
The presentation of some congenital anomaly presentation was also a perinatal predictor of a persistently low Apgar score (aOR = 3.19; p <0.01) at 5ꞌ. Given that many published studies (27,24,33,25) choose to exclude newborns with congenital anomalies, it was impossible to find enough referents to contrast this result. However, among the few studies found, similarity was observed with an investigation carried out in Chile where it was reported that congenital malformations predict sustained low Apgar scores up to 5ꞌ (ORa = 4.76; p <0.001) (34). Although other publications do not do a multivariate analysis of the malformation as a predictor of persistently low Apgar, they partially support what was found in this study. Thus Acero et al. (9) reported that congenital malformation is a risk factor for low Apgar (ORc = 7.0; p <0.01); Likewise, a study carried out in Brazil indicates that the congenital anomaly is 4.6 times more frequent in neonates with persistently low Apgar scores at 5ꞌ (35). Contrarily, for Vasco et al. (26), the absence of congenital defects is a protective factor for obtaining sustained low Apgar scores at 5 minutes.
Between 16.1% and 5.9% of neonates fail to breathe spontaneously after birth in the first and fifth minutes of life (36), which is an indicator of sustained neonatal depression. Likewise, in some cases, there is an absence of crying (10.2%), limb movement (7.3%), and abnormal coloration (3.3%), indicators that translate into persistent low Apgar scores, resulting in the need for neonatal resuscitation maneuvers in up to 10% of newborns (37). This was corroborated in the present study and found longer hospital stays and mortality in neonates with a persistently low Apgar score at the fifth minute. Apart from the limitations of this study (for example, the non-inclusion of maternal factors), it has been shown that perinatal factors also contribute to explain a large part of the cases of persistently low Apgar score at 5 minutes, being necessary further research in this regard.
CONCLUSIÓN
Perinatal predictors of persistently low Apgar scores at five minutes are the aspiration of meconium amniotic fluid and the presence of congenital abnormalities.
Author’s contributions: MACC participated in the conception of the study, analysis, and interpretation of the results, writing of the first version of the manuscript
and statistical analysis. KEAC participated in the writing of the first version of the article, analysis and interpretation of results. JPSA participated in the collection
of results and interpretation of results. All authors participated in the critical review of the article and approval of the final version.
Funding: self-financed study.
Conflict of interest: the authors declare that they have no conflict of interest.
Received: October 17, 2020
Accepted: December 18, 2020
Correspondence: Marco Antonio
Chilipio Chiclla.
Address: Jr. 2 de septiembre
C05, Mala, Cañete.
Cell: 992627064
Email:
marco.chilipio@unmsm.edu.pe.
REFERENCES
