ARTICULO ORIGINAL
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2021 - Universidad Ricardo Palma10.25176/RFMH.v21i2.3452
APPLICATION OF PANORAMIC T2 SEQUENCE FOR MAGNETIC RESONANCE IMAGING OF LUMBOSACRAL SPINE
APLICACIÓN DE SECUENCIA T2 PANORÁMICA PARA RESONANCIA MAGNÉTICA DE COLUMNA LUMBOSACRA
Alexander Román Meza 1,2,3,a,b,c , Raúl Ruiz Arias 4,5,6,d,e
1 Servicio de Tomografía y Resonancia, Hospital Nacional Edgardo Rebagliati Martins, EsSalud.
Lima, Perú.
2 Centro de Diagnóstico por Imágenes de Clínica Internacional - Sede San Borja. Lima, Perú.
3 Miembro de la Asociación Peruana de Tecnólogos Médicos en Calidad y Seguridad Radiológica
(APTEMCSER). Lima, Perú.
4 Jefe de la Oficina de Estadística e Informática del Hospital de Emergencias José Casimiro Ulloa
- Ministerio de Salud. Lima, Perú.
5 Docente de Posgrado de la Facultad de Tecnología Médica de la Universidad Nacional Federico
Villarreal. Lima, Perú.
6 Docente de Estudios Generales de la Universidad San Ignacio de Loyola. Lima, Perú.
a Graduate in Radiologic Technology;
b Specialist in computed tomography (CT) and magnetic resonance imaging (MRI);
c Master of Health Services Management
d Graduate in Statistics;
e Master in Statistics
ABSTRACT
Introduction: The evaluation of the total spine by magnetic resonance imaging in a
T2-weighted single sequence using Software Composing previous planning, called panoramic, would be
beneficial in the study of lumbosacral spine for the additional information that could be obtained.
Objective: To analyze the application of T2 panoramic sequence for magnetic resonance imaging of
the lumbosacral segment. Methods: Retrospective and cross-sectional study executed with 186 cases
selected by stratified probability sampling, between 18 and 60 years old, using a form consisted of a
general sheet and an analytical sheet obtained from the request for radiological study and the
examination itself. Results: Of the total, 80.1% were in the adult stage of life, and 53.8% were
female, and 52.7% had the suspicion of herniated disc as a specific diagnostic presumption. Degenerative
pathologies were mainly presented, with 93%, having herniated discs as the most frequent with 57%, which
included extruded, protruded and migrated hernias with 40.6%, 37.9% and 21.5 % respectively. Likewise,
it was verified with hypothesis test that this acquisition allows to localize 50% more findings in
contrast to the usual examination, defining that this sequence should be applied because it localizes
findings in a greater number in comparison to the lumbosacral selective examination. Conclusions:
In
general, it was defined that the application of this panoramic T2 sequence is more usefulness for a
better evaluation, because it achieves greater findings, resulting as main pathologies in lumbosacral,
cervical and dorsal segments those of a degenerative type, standing out the herniated discs.
Keywords: Magnetic resonance imaging, Radiologic technology, Spine. (Source: MeSH NLM).
RESUMEN
Introducción: La evaluación de columna total mediante resonancia magnética en una sola secuencia
potenciada en T2 utilizando Software Composing previa planeación, denominada panorámica, sería
beneficioso en el estudio de columna lumbosacra por la información adicional que podría obtenerse.
Objetivo: Analizar la aplicación de secuencia panorámica en T2 para resonancia magnética del
segmento lumbosacro. Métodos: Estudio retrospectivo y transversal realizado con 186 casos
seleccionados mediante muestreo probabilístico estratificado, entre 18 a 60 años, utilizándose una ficha
conformada por una hoja general y una hoja analítica obtenidas de la solicitud de estudio radiológico y
el propio examen realizado. Resultados: Del total, un 80,1% era de etapa de vida adulta, y 53,8%
era femenino, además que un 52,7% tuvieron como presunción diagnóstica específica la sospecha de hernia
discal. Se presentó principalmente patologías degenerativas, en un 93%, teniendo a las hernias como las
más frecuentes en un 57%, que a su vez comprendió hernias extruidas, protruidas y migradas con 40,6%,
37,9% y 21,5% respectivamente. Así mismo, se comprobó con prueba de hipótesis que esta adquisición
permite localizar un 50% más de hallazgos a diferencia del examen habitual, definiéndose que esta
secuencia debe aplicarse porque localiza hallazgos en un mayor número en comparación al examen selectivo
lumbosacro. Conclusiones: De forma general, se definió que la aplicación de esta secuencia T2
panorámica
es de mayor utilidad para una mejor evaluación, por lograrse mayores hallazgos, resultando como
patologías principales tanto en segmento lumbosacro como cervical y dorsal las de tipo degenerativas,
resaltando las hernias discales.
Palabras clave: Imagen por resonancia magnética, Tecnología radiológica, Columna vertebral.
(Fuente: DeCS BIREME)
The Peruvian population has undergone a sociodemographic transition with a decrease in the mortality rate, a larger economically active population, and population aging, with a greater presentation of chronic-degenerative diseases to the detriment of infectious diseases (1). Among this group of now frequent diseases are dorsopathies, located in a sixth place of morbidity for outpatient consultation, with 3.2%, and which occurs in all stages of adult life: 2.4% in young adults, 5.6% in adults and 6.9% in older adults, and even in teenagers, with 1.3%, a situational context that had not occurred in recent decades (2).
In this way, an adequate evaluation of the spine is of utmost importance, especially at the level of the lumbosacral spine, since in this region there is greater symptomatology, being the objective of clinical and especially radiological review because it is the most useful diagnostic. Currently, magnetic resonance images stand out for allowing the visualization of anatomical information at the spinal and vertebral level with high contrast resolution, having as a fundamental part the T2-weighted image sequence that demonstrates the differentiation between cerebrospinal fluid with the other structures of the vertebromedullary region. Therefore, it has a sensitivity and specificity of 85.5%, close to 100% in oncological and inflammatory pathology (3,4).
However, traditionally the clinical and especially radiological evaluation of the spine in general has been limited to the region that is presumed to be affected by various limitations, despite the fact that not all pathological types will affect a single region, such as herniated discs with a greater lumbosacral settlement, spondyloarthropathies in the lower back with the likelihood of involvement in adjacent segments, and others that are clinically silent such as vertebral hemangiomas, located mainly at the dorsal level but also at other levels(5,6).
Based on this, some method is required to visualize the total spine, such as the panoramic sequence or also called panoramic image, which makes it possible to see the spine in a single sequence with modern magnetic resonance imaging systems. This allows the acquisition of images in the sagittal plane of the entire axis of the spine, taking only a few additional minutes compared to the traditional examination, without the need for repositioning the patient, and only planning it from the acquisition station in the MRI Scanning Room, where the acquisition time will vary according to each sequence (7,8).
The technique is based on a direct application of the Composing Software, which allows to show an image resulting from other sequences that were acquired in advance. This was traditionally only done in a later post-processing of images, but now it can be obtained automatically by pre-planning the sequences of interest in alignment with what your acquisitions are achieved with the composite image minutes later. This possibility means a notable optimization in terms of the use of extra time and additional platform for image post-processing (8,9).
Considering that the T2 sequence is a pattern and a basic part of any study of the spinal cord, the fact of using a panoramic sequence enhanced in T2 would be of great contribution and utility to the usual study of the lumbosacral spine; this is because it would allow additional information to be obtained. Therefore, its analysis would serve as a recommendation to opt for its performance due to its contribution and benefit in the diagnosis. In view of this, the objective was to analyze the application of this sequence for the study of the lumbosacral spine by magnetic resonance imaging (MRI).
METHODS
Study design
A retrospective and cross-sectional study was carried out, from January to June 2016, in a group of adult patients whose ages were between 18 and 60 years of age. An MRI study of the lumbosacral spine from an outpatient consultation at a private health services institution in Lima was performed.
Population and sample
The population was made up of 357 patients who had MRI of the lumbosacral spine, whose sample was obtained with the proper formula for a finite population:
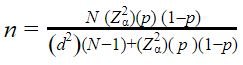
|
Collection and evaluation instrument
A collection sheet was applied, consisting of a general sheet and an analytical sheet, the data of which were filled in considering the request for a radiological study and the examination performed respectively, using the systematic observation technique. The first sheet allows collecting basic data such as gender and stage of life of the patient, as well as the diagnostic presumption to perform the examination, and the second sheet collects if findings were presented and in which pathological groups and subgroups they could be classified. The examinations were carried out on a Siemens MAGNETOM Aera 1.5 Tesla MRI scanner, using the Spine 32 antennas (attached to the equipment table) and Body 18 (placed at the abdominal level referring to the lumbosacral spine), in which the study was acquired specific in its usual form as well as panoramic T2 Sequence using just an additional 3:37 minutes.
Statistical analysis
A data matrix was prepared using the Microsoft Excel 2016 software for the corresponding collection, creating contingency tables with a subsequent verification of the data obtained. For processing, the statistical software R for Windows, Version 3.1.2, was used, making the corresponding frequency distribution for the different findings and allowing the calculation of means and trends. Likewise, the normal distribution was verified in the data obtained by means of the Kolmogorov-Smirnov test and with this apply the hypothesis test for a proportion, considering:
- Null hypothesis (H0): The acquisition of the panoramic T2 Sequence in the lumbosacral spine does not allow 50% more findings to be located in contrast to a routine examination.
- Alternative hypothesis (H1): The acquisition of the panoramic T2 Sequence in the lumbosacral spine does allow 50% more findings to be located in contrast to a routine examination.
The study was carried out based on ethical considerations and good practices, with the authorization of the Academic and Research Directorate of Clínica Internacional, from whose San Borja headquarters the radiological examinations were obtained after coordination with the headquarters of the Center for Diagnostic Imaging and Supervision of the Magnetic Resonance Area, respecting the confidentiality of the information collected for the exclusive use of this investigation.
RESULTS
The ages of the patients who had magnetic resonance imaging ranged from 18 to 60 years and the median achieved was 40 years. Reviewing the selected cases based on life stage, adults themselves (from 31 to 60 years) were 80.1%, while young adults (from 18 to 30 years) represented 19.9%. Likewise, the female gender constituted 53.8% and the male gender 46.2%, and in which total of cases the most frequent diagnostic presumption was the herniated discs, with 52.7%.
In general, of 186 examinations in total, there were 5 cases that presented a normal diagnosis in the traditional study and with the application of panoramic T2 sequence. Therefore, the remaining 181 cases had some finding, regardless of the acquired segment of the spine. Of these 181 mentioned, the usual lumbosacral study had a total of 414 findings.
In the lumbosacral spine, degenerative pathologies were seen as the most frequent findings, occurring in 93% of cases. Of these, herniated discs were the most common with 57%, the majority of which comprised disc extrusion in 40.6%. Likewise, there were disc protrusion in 37.9% and in fewer disc migration with only 21.5%, continuing with lumbar disc degeneration and modic changes with 19.5% and 9.9% respectively, having as a finding less frequent to spondylolysis with only 0.5%. The other findings were congenital anomalies (5.3%) and neoplastic pathology (1%, represented by hemangiomas as the only type of tumor) and, with less than 1% of cases, there were inflammatory pathologies (0.5%) and traumatic injuries (0.2%). Among the congenital anomalies, the so-called transition anomalies stood out, such as lumbarizations in 50% (conversion of the S1 vertebra) and sacralizations in 36.4% (conversion of the S5 vertebra). Herniated discs located in the lumbosacral spine were 52.9%: disc extrusion accounted for 21.5%, disc protrusion accounted for 20%, while only 11.4% were disc migration, given in 167 patients (Table 1).
Table 1. Findings obtained by routine study by MRI of Lumbosacral spine
| Type of Pathology in Lumbosacral Spine | ||||||||
|---|---|---|---|---|---|---|---|---|
| Specific diagnostic findings |
Degenerative | Congenital | Neoplastic | Total | ||||
| n | % | n | % | n | % | n | % | |
| Disc protrusion | 83 | 21,6% | 83 | 20,0% | ||||
| Disc extrusión | 89 | 23,1% | 89 | 21,5% | ||||
| Disc migration | 47 | 12,2% | 47 | 11,4% | ||||
| Disc degeneration | 75 | 19,5% | 75 | 18,1% | ||||
| Modic type II | 21 | 5,5% | 21 | 5,1% | ||||
| Modic type I | 17 | 4,4% | 17 | 4,1% | ||||
| Schmorl's nodes | 7 | 1,8% | 7 | 1,7% | ||||
| Spondylolysis | 2 | 0,5% | 2 | 0,5% | ||||
| Other degenerative types | 44 | 11,4% | 44 | 10,6% | ||||
| Lumbarization | 11 | 50,0% | 11 | 2,7% | ||||
| Sacralization | 8 | 36,4% | 8 | 1,9% | ||||
| Other congenital types | 3 | 13,6% | 3 | 0,7% | ||||
| Hemangioma | 4 | 100% | 4 | 1,0% | ||||
| Other types Neoplastic | 0 | 0% | 0 | 0% | ||||
| Other pathologies Vertebromedullary | 3 | 0,7% | ||||||
| Totals by types | 385 | 100% | 22 | 100% | 4 | 100% | 414 | 100% |
| Absolute total | 385 | 93,0% | 22 | 5,3% | 4 | 1,0% | 414 | 100% |
Likewise, it is worth mentioning that the application of panoramic T2 sequence in the 181
previously mentioned cases allowed to denote additional findings at the cervical spine and dorsal spine,
which were 117 and 71, that is, 188 additional findings, thus constituting a total of 602 findings when
acquiring the MRI exam with the panoramic sequence included.
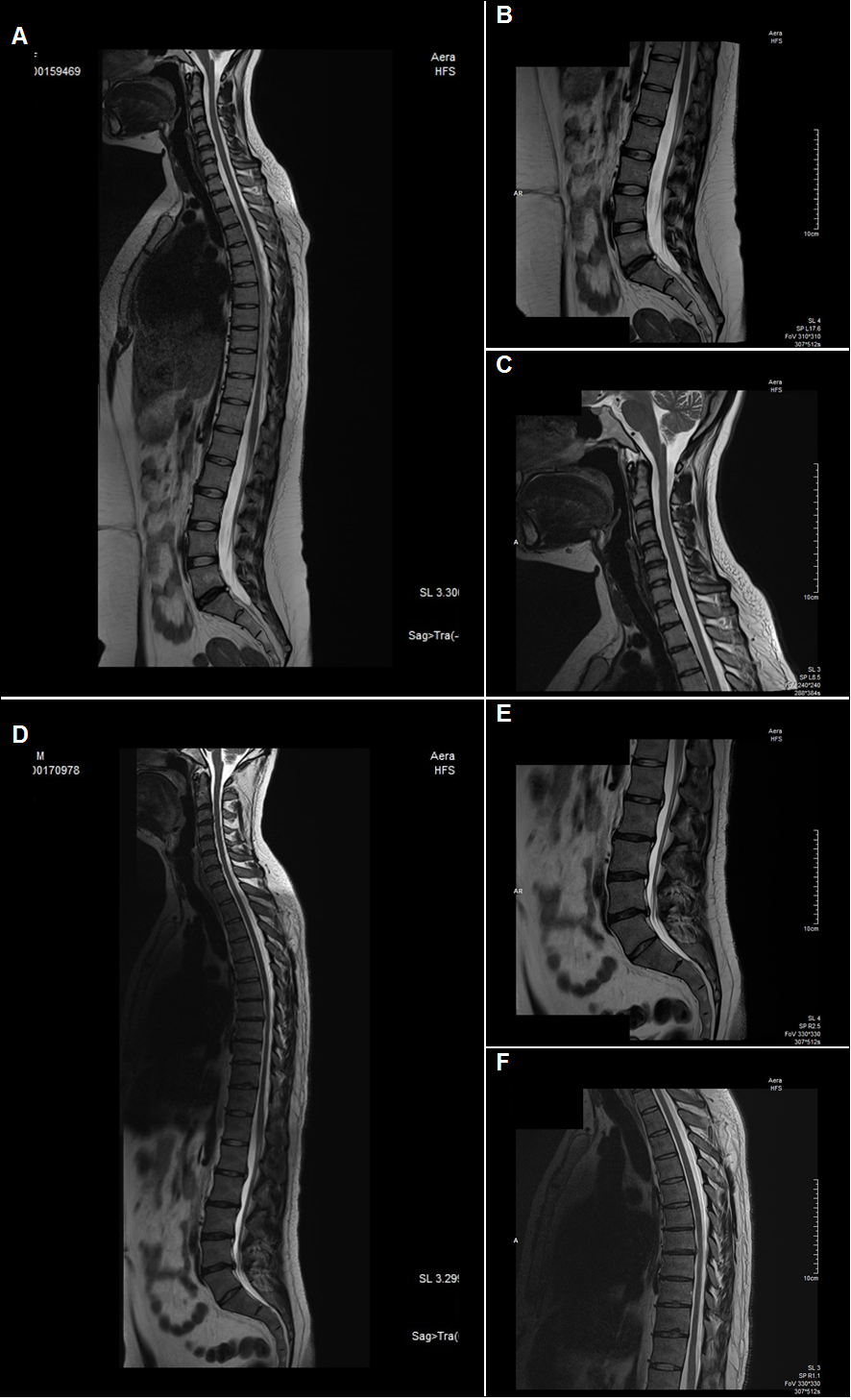
At the level of the cervical spine, there were basically degenerative pathologies in 99.1%,
highlighting herniated discs with 59.5%. Of this total, 58% comprised disc protrusion (especially in the
C5-C6 disc), disc extrusion in 39.1% and finally disc migration in 2.9% (Figure 1),
followed by 28, 4% due to disc degenerations. It should be mentioned that congenital anomalies were also
presented in 0.9%, represented by hydrosyringomyelia. It should be noted that localized hernias
accounted for 59% of cervical lesions, which in turn included disc protrusion in 34.2%, while 23.1%
consisted of disc extrusion and only 1.7% were disc migration (Table 2).
In the dorsal spine there was also a higher percentage of degenerative pathologies with a
frequency of 81.7%, where herniated disc predominated in more than half of the cases (51.7%), including
disc protrusion with 70% (especially in the D7-D8 disc) and disc extrusion with 30% (Figure 1); apart from Schmörl's nodules with 24.1% and disc degenerations with
20.7%. The remaining 18.3% in the dorsal segment corresponded to neoplastic pathologies, whose lineage
was specifically vertebral hemangioma. The dorsal hernias presented were 42.3% of the total findings,
comprising disc protrusion and disc extrusion in 29.6% and 12.7% respectively. Therefore, the main
findings located outside the lumbosacral spine were hernias, which occurred in 77 patients, both at the
cervical level, with 59%, and at the dorsal level with 42.3% (Table 2).
Table 2. Findings obtained outside the Lumbosacral spine by Panoramic T2 sequence Panorámica
|
Type of Pathology outside the Lumbosacral spine |
|||||||||
|---|---|---|---|---|---|---|---|---|---|
| Specific diagnostic findings | Degenerative | Congenital | Neoplastic | Total | |||||
| n | % | n | % | n | % | n | % | ||
| Findings in the Cervical Spine |
Disc protrusion | 40 | 34,5% | 40 | 34,2% | ||||
| Disc extrusion | 27 | 23,3% | 27 | 23,1% | |||||
| Disc migration | 2 | 1,7% | 2 | 1,7% | |||||
| Disc degeneration | 33 | 28,4% | 33 | 28,2% | |||||
| Other degenerative types | 14 | 12% | 14 | 12% | |||||
| Hydrosyringomyelia | 1 | 100% | 1 | 0,9% | |||||
| Other congenital types | 0 | 0% | 0 | 0% | |||||
| Totals by type | 116 | 100% | 1 | 100% | 117 | 100% | |||
| Absolute total at Cervical level | 116 | 99,1% | 1 | 0,9% | 117 | 100% | |||
| Findings in the Dorsal Spine |
Disc protrusion | 21 | 36,2% | 21 | 29,6% | ||||
| Disc extrusion | 9 | 15,5% | 9 | 12,7% | |||||
| Schmorl's nodes | 14 | 24,1% | 14 | 19,7% | |||||
| Disc degeneration | 12 | 20,7% | 12 | 16,9% | |||||
| Other degenerative types | 2 | 3,4% | 2 | 2,8% | |||||
| Hemangiomas | 13 | 100% | 13 | 18,3% | |||||
| Other neoplastic types | 0 | 0% | 0 | 0% | |||||
| Totals by type | 58 | 100% | 13 | 100% | 71 | 100% | |||
| Absolute total at Dorsal level | 58 | 81,7% | 13 | 18,3% | 71 | 100% | |||
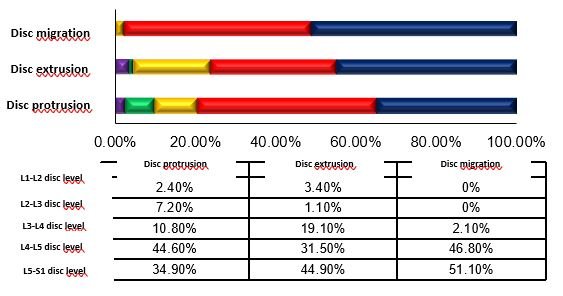
Regarding the location of herniated discs at the level of the lumbosacral spine, which has been the most frequent lesion, it occurred mainly at the level of the L5-S1 disc in 42% of cases, although it also occurred in the other intervertebral discs: L4- L5 with 39.7%, L3-L4 with 12.3%, L2-L3 with 3.2% and L1-L2 with 2.3%. The L5-S1 disc was the main location of disc extrusion and disc migration, with 44.9% and 55.1% respectively, unlike protruding hernias located mainly in the L4-L5 disc, with 44.6% (graphic 1).
The application of the panoramic T2 image for examination of the lumbosacral spine by magnetic resonance imaging was verified using hypothesis testing for a proportion, taking into consideration that, as H0, the technique does not allow 50% more findings to be located than in a regular examination, and that, as H1, the technique does allow 50% more findings to be located in contrast to a regular test. In this way, the Sig value of the corresponding Zcal was obtained from the findings at the level of the lumbosacral segment in the conventional exam and the amount of findings obtained by adding the panoramic T2 sequence, obtaining Sig = 0.031, which being less than 0.05, rejecting the null hypothesis and therefore at 95% confidence level, it can be stated that the application of this. This sequence does allow 50% more findings to be located, showing that it is useful for MR imaging of the lumbosacral spine.
DISCUSSION
The results demonstrate that the application of the panoramic T2-weighted sequence for the lumbosacral spine examination is valid. Therefore, the importance of magnetic resonance imaging in the evaluation of the spine is first reaffirmed, as stated by Aroche (10) and Medina (11). Second, that requests for examination with a specific presumption justify their performance for a due evaluation, since they allow to see early changes and/or incipient lesions and thus have a clinical relevance, as explained by Fretes (12), Kovacs (13), Millán and Cols (14), and Rodríguez (15).
Analyzing, the hypothesis verification defined that 50% more findings are located with the panoramic sequence in question, unlike the usual study. This is similar as reported by Méndez (16), which obtained 74.8% of additional findings using STIR sequence, applying post-process after examination and considering elderly patients. In addition, what is proposed by Schiappacasse (17) and Campos (18) is supported, where it was proposed to use a sagittal sequence for the entire column. It also confirms what was concluded by Burbano (19) and Campos (18), where the T2-weighted image was superior for the various anomalies. In relation to this, what was expressed by Tito (20), is corroborated, who indicated the importance of including this sequence in the examination of an image that reveals adjacent lesions to those presented in the specific initial evaluation segment.
Reviewing the findings, there was the presence of a greater number of degenerative pathologies, with 93% of findings. The main ones were herniated discs, with a frequency of 60%, which coincided with the studies by Ortega (21) at the Centro Médico Ecatepec, of the Instituto Mexicano de Seguridad Social, with the studies by González (22) at the Hospital Universitario Nacional de Colombia, and with the findings of Enríquez (23) in the Clínica Pichincha, whose results were also the most outstanding, with 40.2%, 33.7% and 32.7% respectively. The highest percentage were disc extrusion, in 40.6%, then protruding hernias, with 37.9%. These findings were different and at the same time with a lower percentage compared to the studies by Ortega (21) and González (22), as well as the study of hernias carried out by Solano and Ávila (24) at the Hospital Carrasco de Cuenca, of the Instituto Ecuatoriano de Seguridad Social, in which disc protrusions were mainly presented, with figures equivalent to 73.3%, 87.6% and 96.7% in each case.
Similarly, it was found that the main location of the different types of hernias presented was mainly at the level of the L5-S1 disc in 42% of cases. This result coincided with the theses of Gil (25) in a Sanitary Production Company of Lima, with those of Rivero (26) in the Hospital Nacional Dos de Mayo of the Ministry of Health, with those of Quispe (27) in the Clínica La Luz de Lima, that of Medina (28) in the Hospital Nacional “Ramiro Prialé Prialé”, of the Social Security - EsSalud, and with those of Román (29) in the Hospital Nacional “Luis N. Sáenz” of the Peruvian National Police, in whose results it was also the main location, with 66%, 62%, 39.1%, 34.4% and 34% respectively, fully endorsing that it is the most affected intervertebral disc in people regardless of the activity that could develop and the population group to which they could belong.
Likewise, findings were obtained in both the cervical and dorsal spine, acquiring the panoramic T2 sequence. In both segments, the highest frequency was also given by herniated discs presented in 59.5% and 51.7% of cases, respectively. With this, it is confirmed that herniated discs are the most frequent pathology of the entire spinal axis, and not only at the lumbosacral level. Clinically, the latter is the area with the greatest symptomatological settlement due to the presence of some typical risk factors of the activity, workload or rhythm of people's lives.
CONCLUSION
Through the present investigation, it was reaffirmed that the lumbosacral spine resonance is a valuable exam because it allows the discard and/or evaluation of multiple findings with precision through the possibility of differentiation. Degenerative entities are the most frequent, and it was shown that the acquisition of the panoramic image in T2 is useful because it helps to locate a greater number of conditions at the general level of the spine as in non-contiguous segments. Therefore, this sequence should be considered as a fundamental element to find additional information that contributes to a better diagnosis, compared to the usual lumbosacral magnetic resonance.
In this way, it was determined that the application of the panoramic T2 Sequence for lumbosacral magnetic resonance is absolutely functional and useful in the diagnostic evaluation because it allows locating 50% more additional findings compared to the usual study of the lumbosacral segment. The main findings in the lumbosacral segment, as well as at the cervical and dorsal level, were degenerative diseases, predominantly herniated discs in a greater proportion. The most frequent lumbosacral location was the L5-S1 disc.
Authorship Contributions: ARM: Conception and design of the article, collection of
information, review of magnetic resonance imaging examinations, analysis and interpretation of
results, and writing of the manuscript; RRA: Planning and technical-administrative advice on the
article, statistical advice, critical review of the manuscript, and final approval of the
manuscript.
Funding sources: Self-financed
Declaration of Non-publication in another indexed journal: We declare that the material
contained in the manuscript has not been previously published or sent to another biomedical
journal.
Conflicts of interest: The authors declare no conflicts of interest.
Received: december 14, 2020
Approved: february 13, 2021
Correspondence: Alexander H. Román Meza.
Address: Cl. Tarata 493. La Perla - Callao.
Telephone number: 949071089 - 4200066
E-mail: alexrom2490@gmail.com
BIBLIOGRAPHIC REFERENCES