ARTÍCULO ORIGINAL
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2021 - Universidad Ricardo PalmaDOI 10.25176/RFMH.v21i1.3460
ANEMIA AND CANCER SURVIVAL, A PERUVIAN 5-YEAR FOLLOW-UP STUDY
ANEMIA Y SUPERVIVENCIA EN PACIENTES CON CÁNCER, UN ESTUDIO PERUANO DE SEGUIMIENTO A 5 AÑOS
Jennyfer E. Garcia Arispe 1,2,a, María Loo-Valverde3,b, Willer Chanduví2,c,Rocio Guillen-Ponce2, Jhony A. De La Cruz-Vargas2,4,d
1 Hospital Nacional de Policía. Lima, Perú.
2 Instituto de Investigación en Ciencias Biomedicas, Universidad Ricardo Palma. Lima, Perú.
3 Hospital Nacional Edgardo Rebagliati. Lima, Perú.
4 Facultad de Medcina Humana, Universidad Ricardo Palma. Lima, Perú
a Physician.
b Pediatric Cardiologist.
c Master in Statistics.
d Physician Specialist in Medical Oncology, Doctor in Medicine.
Introduction: Anemia is a serious public health. Several studies indicate that anemia status is a factor that might influence survival and response to cancer treatment in patients. Objective: To determine the relationship between anemia and 5-year survival in cancer patients. Methods: Observational, analytical, and retrospective cohort study. The sample population consisted of novel diagnosed cancer patients registered for hospital care with their respective follow up from 2014 until 2019. Time to death, presence of anemia, and other variables were evaluated. Survival was determined using Kaplan Meier curves and analyzed using the log-rank test. Hazard ratio and risk were determined in turn using the Cox regression model. Results: 72 patients were included in the study, 79.2% of which correspond to solid neoplasms. Anemia was present at the time of diagnosis in 45.8% of patients. Statistically significant differences were found on survival curves for anemia, severity graded anemia, age, and clinical stage. Anemia showed a significant relation with survival (HR: 3.03; CI: 95; p <0.05) on the adjusted bivariate and multivariate analysis for age over 70 years. Likewise, on the respective adjusted analysis for age and clinical stage, anemia showed a significant relation with survival on patients with solid neoplasms. Overall, 30.3% of patients received some type of treatment for anemia. Conclusion: Anemia is frequently found in cancer patients and is significantly related to 5-year overall survival. Age over 70 and severe anemias were related to higher mortality of cancer patients
Keywords: Anemia; Cancer; Survival; Mortality; Public health . (Source: MESH – NLM)
Cancer is the most common cause of death in high-income countries and the second most common cause of death in low and middle-income countries.1 The International Agency for Research on Cancer (IARC) estimated cancer prevalence for Latin America and the Caribbean was 3 336 468 in 2018.2 Specifically for Peru, IARC estimated that for 2018 prevalence of cancer cases was 150 032, with a mortality of 130 cases for every 100 000 inhabitants.2,3
Disease survival in cancer patients will depend on diverse factors, such as the type of cancer, tumor location, its TNM classification stage, level of differentiation, presence of comorbidities and response to treatment, patient age and performance stage at the time of diagnosis, among others.4
Anemia is a serious public health issue that affects 24.8% of the world population; representing a worldwide indicator of both poor health quality and poor nutrition.5 It has multiple causes, being nutritional deficiency the most frequent one. However, anemia can also be associated with other chronic disorders such as chronic kidney disease, autoimmune diseases, and diabetes mellitus.6 Anemia also constitutes the most frequent hematological finding among cancer patients. It can compromise disease evolution, impacting negatively the patient's quality of life, response to treatment, and potentially life expectancy as well.1,7. Its prevalence can vary between 30 to 90% in oncology patients.8 This variability has been associated with the type of cancer, tumor stage, treatment type with cytotoxic agents, comorbidities, among others.9Prevalence of anemia in patients with hematological cancers and solid tumors are 60-70% and 40%, respectively.10,11. Anemia could be present at the time of cancer diagnosis in up to 40%, and 70% of all cancer patients will present it throughout their disease evolution.12
Several studies indicate that anemia status is a factor that might influence survival and response to cancer treatment in patients. It has been established that tumor hypoxia is common in solid tumors; it is intensified by anemia which in turn leads to treatment resistance due to an imbalance between oxygen supply and consumption, reducing the effectiveness of the treatment.13 Patients with adequate hemoglobin levels have shown better tolerance to surgical treatment and adjuvant therapy. On the contrary, in patients with anemia, it was necessary to correct it in the preoperative period and perform a strict follow-up. Moreover, the presence of anemia favors the development of additional complications during cancer progression of a patient, together with other disparities during the surgical treatment, as well as during the time of general prognosis, increasing the risk of death.14,15 A study in bladder cancer patients found anemia as a strong predictor of mortality in surgically treated patients.6 Optimal minimum hemoglobin levels for cancer patients have not yet been established, but there is evidence to suggest a direct association between a patient's hemoglobin levels and cancer survival. In a study of cervical cancer patients treated with chemo-radiotherapy, a direct and significant relationship was found among hemoglobin levels and survival, reaching a maximum when hemoglobin reached between 11-12 gr/ dL.16 Since the anemic state of a cancer patient influences disease progression, proper management of anemia in cancer patients is important, representing a negative prognostic factor that impairs quality of life. In modern oncology, both survival and quality of life are the main outcomes considered for cancer patients.
This study aimed to determine the relationship between anemia and overall survival in cancer patients treated at the oncology service of the Peruvian National Police Hospital “Luis Nicasio Sáenz”.
METHODS
Design and study area
The proposed analysis considered a longitudinal, observational, and analytical study carried out on a retrospective cohort. In a oncology service of a Peruvian Hospital.
Population and sample The sample was composed of cancer diagnosed with patients who were treated at the oncology service of the Peruvian National Police Hospital “Luis Nicasio Sáenz”, starting in 2014, with a 5-year follow-up until December 2019. Sample selection was carried out through a simple random-probabilistic sampling. Patients included in the study were over 14 years old, with a definitive cancer diagnosis, and treated for the first time in the oncology service during 2014. Patients diagnosed with recurrent cancer, incomplete clinical data, or auxiliary examinations were excluded from the study.
Variables and instruments
The following variables were considered as independent ones: anemia, anemia by severity, and treated anemia; while overall survival estimated in months was considered as the dependent variable. Additionally, the following intervening variables related to survival were analyzed: age, sex, comorbidity, type of cancer, clinical stage, and evolutionary stage of cancer (as active or as in remission).
Procedures
Exposed patients were considered as those having anemia at the time of cancer diagnosis, while not exposed to patients were considered as those without anemia at the time of diagnosis. Patient data collection was obtained from clinical records available at the archive of the Peruvian National Police Hospital "Luis Nicasio Sáenz”. Data were collected until 2019 or until prior death occurrence, whatever event occurred first.
Statistical analysis
Data was processed with the statistical software SPSS and a descriptive analysis of qualitative and quantitative variables was presented using graphs and tables. Overall survival analysis was represented employing Kaplan Meier curves and the level of significance between survival curves was established through the log-rank test. To determine the relationship between anemia and overall cancer survival, bivariate and multivariate analysis was performed with a Cox regression model, obtaining Hazard Ratio values; p values of less than 0.05 were considered statistically significant.
Ethical aspects
The Ethics Committee approved this research project and the head of the Oncology Department of Peruvian National Police Hospital “Luis Nicasio Sáenz” together with Universidad Ricardo Palma´s favorable opinion.17 Principles of the Declaration of Helsinki of the World Medical Association were followed, granting privacy and confidentiality of all patient data.
RESULTS
Overall Results
Overall data was obtained from 213 novel patients registered at the oncology department in 2014 with a definitive cancer diagnosis. Exclusion criteria from the study dismissed cases with incomplete medical records, unavailable data, insufficient laboratory records, patients on pediatric age, benign tumor, or recurrent cancer at the first consultation. A final number of 72 patient cases were finally included for study analysis.
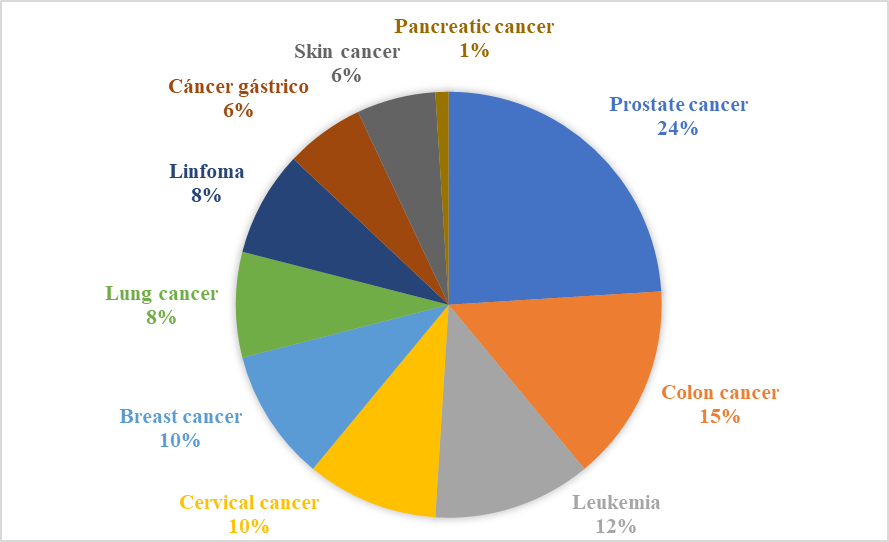
Graph 1 shows the distribution of patients by cancer type. Patients with solid tumors corresponded to 79.8%. Among solid tumors, prostate cancer was the most frequent (24%), followed by colon cancer (15%).
Table 1 shows the descriptive analysis of the qualitative and quantitative variables included in the study by the presence of anemia. A total of 33 patients with anemia were registered, representing 45.8% of the total number of cancer patients. The average age was 64.5 years, and 68.1% of patients were younger than 70 years. Males represented 69.4% of all patients and 78.8% of all patients with anemia. Comorbidities were present in 45.8% of total patients. Concerning the clinical stage of patients with solid tumors, 47.4% corresponds to stage III. Overall, 56.9% of patients presented recurrence or persistence of cancer during follow-up.
Table 1. General characteristics of newly diagnosed cancer patients at Hospital Luis Nicasio Sáenz during 2014 by the presence of anemia.
|
VARIABLE |
TOTAL |
Anemia |
|
|
Yes |
No |
||
|
Total patients |
72 (100%) |
33 (45,8%) |
39 (54,1%) |
|
Age* |
64,52 (13,1) |
66,54 (13,3) |
62,82 (12,93) |
|
Less than 70 years |
23 (31,9%) |
13 (39,4%) |
10 (25,6%) |
|
Over 70 years |
49 (68,1%) |
20 (60,6%) |
29 (74,4%) |
|
Sex |
|
|
|
|
Male |
50 (69,4%) |
26 (78,8%) |
24 (61,5%) |
|
Female |
22 (30,6%) |
7 (21,2%) |
15 (38,5%) |
|
Comorbidity |
|
|
|
|
Yes; |
33 (45,8%) |
19 (57,6%) |
14 (35,9%) |
|
No |
39 (54,2%) |
14 (42,4%) |
25 (64,1%) |
|
Cancer type |
|
|
|
|
Hematological |
15 (20,8%) |
9 (27,3%) |
6 (15,4%) |
|
Solid |
57 (79,2%) |
24 (72,7%) |
33 (84,6%) |
|
Clinical stage (solid type) |
|||
|
I |
4 (7%) |
0 |
4 (12,1%) |
|
II |
19 (33,3%) |
7 (29,2%) |
12 (36,4%) |
|
III |
27 (47,4%) |
12 (50%) |
15 (45,5%) |
|
IV |
7 (12,3%) |
5 (20,8%) |
2 (6%) |
|
Cancer evolutive stage |
|
|
|
|
Remision |
31 (43,1%) |
13 (39,3%) |
18 (46,2%) |
|
Recurrent/persistent |
41 (56,9%) |
20 (60,7%) |
21 (53,8%) |
|
Treated anemia |
|
|
|
|
Yes |
10 (13,9%) |
10 (30,3%) |
|
|
No |
62 (86,1%) |
23 (69,7%) |
39 (100%) |
|
Hemoglobin** |
12,1 (8-12,9) |
8 (6,7-9,7) |
12,8 (12,5-13,8) |
|
HCT** |
35,3 (24,5-38,3) |
24 (19,7-27,2) |
38,3 (36,3-40,4) |
Concerning patients with anemia, 30,3% received some type of specific treatment. The hemoglobin median of all patients was 12,1 gr/ dl. On anemic patients, the median of hemoglobin was 8 gr/ dl, while in the non-anemic patients was 12,8 g/ dl. Hematocrit mean values for all patients and anemic patients were 35,3 and 24,0 respectively.
Raw and Adjusted Bivariate Analysis
For both bivariate and age-adjusted analysis, anemia had respectively a statistically significant relation with survival (HR: 3.03, 95% CI p <0.05). For the analysis of anemia according to severity, severe anemia was significant in both the bivariate analysis (HR: 10.59, 95% CI p <0.05) and the adjusted one (HR: 9.18, 95% CI, p <0, 05); while moderate anemia acquired significance on the adjustment by age (HR: 2.33, p <0.05). Age had a statistically significant relation with survival, for both bivariate analysis and the adjusted one for the presence of anemia. Age over 70 years showed to be a risk factor with lower survival (HR: 3.79, p: 0.000, CI: 1.91-7.48). (Table 2)
Table 2. Cox regression on all study patients.
|
Variable |
Raw HR |
p / IC |
Adjusted HR |
p / IC |
|
|
Anemia (Yes/No) |
2,68 1,35-5,29 |
0,005 1,35-5,29 |
3,03 |
0,002 1,51-6,07 |
|
|
Anemia severity |
Mild |
1,33 |
1 |
- |
1 |
|
Moderate |
2,06 |
0,065 0,955-4,485 |
2,33 |
0,034 1,06-5,09 |
|
|
Severe |
10,59 |
0,000 4,18-26,86 |
9,18 |
0,000 3,56-23,65 |
|
|
Age (> 70 years / ≤ 70 years) |
3,38 |
0,000 1,73-6,61 |
3,79 |
0,000 1,91-7,48 |
|
We continued analyzing according to the type of tumor. In patients with solid tumors, anemia was significantly related to survival (HR: 2.90, p <0.05). Severe anemia showed a significant relation all for the bivariate analysis, the age-adjusted and clinical-stage one (HR: 7.43, p: 0.001). Age over 70 years old was statistically significant throughout the analysis (p <0.05). (Table 3). When analyzing anemia by severity within the group of patients with hematologic malignancies, severe anemia was statistically significant as a factor related to higher mortality (HR: 13.73, p: 0.02, CI: 1.59-118, 02). (Table 4).
Table 3. Cox regression on patients with solid neoplasms.
|
Variable |
Raw HR |
p / IC |
Adjusted HR |
p / IC |
|
|
Anemia (Yes/No) |
2,24 |
0,040 1,03-4,87 |
2,90 |
0,015 |
|
|
Anemia severity |
Moderate |
1,74 |
0,2 0,71-4,28 |
2,80 |
0,041 1,04-7,52 |
|
Severe |
10,01 |
0,000 3,39-29,55 |
7,43 |
0,001 1,85-11,09 |
|
|
Age (>70 years / ≤70 years) |
3,38 |
0,000 1,73-6,60 |
5,06 |
0,000 2,05-12,43 |
|
|
Clinical stage |
II |
1,15 |
0,894 0,14-9,91 |
0,46 |
0,502 0,05-4,32 |
|
III |
2,98 |
0,291 0,39-22,5 |
0,97 |
0,97 0,11-8,51 |
|
|
IV |
6,13 |
0,099 0,71-52.,81 |
2,43 |
0,44 0,25-23,14 |
|
Table 4. Cox regression on patients with hematological neoplasms.
|
Variable |
Raw HR |
p / IC |
Adjusted HR |
p / IC |
|
|
Anemia (Yes/No) |
4,93 |
0,052 0,98-24,61 |
4,56 |
0,06 0,90-23,06 |
|
|
Anemia severity |
Moderate |
3,67 |
0,139 0,65-20,52 |
3,55 |
0,15 0,63-20,04 |
|
Severe |
15,46 |
0,009 1,97-121,3 |
13,73 |
0,02 1,59-118,02 |
|
|
Age (>70 years / ≤70 years) |
2,02 |
0,296 0,53-7,59 |
1,64 |
0,462 0,43-6,26 |
|
Anemia and Survival
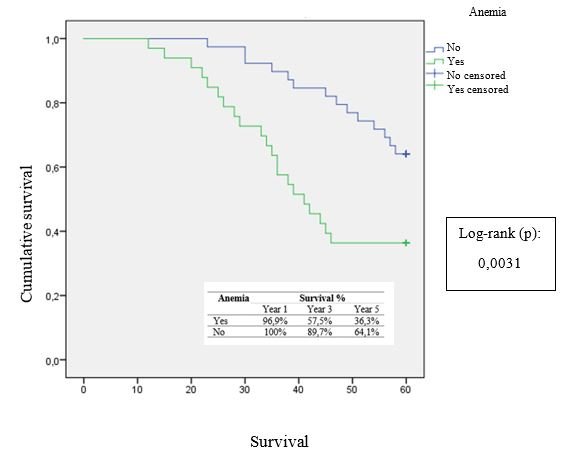
Overall survival analysis at 5 years follow-up showed that patients with anemia had a lower percentage of survival when compared to patients without anemia (36.3% vs 64.1%, respectively). These differences were statistically significant between survival curves (p <0.05). (Graph 2). The 5-year survival rates of patients who received treatment or not for anemia were 60% and 50%, respectively (log-rank test p = 0.716).
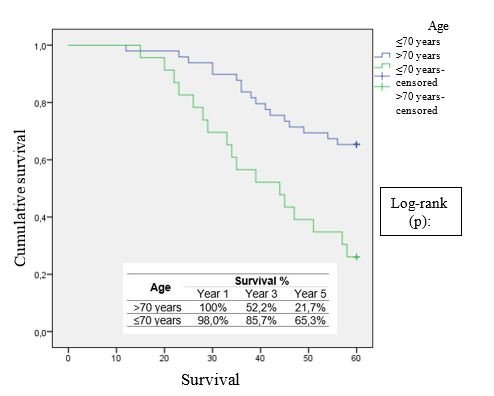
Graph 3 shows the survival curves by age. The highest death proportion occurred in patients older than 70 years, with a 3-year and 5-year survival analysis of 52.2% and 21.7% respectively. The difference between the survival curves was statistically significant (p = 0.000).
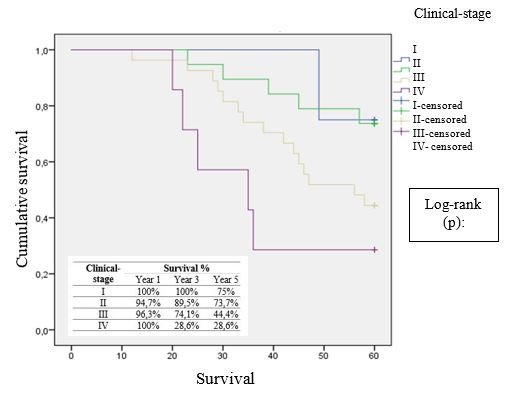
In patients with solid neoplasms, survival was evaluated by the clinical stage (Graph 4). 71.4% of patients on cancer stage IV presented the neoplasm with a lower survival at 3 and 5 years (28.6%). Patients on stage I showed the highest survival at 5 years (75%). The difference between survival curves for each cancer stage was significant, with a p-value of 0.027.
DISCUSSION
Anemia is a frequent finding in cancer patients. The present study found a 45.8% frequency of anemia at the time of cancer diagnosis. This possibly linked to patients diagnosed with gastrointestinal, gynecological, and urological malignancies in which anemia is attributed to chronic bleeding. Similar to what is reported by a retrospective study by Paitan et al.11 for patients with different types of cancer, 46.5% presented anemia at the time of cancer diagnosis. In a separate study conducted in patients with non-Hodgkin lymphoma and Hodgkin lymphoma, anemia occurred in 33.3% of patients at diagnosis.18 Research carried by Väyrynen et al.19, found that for colorectal cancer patients, anemia was present in 43%, being normocytic anemia the most frequent one. Moreover, in patients with gastric cancer, anemia is much more frequent; a recent study conducted in patients with gastric cancer reported the presence of anemia at the onset of symptoms in up to two-thirds of those patients.20
There is a large body of data derived from preclinical investigations that show that hypoxic microenvironments significantly affect solid tumor response to anticancer therapies, promote tumor progression and cancer aggressiveness, and facilitate the spread of tumor cells.21
Concerning clinical and demographic characteristics of cancer patients who presented anemia: 68.1% were younger than 70 years, 78.8% were male, 57.6% had some comorbidity, 72.7% presented solid neoplasms, and 50% of patients were at clinical stage III. A study carried out in cancer patients undergoing palliative treatment had a similar population with 57% of male patients; being gastrointestinal, urological, and pulmonary neoplasms the most frequent ones. The prospective study "European Cancer Anemia Survey" (ECAS), with more than 15,000 cancer patients, evaluated anemic characteristics on these patients, showing that 78% presented solid neoplasms, with a disease recurrence of 43%.22
For the present study, a considerable percentage of anemic patients presented disease recurrence (60.7%). In this regard, current literature refers to the effects of anemia in cancer patients, especially those with solid neoplasms. Within these patients, anemia would condition intra-tumor hypoxia, which in turn would produce radio-resistance, apoptosis inhibition, angiogenesis; and afterward would promote tumor progression, long-distance disease dissemination, and treatment resistance.23 Wilson et al.15 studied preoperative anemia in patients with colorectal cancer, finding a significant relation of less disease-free time after treatment conclusion. Also, together with a different study on colorectal carcinoma, the initial study found anemia to be an adverse factor of both survival and disease recurrence.15,19 Specifically, normocytic anemia was associated with a reduction in overall survival (HR: 1.61, p: 0.023, CI: 1.07-2.42). Anemia subtype for each patient was not determined in this study.
When determining risk by Hazard Ratio (HR), both bivariate and age-adjusted analyses showed that anemia is a factor related to mortality (HR: 3.04, p: 0.002, CI 1.51 -6.09). Even in patients with malignant solid neoplasms, anemia was a prognostic factor that increased 3 times the risk of death (p: 0.008, CI: 1.35-7.05), independent of age and clinical stage. This result is similar to the one reported by Medrano et al.20 in a cohort of 558 patients with advanced gastric adenocarcinoma, where anemia was found to be an adverse prognostic factor for survival (OR: 3.62, p: 0.000, CI: 1.4-13.8). Similarly, Paitan et al.11, showed that when adjusting the lack of anemia to other variables, it demonstrated to be an important protective factor to explain survival (HR: 0.6, p: <0.001, CI: 0, 5-0.8). Last but not least, on a study carried on patients with different stages of cervical cancer, anemia showed a significant difference in mortality: in patients with hemoglobin values above and below 12 gr/ dl, the 5-year survival was 82% and 44% respectively.16
For the analysis of anemia by the level of severity, severe anemia (defined as hemoglobin values lower than 7gr/ dl) was significantly related with shorter survival in both the bivariate and the adjusted analysis for age and for clinical stage (HR: 9, 77, p: <0.01, CI: 3.73-25.61). Only a few studies have been carried out on the analysis of anemia according to severity. Jiménez et al.18 carried out a case-control study in patients with acute lymphoblastic leukemia, where they found that 36.2% of patients had severe anemia; however, it was not found to be an unfavorable prognostic factor. In contrast, a different study conducted in patients with advanced lung cancer found severe anemia as an independent factor associated with prognosis.24
Anemia is a major source of morbidity and mortality worldwide. Meta-analysis studies conducted in patients with different types of cancer have shown that anemia, independent of its severity is associated with a shorter survival during cancer disease. The previous has been demonstrated in patients with solid neoplasms such as colorectal, pulmonary, cervical, prostate, head, neck, and hematological neoplasms such as lymphoma and multiple myeloma.15,16,25
As for additional factors associated with cancer survival analyzed in this study, age over 70 years old was a factor significantly associated with lower cancer survival (HR: 3, p <0.020, CI: 1.18-7.601), especially in patients with solid malignancies (HR: 4.73, p: 0.009, CI: 1.46-15.27). In the study carried out by Valencia et al.26 in patients with pancreatic cancer, age over 55 years was associated with an increase in patient mortality (HR: 11.3). Advanced age is one of the most severe risk factors for mortality in many types of cancer.27 Considering that the prevalence of anemia increases with age, adequate management of anemia is detrimental, especially in older patients in which advanced age constitutes a factor that may increase the risk of death.28.
Regarding the treatment of anemia, only 30.3% of the patients received specific therapy. This is consistent with the results of the ECAS study, where only 40% of cancer patients received iron supplements, transfusions, or erythropoietin-stimulating agents.22
In this study, the overall 5-year survival rate of patients receiving anemia treatment compared to those not being treated was 60% and 50% respectively, representing a non-significant difference. In that respect, a retrospective study of pancreatic cancer patients analyzed the prognostic value for blood transfusions26, finding an association with shorter survival and worse prognosis (HR: 4.6, p: 0.027). The previous is due to the immunomodulatory effects of blood transfusion which may influence the control of the disease. On the contrary, a different study of patients on palliative treatment patients showed that blood transfusion was significantly associated with survival.4.
Blood transfusions in anemic patients before radiation therapy initially appear to have improved treatment outcomes, but the HIV epidemic in the 1980s brought many unintended transfusion infections29 in addition to complications from immunomodulation.30 Erythropoietin therapy was later developed as an alternative method. However, several clinical trials failed to demonstrate improvements of radiation treatment, even with an added negative effect on survival.31,32
Anemia is the most common hematologic manifestation of cancer and affects the majority of cancer patients. Its incidence increases with the administration of oncological chemotherapy/ radiotherapy treatments. Anemia reduces the quality of life and shortens survival in cancer patients. A positive correlation was observed between anemia and tumor hypoxia. Experimentally, hypoxia improves tumor growth and resistance to therapy by stimulating angiogenesis, accumulation of genomic mutations, the increment of resistance to apoptosis and to destructive effects of free radicals generated by chemotherapy/ radiotherapy.32 Every study indicated positive correlations between reduced hemoglobin and higher levels of tumor hypoxia with a poor prognosis. Attempts of treatments by radiosensitization by enhanced tumor oxygenation or hypoxic cell sensitization (through hyperbaric oxygen), electrophilic radiosensitizing, pharmacological agents, and mitomycin had limited success.33. In the current era of multimodal cancer therapy, the prevalence of treatment-related anemia is likely to increase even though exact estimates are difficult to predict.
The current study has the limitations of a retrospective, single-center cohort study with a specific population. Medical records not always contained required information for research, which led to the exclusion of a large number of patients’ files. The limited sample size did not allow us to analyze other factors that influence survival.
CONCLUSIONS
Anemia is a frequent manifestation in cancer patients and is significantly related to overall 5-year survival. Severe anemia, age over 70 years, and advanced clinical stage were related to higher mortality. Further prospective confirmatory studies are necessary.
Conflicts of interest: Authors declare no conflicts of interest. This work corresponds to a thesis developed during Curso Taller de Tesis, at Universidad Ricardo Palma.
Funding sources: Self-financed.
Authorship contributions: The authors participated in the genesis of the idea, project design, data collection and interpretation, analysis of results and preparation of the manuscript of this research work.
Received: November 22,2020
Approved: January 03, 2021
Correspondence: Maria Loo-Valverde.
E-mail: maryloovalverde@gmail.com
REFERENCES