CASE REPORT
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2021 - Universidad Ricardo PalmaDOI 10.25176/RFMH.v21i2.3651
SPONTANEOUS PNEUMOMEDIASTINUM IN PATIENTS WITH COVID-19. CASE REPORT.
NEUMOMEDIASTINO ESPONTÁNEO EN UN PACIENTE CON COVID-19. REPORTE DE CASO.
Pedro Paolo Sotelo-Jiménez(1,a), Enrique Moyano Navarro(1,a), Félix Tipacti Rodríguez(2,a), Carlos Milla Bravo(3,c)
1 Departamento de Medicina Interna, Hospital Nacional Edgardo Rebagliati Martins, Essalud, Lima-Peru.
2 Departamento de Cirugía de Tórax y Cardiovascular, Hospital Nacional Edgardo Rebagliati Martins, Essalud, Lima-Peru.
3 Departamento de Radiología, Hospital Nacional Edgardo Rebagliati Martins, Essalud, Lima-Peru.
a Physician Specialist in Internal Medicine.
b Physician Specialist in Thoracic Surgery.
c Physician Specialist in Interventional Radiology.
Introduction: Pneumomediastinum is an infrequent and rare pathology. The typical radiological manifestations in patients with SARS-CoV-2 pneumonia consist of the presence of bilateral pulmonary opacities, of peripheral distribution. In a recent series of patients with COVID-19, it indicates that 1% of patients can develop spontaneous pneumomediastinum as a complication, it is generally benign and it is not yet clear that this may be an indicator of worsening. Clinical Case: This is a 43-year-old male patient who presented a 15-day illness characterized by pharyngeal pain, fever, chest pain and respiratory distress, receiving multiple antiviral and antibiotic treatment schemes without response, for which he attended to Rebagliati Hospital where he was found respiratory failure, hypoxemia and sepsis. His tomography was compatible with ground glass infiltrate, areas of bilateral lung consolidation, and pneumomediastinum. It did not require surgical treatment and it evolved favorably to pneumonia with a decrease in inflammatory markers and remission of pneumomediastinum in tomographic control. Conclusion: This report highlights that in COVID-19 infection the pulmonary complications to take into account are bilateral pneumonia, bacterial coinfection, sepsis and spontaneous pneumomediastinum.
Keywords: Spontaneous Pneumomediastinum, COVID-19, Case Report. (Source: MeSH – NLM)
RESUMEN
Introducción: El neumomediastino es una patología poco frecuente y rara. Las manifestaciones radiológicas típicas en los pacientes en neumonía por SARS-CoV-2 consiste en la presencia de opacidades pulmonares bilaterales, de distribución periférica. En una reciente serie de pacientes con COVID-19 indica que el 1% de los pacientes pueden desarrollar neumomediastino espontáneo como complicación, generalmente es de curso benigno y no se aclara aún que ello puede suponer un indicador de agravamiento. Caso Clínico: Se trata de un paciente varón de 43 años que presentó un tiempo de enfermedad de 15 días caracterizado por dolor faríngeo, fiebre, dolor torácico y dificultad respiratoria, recibiendo múltiples esquemas de tratamiento tanto antiviral y antibióticos sin respuesta, por lo que acudió al Hospital Rebagliati donde se le encontró insuficiencia respiratoria, hipoxemia y sepsis. Su tomografía fue compatible con infiltrado en vidrio deslustrado, áreas de consolidación pulmonar bilateral y neumomediastino. No requirió tratamiento quirúrgico y evolucionó favorablemente a la neumonía con disminución de marcadores inflamatorios y remisión de neumomediastino en control tomográfico. Conclusión: Este reporte resalta que en la infección por COVID-19 las complicaciones pulmonares a tener en cuenta son la neumonía bilateral, coinfección bacteriana, sepsis y neumomediastino espontáneo.
Palabras Clave: Spontaneous Pneumomediastinum, COVID-19, Reporte de Caso. (Fuente: DeCS-BIREME)
Spontaneous pneumomediastinum (SPM) or Hamman's syndrome is a secondary complication to increased intra-alveolar pressure that causes alveolar rupture and air outflow from the bronchial tree to the mediastinum(1), which in turn can spread to the subcutaneous tissue, exceptionally at the endothoracic and peritoneal levels, or even to the spinal canal(1,2).
It was first described in 1939 as a very characteristic but infrequent sign consisting of crepitus concomitant with the heartbeat and is perceived during auscultation of the anterior thoracic region (Hamman's sign)(3). The predisposing conditions which have been described are interstitial pulmonary and chronic obstructive diseases, bronchial asthma, bronchiectasis, trauma and thoracic procedures, mechanical ventilation, inhaling toxic substances, foreign body, chesty cough, labor and lung cancer. The probability to develop such pathology is a consequence of respiratory infections with severe cough as it is in the case of infection by coronavirus SARS-CoV-2(2,4).
CLINICAL CASE
A 43-year-old male patient from Lima with a history of overweight. He denied tobacco use and previous pulmonary diseases. He was in direct epidemiological contact five days prior with his brother who had been infected by coronavirus.
He presented a 15-day illness characterized by pharyngeal pain, general discomfort, moderate frontoparietal cephalea, fever, anosmia and ageusia. He received ambulatory treatment with multiple schemes: clarithromycin, hydroxychloroquine, ivermectin, levofloxacin (stopped due to allergic reaction) and intravenous ceftriaxone without clinical response until he developed chest pain, lingering cough with greenish sputum and progressive respiratory distress four days prior to hospital admission. Due to this, he attended the emergency department at CELIM - Hospital Nacional Edgardo Rebagliati Martins (HNERM) reaching oxygen saturation (Sat02) at 86%. It was initially diagnosed as acute respiratory failure and atypical pneumonia caused by COVID-19 requiring oxygen therapy by mask with a reservoir bag. There was no history of invasive procedures in the thoracic area.
Physical assessment: Blood pressure: 100/60 mmHg, Heart rate: 110 heartbeats per minute, Respiratory rate: 28 breaths per minute, receiving 15 liters of oxygen per minute (Oxygen saturation: 93%), in poor general conditions, supraclavicular subcutaneous emphysema and erythematous papular lesions on the back and shoulders were palpated.
Thorax: decreased vesicular murmur and crepitus in both lung bases.
Ancillary testing at the time of admission showed: leukocytes: 20,130; lymphocytes: 840; hemoglobin: 13.3 g /dl; platelets: 1049,000; glucose: 87mg/dl; creatinine: 1.09 mg/dl; fibrinogen: 976mg/dl; D-Dimer: 0.46 ug/ml; CPK MB: 0.59; Troponin: 0.008; LDH: 402 U/L; CRP: 14.47 ng/ml; Ferritin: 1663 ng/ml. PaFiO2: 102. Lactate:1,2. lgM Rapid Test, Molecular PCR test positive for SARS-CoV-2.
Blood cultures for common germs were negative for bacterial growth.
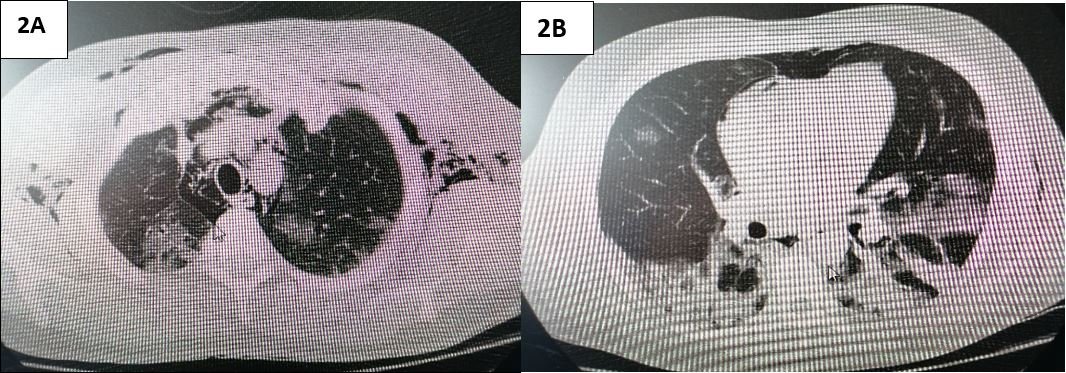
The chest tomography scan showed areas of alveolar infiltrate in tarnished glass, bilateral consolidation with 50% pulmonary compromise, as well as subcutaneous emphysema and pneumomediastinum (Figure 1 and Figure 2).
Figure 1. 1A: chest x-ray showing bilateral pulmonary infiltrates and gas in subcutaneous tissue at cervical level. 1B: chest tomography scan showing subcutaneous cervical emphysema.

Figure 2. 2A: chest tomography scan showing dissection of subcutaneous emphysema at thoracic and axillary levels, pneumomediastinum and bilateral ground-glass images. 2B: chest tomography scan showing pneumomediastinum, bullae, ground-glass areas and marked consolidation at the lung bases.
Upon medical assessment by the Thoracic Surgery Department, it was concluded he did not require a special surgical procedure and only conservative management and observation was needed.
He was given 250 mg of methylprednisolone every 24 hours for 5 days, 60 mg of enoxaparin subcutaneously every 24 hours, 4.5 g of piperacillin/tazobactam intravenously every 6 hours for 10 days, progressive weaning of oxygen therapy and strict monitoring of oxygen saturation.
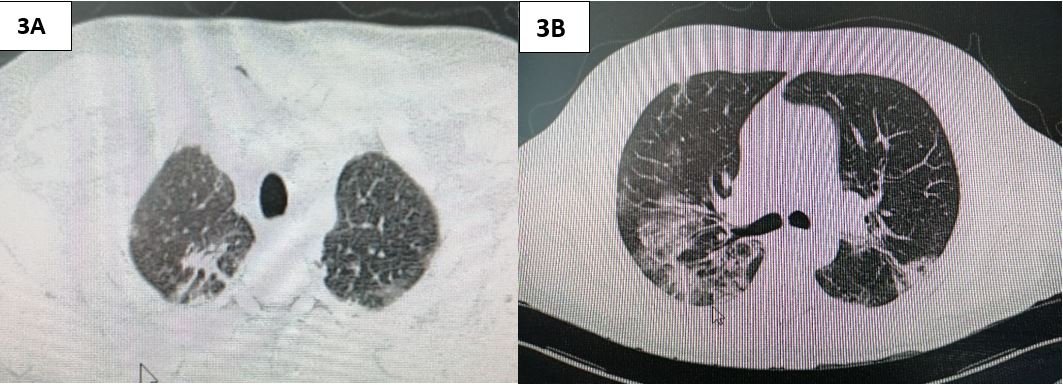
He progressed favorably and his medical controls two weeks after showed gas disappearance in soft tissues at cervical and mediastinum levels, bilateral evolutive consolidations (Figure 3).
Figure 3. 3A: chest tomography scan showing remission of pneumomediastinum and a 15-days subcutaneous emphysema. 3B: chest tomography scan showing evolving pulmonary consolidations with some fibrous tracts.
Analytics of improvement: hemogram with with 8726 leukocytes, 1700 lymphocytes, Hb 12 g/dl; 300,000 platelets; LDH 204 ng/ml; CRP <0.4 U/L; ferritin: 593 ng/ml.
He was discharged 18 days after, hemodynamically stable, no fever, with oxygen saturation at 97% and no use of supplemental oxygen.
DISCUSSION
Pneumomediastinum is an infrequent and rare pathology with an incidence of 1:44000 hospital admissions. It is over 70% more frequent in young males(5), generally originating from air migration from the ruptured alveoli to the mediastinum through the Macklin effect(6).
The typical radiological manifestations in patients with SARS-CoV-2 pneumonia consist of the presence of bilateral ground-glass pulmonary opacities, peripheral distribution, consolidations and pulmonary thromboembolism in some cases(5).
In this case, our patient used several drugs (antimicrobials) on an outpatient basis with no proven efficacy at the present time. According to a meta-analysis, only 3.5% of patients present bacterial co-infection at the time of admission while 15% of them present it during hospital stay, and more than 71% were prescribed antibiotics, all of which generates bacterial resistance, adverse reactions and unnecessary costs(7) as a consequence.
A recent series of patients with COVID-19 indicates that 1% of patients can develop spontaneous pneumomediastinum as a complication(8) and, although the exact mechanism by which spontaneous pneumomediastinum occurs in SARS-CoV-2 pneumonia is unknown, it is attributed to intense coughing or valsalva maneuvers. In theory, it is considered a self-limited and benign condition which responds favorably to conservative therapeutic measures in most cases(7), but it requires observation and continuous follow-up when there is a predisposing pulmonary disease due to the possibility of related cardiovascular and respiratory complications. Therefore, further research is needed to determine its prognostic significance and, in case it becomes a marker of disease progression in COVID-19 infection, measures or specific recommendations(4,7) should be established.
CONCLUSION
This case report stresses the pulmonary complications to be considered in patients infected by COVID-19, such as bilateral pneumonia, bacterial coinfection, sepsis, respiratory failure and spontaneous pneumomediastinum. The treatment for this last mentioned is observation and continuous monitoring, especially in patients who show disease progression.
Authorship Contributions: The authors participated in the generation, writing and final approval of the original article, as well as in data collection.
Funding sources: Self-financed.
Conflicts of Interest: The authors declare no conflicts of interest.
Received: August 20, 2020.
Approved: February 15, 2021.
Correspondence: Dr. Pedro Paolo Sotelo Jiménez.
Address: Domingo Cueto N°120, Jesús María. Lima, Perú.
Telephone: 2654901- anexo 3149/ 3415 y 999 675 855
E-mail: pepasoji@hotmail.com
BIBLIOGRAPHIC REFERENCES
