ARTÍCULO ORIGINAL
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2021 - Universidad Ricardo PalmaDOI 10.25176/RFMH.v21i2.3656
PRENATAL FACTORS ASSOCIATED WITH BREACH OF THE BASIC VACCINATION SCHEME IN UNDER 5 YEARS OF AGE
FACTORES PRENATALES ASOCIADOS AL INCUMPLIMIENTO DEL ESQUEMA BÁSICO DE VACUNACIÓN EN MENORES DE 5 AÑOS
Trinidad L. Isidro-Ríos(1,a), Alfonso Gutiérrez-Aguado(1,b), Jhony A. De la Cruz-Vargas(1,c)
1 Instituto de Investigación en ciencias biomédicas. Facultad de medicina. Universidad Ricardo Palma
a Bachiller de Medicina Humana.
b Magister en Salud pública. Médico cirujano.
c PhD; MCR; MD. ONCOLOGIST. Médico cirujano.
Objective: To determine the prenatal risk factors associated with the failure to comply with the basic vaccination scheme in children under 5 years of age, based on the Demographic and Family Health Survey (ENDES) of 2018. Materials and Methods: It is an observational, retrospective, analytical and transversal study. We study the sample of the National Demographic and Health Survey (ENDES) for 2018 that includes 18 104 children between 1 and 5 years with health card seen in the interview, finding the results in the INEI surveys. The files containing the vaccination scheme questionnaires are selected and the data processed with SPSS version 25. The statistical processing is analytical and descriptive, bivariate and multivariate with the help of STATA v16 and Excel 2016. Results: There was a final sample of 18,104 children between 1 to 5 years old in 2018. The multivariate analysis found the association of non-compliance with the vaccination schedule with the mother's age (p value = <0.01, PR = 1.20, CI = 1.13 - 1.28), the number of controls inadequate (p value = <0.01, PR = 1.28, CI = 1.23 - 1.33) and the pregnant woman did not receive the tetanus vaccine during pregnancy (p= <0.01, RP= 1.16, CI= 1.12 - 1.20). No such association was found with the place of residence, wealth index and natural region. Conclusions: The prenatal risk factors associated with the failure to comply with the basic vaccination scheme in children under 5 years of age were maternal age, the number of inadequate prenatal check-ups and the pregnant woman who had not received the tetanus vaccine
Keywords: Immunization schedule, vaccination and risk factors. (Source: MESH – NLM)
RESUMEN
Objetivo: Determinar los factores de riesgo prenatales asociados al incumplimiento del esquema básico de vacunación en menores de 5 años a partir de la encuesta demográfica y de salud familiar (ENDES) del año 2018. Materiales y Métodos: Es un estudio observacional, retrospectivo, analítico y transversal. Se estudia la muestra de la Encuesta Nacional Demográfica y de Salud (ENDES) del año 2018 que comprende a 18 104 niños entre 1 a 5 años con tarjeta de salud vista en la entrevista, encontrándose los resultados en las encuestas del INEI. Se selecciona los archivos que contienen los cuestionarios del esquema de vacunación y se procesan los datos con SPSS versión 25. El procesamiento estadístico es de tipo analítico y descriptivo, bivariado y multivariado con ayuda de STATA v16 y Excel 2016. Resultados: Se contó con una muestra final de 18 104 de menores entre 1 a 5 años el 2018. En el análisis multivariado se encontró la asociación del incumplimiento de esquema de vacunación con la edad de la madre (valor p= <0,01, RP= 1,20, IC= 1,13 – 1,28), el número de controles no adecuados (valor p= <0,01, RP= 1,28, IC= 1,23 – 1,33) y la gestante no haber recibido la vacuna antitetánica en el embarazo (valor p= <0,01, RP= 1,16, IC= 1,12 – 1,20). No se encontró dicha asociación con el lugar de residencia, índice de riqueza y región natural. Conclusiones: Los factores de riesgo prenatales asociados al incumplimiento del esquema básico de vacunación en menores de 5 años fueron la edad materna, el número de controles prenatales inadecuados y la gestante no haber recibido la vacuna antitetánica.
Palabras Claves: Esquema de inmunización, vacunación y factores de riesgo (Fuente: Decs - BIREME).
Vaccines are biological results that encompass one or multiple antigens that are supplied with the purpose of performing a respective immune stimulus, which seeks to mimic the natural infection, developing immune replication with the purpose of safeguarding it in the following presentations to the respective microorganism.(1) They constitute one of the most efficient public health interventions in terms of cost reduction and morbimortality of preventable infectious and contagious diseases.(2) Systematic vaccination programs have led to the disappearance of smallpox, reduction of the spread of poliomyelitis in practically the whole world and the surveillance of diseases such as measles, tetanus, diphtheria, rubella or massive Haemophilus influenzae disease.(1)
The World Health Organization indicates that organized vaccination covers four out of five children where all three doses of diphtheria, tetanus and pertussis vaccine (DTP3) have been administered, in order to safeguard them against dangerous infectious diseases that can lead to severe disorders and disabilities up to mortality.(3)
A nivel mundial según la OMS, la cobertura de inmunización sigue siendo desde 2010 alrededor del 86%. Se necesita una cobertura del 95% a escala mundial que abarque a los países y las comunidades para garantizar la protección contra los brotes de enfermedades que pueden prevenirse con vacunas.(4)
Globally according to WHO, immunization coverage remains around 86% since 2010. A 95% coverage is needed globally covering countries and communities to ensure protection against vaccine-preventable disease outbreaks.(4)
In Peru, there is a national vaccination scheme which has a succession of the organization and the way vaccines are provided formally accepted by the Ministry of Health with the purpose of cooperating to increase the quality of health of the inhabitants by controlling preventable immune diseases being seventeen vaccines incorporated in the national scheme up to the year of age.(4) There are vaccination indicators that allow monitoring the access, follow-up, results and impact of "The National Sanitary Strategy of immunizations" where the percentages that measure the performance and coverage for the fulfillment of the complete vaccination in a child are calculated.(4)
In Peru, vaccination percentages are obtained through the Demographic and Family Health Survey (ENDES).(4) Therefore, it is of vital importance to determine the main risk factors in our environment that generate non-compliance with the basic vaccination schedule and thus detect them in order to generate recommendations for adequate compliance and expand national coverage.(5)
METHODOLOGY
Design and study area: The present is an Observational, retrospective analytical and cross-sectional study of a secondary analysis of data from the National Demographic and Health Survey (ENDES) of 2018.
Population: It is constituted by minors aged one to five years old in Peru in the year, registered according to the 2018 Demographic and Family Health Survey database.
Sample: The type of sample is Bi-stage self-weighted, in the first stage the Primary Sampling Unit is selected by clusters and the second stage the Secondary Sampling Unit is selected to dwellings resulting in 18 104 participants. The statistical and cartographic information from the National Population Census XI and Housing Census VI of 2007 and the SISFOH Update 2012-2013, and the cartographic material updated for this purpose in the cartographic updating process carried out for the execution of the DHS. The databases are available in the "Microdata" section of the website of the Instituto Nacional de Estadística e Informática del Perú (http://inei.inei.gob.pe/microdatos/).(4) The following sample selection criteria were used:
Inclusion criteria:
-
• Children older than one year (12 months) of age registered in the DHS 2018 data center.
• Minors whose mothers or caregivers had presented vaccination health card or given report to the interviewer.
• Children whose mothers have provided information concerning the study variables.
-
• Mothers or children with missing or incomplete data concerning the study variables.
Among the study variables, non-compliance with the vaccination schedule was taken as a dependent variable and place of residence, age, wealth index, maximum level of education, prenatal controls and tetanus vaccination as independent variables.
As techniques and instruments for data collection:
The questionnaire implemented in a mobile device: Tablet was used as an instrument, and as a technique the survey conducted in the homes selected to fill out the questionnaire. The variable description section was subsequently visualized and the data files were selected (http://webinei.inei.gob.pe/anda_inei/index.php/catalog/306/vargrp/VG26).(4)
The dependent variable in:
REC43: This file contains information on Immunization and morbidity: Immunizations received by the infant.
REC95: This file contains information on variables on the topic of health and immunization.
The independent variable: REC0111: This file contains information on basic data on women aged 15-49 years.
REC41: This file contains information on pre-natal and delivery care.
RECH0: This file contains information on household characteristics such as.
REC91: This file contains information on domestic violence, as well as on Sexually Transmitted Infections during pregnancy.
Once the variable of interest for the present investigation had been identified, a data file was formed with all of them, taking into account the identifiers according to the DHS (CASEID, HHID). After this, the missing data were eliminated, leaving a sample of 18,104 children between 1 and 5 years of age.
Data processing and analysis plan
For the ordering, processing, tabulation and analysis of the results, the SPSS version 25 statistical software was used and the tables were captured in Excel 2016. To obtain the results, the SPSS complex samples module was used, for which the weighting variable V005, the conglomeration variable V001 and the stratification variable V022 were identified; the CSPLAN file was generated with them, maintaining the DHSES sample design. Subsequently, STATA V16 software was used to calculate the prevalence ratios for both the crude and adjusted prevalence ratios using the Poisson regression model with robust variance.
For the univariate analysis, frequencies and percentages were calculated. Then, in the analytical phase, those variables with more than 2 categories were categorized in order to calculate the crude prevalence ratios (PR). Subsequently, adjusted prevalence ratios were calculated in order to identify the factors associated with noncompliance with the basic vaccination schedule.
The response variable was Non-compliance with the Basic Vaccination Schedule, which was calculated based on the recoding of the variables "BCG 1, HVB , PENTAVALENT 1, ANTIPOLIO 1, ROTAVIRUS 1, PNEUMOCOCOCO1, PENTAVALENT 2, ANTIPOLIO 2, ROTAVIRUS 2, PNEUMOCOCOCO 2, PENTAVALENT 3, ANTIPOLIO 3, MMR 1, PNEUMOCOCOCO 3 and INFLUENZA 1".
It should be noted that the varicella vaccine was not included in the ENDES records, so it could not be taken.(27)
Ethical aspects
In the database used are of public access through the web page of the National Institute of Statistics and Census, that institution has classified each occurrence of the study with tools to safeguard the identity of each participating individual, where without diminishing its statistical benefit, it is difficult to infer what could be the profile of a precise person. The study was approved by the Institute of Research in Biomedical Sciences of the Ricardo Palma University and the registration and approval of the Faculty of Human Medicine.
Limitations of the study
The present study is limited to prenatal risk factors that influence non-compliance with the vaccination schedule, but does not take into account other factors such as biological factors, postnatal factors, underlying diseases of the mother and child.
RESULTS
Of the 18,104 children, it was found that 10,044 children did not comply with the basic vaccination schedule, 55.5% of the total. (Figure 1)
Figura 1. Children over 12 months older according to compliance with the vaccination scheme - BCG 1, HVB, Penta 1, Polio 1, Rota 1, Neumo 1, Penta 2, Polio 2, Rota 2, Neumo 2, Penta 3, Polio 3, SPR1, Neumo 3 e Influenza.
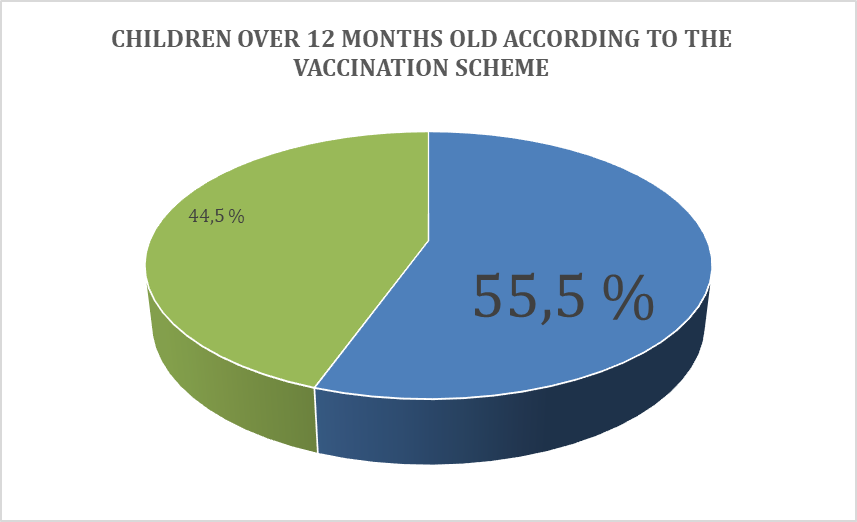
Source: ENDES 2018
In the same work with the total sample of 18 104 another analysis was performed taking to the vaccination scheme to 7 main vaccines according to previous studies; BCG, DPT1, POLIO 1, DPT2, POLIO 2, DPT3 AND POLIO 3 where it was found that 3 863 minors failed to comply with the vaccination scheme being 21.3% of the total.
Regarding the general characteristics of the mothers in this sample, it was observed that 70% belonged to urban areas and 30% to rural areas, 4.3% were between 12 and 19 years old, 65.5% were between 20 and 34 years old and 30.2% were between 35 and 49 years old. In the highest level of education 1.6% had no education at all, 20.1% had primary education, 44.7% had secondary education and 33.6% had higher education. In the level of wealth 28.4% were very poor, 26.2% poor, 19.6% medium, 14.8% rich and 10.9% very rich. According to natural region 12.4% lived in metropolitan Lima, 29.6% in the rest of the coast, 34% in the highlands and 24% in the jungle. According to prenatal checkups 89.3% had more than 6 NPC and 10.7% between 1 and 5 NPC and according to the application of tetanus vaccine 76.7% received and 23.3% did not receive it. (Table 1)
Table 1. General characteristics of mothers with children older than 1 year according to ENDES 2018.
|
General characteristics |
N |
% |
|
Place of residence |
|
|
|
Urban |
12669 |
70% |
|
Rural |
5435 |
30% |
|
Age |
|
|
|
From 12 - 19 |
777 |
4,3% |
|
20-34 |
11865 |
65,5% |
|
35-49 |
5462 |
30,2% |
|
Maximum level of education |
|
|
|
Uneducated |
292 |
1,6% |
|
Primary |
3634 |
20,1% |
|
Secondary |
8098 |
44,7% |
|
Higher |
6080 |
33,6% |
|
Wealth index |
|
|
|
Very poor |
5145 |
28,4% |
|
Poor |
4749 |
26,2% |
|
Middle |
3557 |
19,6% |
|
Wealthy |
2673 |
14,8% |
|
Very wealthy |
1980 |
10,9% |
|
Natural Region |
|
|
|
Metropolitan Lima |
2247 |
12,4% |
|
Rest Costa |
5353 |
29,6% |
|
Mountain range |
6157 |
34,0% |
|
Jungle |
4347 |
24,0% |
|
Prenatal check-ups |
|
|
|
From 6 to more PCU |
16171 |
89,3% |
|
From 1 to 5 PCU |
1933 |
10,7% |
|
Tetanus vaccine in pregnancy |
|
|
|
Received |
13890 |
76.7% |
|
Not received |
4214 |
23,3% |
Regarding the risk factors according to non-compliance with vaccination, the p-value of area of residence 0.004, age 0.000, maximum level of education 0.345, wealth index 0.000, natural region 0.000, prenatal controls 0.000 and tetanus vaccination in pregnancy 0.000 were found. (Table 2).
Table 2. Risk factors for mothers with children under 5 years of age according to whether they comply with the vaccination scheme.
|
Factors |
Vaccination scheme |
Tight F |
p value |
|||
|
Breached |
Met |
|||||
|
n |
% |
n |
% |
|||
|
Place of residence |
||||||
|
Rural |
2507 |
24.8% |
2507 |
27.3% |
8,358 |
0,004 |
|
Urban |
7116 |
75.2% |
5553 |
72.7% |
||
|
Age |
||||||
|
From 12 - 19 |
532 |
4.9% |
245 |
2.9% |
16,517 |
0,000 |
|
35-49 |
2892 |
29.9% |
2570 |
32.0% |
||
|
20-34 |
6620 |
65.2% |
5245 |
65.1% |
||
|
Maximum level of education |
||||||
|
Uneducated/p> |
166 |
1.5% |
126 |
1.4% |
1,104 |
0,345 |
|
Primary |
1988 |
18.5% |
1646 |
19.1% |
||
|
Secondary |
4520 |
43.6% |
3578 |
44.5% |
||
|
Higher |
3370 |
36.4% |
2710 |
35.0% |
||
|
Wealth index |
||||||
|
Very poor |
2849 |
24.2% |
2296 |
24.7% |
7,095 |
0,000 |
|
Poor |
2591 |
22.9% |
2158 |
24.5% |
||
|
Middle |
1979 |
19.7% |
1578 |
20.4% |
||
|
Wealthy |
1459 |
16.6% |
1214 |
17.7% |
||
|
Very wealthy |
1166 |
16.6% |
814 |
12.7% |
||
|
Natural Region |
||||||
|
Metropolitan Lima |
1385 |
30.0% |
862 |
23.8% |
19,239 |
0,000 |
|
Rest Costa |
3031 |
26.7% |
2322 |
27.0% |
||
|
Mountain range |
3159 |
26.1% |
2998 |
31.5% |
||
|
Jungle |
2469 |
17.2% |
1878 |
17.6% |
||
|
Prenatal check-ups |
||||||
|
From 6 to more PCU |
1366 |
12.5% |
567 |
6.7% |
118,014 |
0,000 |
|
From 1 to 5 PCU |
8678 |
87.5% |
7493 |
93.3% |
||
|
Tetanus vaccine in pregnancy |
||||||
|
Not received |
2602 |
26.6% |
1612 |
19.0% |
101,163 |
0,000 |
|
Received |
7442 |
73.4% |
6448 |
81.0% |
||
The bivariate analysis
Hows that among the factors analyzed, women aged 12 to 19 years have a 1.21 times (CI 1.13 - 1.28) prevalence ratio of non-compliance with the vaccination schedule compared to women aged 20 to 34 years; according to prenatal controls, pregnant women who only had at most 5 NPC have a 1.29 times (CI 1.22 - 1.32) prevalence ratio of non-compliance with the vaccination schedule compared to pregnant women with more than 6 NPC, 22- 1.32) prevalence ratio of non-compliance with the vaccination schedule compared to pregnant women with more than 6 NPCs, if the pregnant woman did not receive the tetanus vaccine, she has 1.16 times (CI 1.13 - 1.20) prevalence ratio of non-compliance with the vaccination schedule compared to those who did receive the tetanus vaccine and the natural region (PR: 0.89 IC 0.84 - 0.94). For place of residence (PR: 1.05 CI 0.99 - 1.11), level of education (PR: 1.08 CI 0.96 - 1.22) and wealth index (PR: 1.00 CI 0.93 - 1.09) no significant association was found. (Table 3)
Table 3. Crude and adjusted reasons for prevalence (PR) among the factors with non-compliance with the vaccination schedule in children under 5 years according to the ENDES 2018.
|
Factors |
Raw RP |
IC95% |
Tight RP |
IC95% |
|
Place of residence |
||||
|
Rural / Urban * |
1.06 |
1,02 - 1,11 |
1.05 |
0,99 - 1,11 |
|
Age |
||||
|
12-19 / 20 -34 * |
1.21 |
1,14 - 1,29 |
1.20 |
1,13 - 1,28 |
|
35-49 / 20 -34 * |
0.97 |
0,94 - 1,00 |
0.96 |
0,92 - 0,99 |
|
Maximum level of education |
||||
|
Uneducated / Higher* |
1.02 |
0,91 - 1,15 |
1.08 |
0,96 - 1,22 |
|
Primary / Higher* |
0.97 |
0,92 - 1,02 |
1.00 |
0,95 - 1,07 |
|
Secondary / Higher* |
0.97 |
0,94 - 1,01 |
0.98 |
0,94 - 1,02 |
|
Wealth index |
||||
|
Very poor / Very wealthy * |
0.89 |
0,84 - 0,95 |
1.00 |
0,93 - 1,09 |
|
Poor / Very wealthy * |
0.87 |
0,82 - 0,93 |
0.94 |
0,88 - 1,00 |
|
Middle / Very wealthy * |
0.89 |
0,83 - 0,94 |
0.93 |
0,87 - 0,99 |
|
Wealthy / Very wealthy * |
0.88 |
0,82 - 0,93 |
0.90 |
0,85 - 0,96 |
|
Natural Region |
||||
|
Jungle/ Metropolitan Lima * |
0.90 |
0,85 - 0,95 |
0.89 |
0,84 - 0,94 |
|
Mountain range / Metropolitan Lima * |
0.84 |
0,80 - 0,88 |
0.82 |
0,77 - 0,86 |
|
Rest Costa/ Metropolitan Lima * |
0.91 |
0,86 - 0,95 |
0.91 |
0,87 - 0,96 |
|
Prenatal check-ups |
||||
|
From 1 to 5 PCU / From 6 to more PCU * |
1.29 |
1,24 - 1,34 |
1.27 |
1,22 - 1,32 |
|
Tetanus vaccine in pregnancy |
|
|
||
|
Not received / Received * |
1.19 |
1,15 - 1,23 |
1.16 |
1,13 - 1,20 |
Fuente: ENDES 2018/Authors own creation
The multivariate analysis
It is observed that there is statistical significance according to the prenatal controls that only had at most 5 NPC present 1.28 times (CI 1.23 - 1.33) prevalence ratio of non-compliance with the vaccination schedule compared to pregnant women who had more than 6 NPC and if the pregnant woman did not receive the tetanus vaccine presents 1.16 times (CI 1.12 - 1.20) prevalence ratio of non-compliance with the vaccination schedule compared to those who received the tetanus vaccine. (Table 4)
Table 4. Multivariate analysis of factors with noncompliance with the vaccination scheme in children under 5 years of age according to ENDES 2018.
|
Factors |
Tight RP |
CI95% |
|
Age |
||
|
12-19 / 20 -34 * |
1.21 |
1,14 - 1,29 |
|
35-49 / 20 -34 * |
0.97 |
0,94 - 1,00 |
|
Prenatal check-ups |
||
|
From 1 to 5 PCU / From 6 to more PCU * |
1.28 |
1,23 - 1,33 |
|
Tetanus vaccine in pregnancy |
|
|
|
Not received / Received * |
1.16 |
1,12 - 1,20 |
Source: ENDES 2018/Authors' own creation
DISCUSSION
Non-compliance with the vaccination schedule goes hand in hand with the health of the child, which is why it is a global public health strategy since it prevents mortality in children; according to the WHO(3), compliance with the vaccination schedule is 90% worldwide.
Vaccination non-compliance rates vary according to the income of the countries, with middle and low income countries having a high rate on average and higher income countries having a lower rate. The rate in China, according to Cao et al(6), reports 6.9% non-compliance in younger children. On the other hand, in Mexico, a country with similar sociocultural and demographic characteristics to our country, Palacios(7) estimated the rate of noncompliance with the vaccination schedule in younger children at 35%.
In our study, 55.5% of children between 1 and 5 years of age did not comply with the vaccination schedule, a rate above that of middle and high income countries and far from the WHO world recommendations. Similarly, in the Peruvian population, Achuquín(8) in 2017, found 22% non-compliance with the scheme, so we deduce that the percentage found in our study would not be in the expected range since the previous study did not take into account the complete scheme but only 7 main vaccines and in an analysis where the same vaccines were taken, it was found that 21.3% of children aged 1 to 5 years did not comply with the vaccination scheme in 2018 according to ENDES, which would be in the expected range according to INEI.(9)
Maternal age is related as risk behavior and with greater difficulty in making decisions, probably due to hormonal changes and this development is not synchronous between the prefrontal area with respect to those related to socioemotional processes(8). Sheikh et al(10) in Bangladesh, found that a maternal age younger than 20 years was related to noncompliance (OR= 3.21, p < 0.05, CI= 1.02- 10.13). Likewise Ali(11) in 2017 showed an association between mothers between 19 to 26 and noncompliance with the scheme (OR = 9.59) and Cabrejos(12) in 2017 in his study conducted in Peru, found maternal age as a factor associated with noncompliance with the scheme. Similarly, in our study it was found that maternal age between 12 and 19 years was associated 1.20 times higher than between 20 and 34 years of age of the mothers, increasing the risk of noncompliance with the vaccination schedule. Thus, maternal age was found to be a factor associated with noncompliance with the vaccination schedule.
Adequate prenatal follow-up is associated with a lower number of obstetric complications and with making the mother aware of the care and pertinent behaviors to follow during pregnancy, the main ones being compliance with immunizations and prenatal controls.(8,13) In Peru, according to MINSA, prenatal controls must be at least 6 CPN to be considered adequate follow-up and to guarantee the wellbeing of the baby, if there are fewer or no prenatal controls, this can generate a high risk for the mother and the baby, which often affects development(8). In the study, non-compliance with the vaccination schedule was found to be 1.28 times higher in pregnant women with less than 6 prenatal checkups than in pregnant women with 6 or more prenatal checkups. Likewise, Ali(11) in 2017 found an association between fewer prenatal checkups and noncompliance with the vaccination schedule (OR = 9.59), Nozaki(13) found that having more than 4 checkups was associated with compliance with the vaccination schedule (OR: 1.87, 95% CI: 1.28- 2.73) and Achuquín(8) in 2017 in Peru (OR= 2.19, p=<0.01, CI= 1.79- 2.51) found that prenatal checkups are a factor associated with noncompliance with the vaccination schedule.
The application of the tetanus vaccine during pregnancy serves to guarantee the wellbeing of the baby during gestation, since if it is not applied it can generate risk for the baby, which often affects its development.(8,13) The study found that not applying the tetanus vaccine was associated 1.28 times more than in children of mothers with tetanus vaccine application, increasing the risk of non-compliance with the vaccination schedule. Similarly Ali(11) in 2017 found an association between tetanus vaccination and compliance with the vaccination schedule (OR = 9.59). A similar finding was that of Nozaki(13) found an association between the application of tetanus vaccine during gestation and compliance with the vaccination schedule (OR: 1.87, 95% CI: 1.28- 2.73) and Achuquín(8) in 2017 in Peru obtained that not having received the tetanus vaccine (OR= 2.19, p=<0.01, CI= 1.79- 2.51). The application of vaccines in pregnant women generates awareness and adherence to the vaccination schedule in their children; therefore, not applying the vaccine is a risk factor.
The area of residence, in rural areas is related to the poor accessibility of vaccines associated with non-compliance with the vaccination schedule(15). As well as 2017 in Colombia, Salas(14) obtained 26% in rural areas and Achuquín(8) in Peru found 23.6% in rural areas (p <0.01, OR= 0.97, CI= 0.84 - 1.12) related to non-compliance with the vaccination scheme in minors. On the other hand, Garcia(15) in Apurimac-Peru in 2015 obtained 36.7% of children in rural areas did not comply with the vaccination schedule. In our study, it was found that 24% of children under 5 years of age did not comply with the vaccination schedule and live in rural areas; statistical significance was not found in accordance with the background.
According to the maximum level of education of the mother, incomplete or deficient training can lead to poor knowledge in basic health issues and assimilation of misconceptions causing poor judgment in mothers or caregivers which can generate non-compliance with immunizations for example, adverse reactions can generate lethality, vaccines are not necessary for the development of a child and vaccine myths(8,16). Forshaw et al. in 2017 found that 35% of mothers with primary education did not comply with the vaccination schedule for their children. Similarly, Salas(14) in Colombia in 2016 found that 40% of mothers with primary education at the highest level did not comply with the vaccination schedule. On the other hand, in Peru in 2017, Aguilar et al(17) obtained 50.1% of mothers with primary education did not comply with the vaccination schedule in their children and Achuquín(8) in the same year obtained 28.2% of mothers with primary or no academic degree did not comply with the vaccination schedule (p= 0.24, OR=1.07, CI 0.95 - 1.21). In our study, 18.5% of mothers with primary education did not comply with the vaccination schedule in their children, in which no statistical association was found according to our antecedents, perhaps due to the association of the variables and the sample.
The wealth index could have an association because, although vaccines are free, the condition of poverty means that mothers are often unable to take their children to the health center because they do not have the economic means such as transportation and food, among others(8). Morton(11) in Australia in 2018 found that 26% of children in extreme poverty did not comply with the vaccination schedule and Sheikh et al(10) in Bangladesh identified extreme poverty as a risk factor associated with non-compliance with vaccination with an OR= 2.2. Likewise, Achuquín(8) in Peru found 28.2% poverty (OR= 1.10, p= <0.01, CI= 1.07- 1.26) found socioeconomic status as a factor associated with noncompliance (gamma= 0.553, sig (Bilateral)= 0.003 and p= 0.01). In our study we found that 24.4% of children in the very poor quintile did not comply with the vaccination schedule, but without statistical association, in contrast to our antecedents, because the antecedents that did show an association were in other countries or with samples of minors.
According to the natural region considering the accessibility of vaccines, being better in lima because in provinces there is difficulty in transporting and complying with the entire cold chain in vaccines(16). According to Achuquín(8) in 2017, there was no association between the natural region and non-compliance with vaccination.
As in our study, it was found that 26.1% of underage children did not comply with the vaccination schedule in the highlands. In both studies, no statistical association was found, which could be due to the sample and size.
CONCLUSIONS
-
• Through our work, it was obtained that the variable young age of the mother, prenatal controls less than 6 and the non-application of tetanus vaccine in the pregnant woman is associated as a risk factor for noncompliance with the vaccination schedule in children under 5 years of age in 2018.
• No significant association was found between noncompliance with the vaccination schedule in children under 5 years of age with the place of residence, educational level of the mother, wealth index and natural region possibly due to the population used, as this generates many biases and limits the study.
Authorship contributions: The author participated in the generation, writing and final approval of the original article, as well as in data collection.
Financing: Self-funded.
Conflict of interest: The author declares that she has no conflict of interest in the publication of this article.
Acknowledgment: We thank Dr. Jhony De la Cruz Vargas for his collaboration with the development of this article.
Received: January 03, 2021
Approved: February 08, 2021.
Correspondencia: Isidro Rios Trinidad Liberata.
Teléfono: 975508857
Correo: libe.isidro.14@gmail.com
BIBLIOGRAPHIC REFERENCES
