ARTICULO ORIGINAL
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2021 - Universidad Ricardo Palma10.25176/RFMH.v21i2.3708
PLATELET / SPLEEN RATIO FOR THE DIAGNOSIS OF ESOPHAGEAL VARICES AND THE RISK OF BLEEDING IN PATIENTS WITH LIVER FAILURE
COCIENTE PLAQUETAS/BAZO PARA EL DIAGNÓSTICO DE VÁRICES ESOFÁGICAS Y RIESGO DE SANGRADO EN PACIENTES CON INSUFICIENCIA HEPÁTICA
Álvaro José Montiel Jarquín1,d, Arturo García Galicia1,a, Andrés Gámez Herrera2,b, Emma Ixchel González Bravo1,c, Ricardo Adolfo Parker Bosquez3,b, José Alfredo León Zamudio4,e, José Álvaro Parra Salazar1,f, María del Socorro Romero Figueroa5,g
1 Unidad Médica de Alta Especialidad Hospital de Especialidades, Centro Médico Nacional “Gral. de
Div. Manuel Ávila Camacho”, Instituto Mexicano del Seguro Social, Puebla-Puebla México.
2 Unidad de Medicina Familiar n°8, Delegación Puebla, Instituto Mexicano del Seguro Social.
Puebla, Puebla-México.
3 Hospital General de Zona número 20, Delegación Puebla, Instituto Mexicano del Seguro Social,
Puebla-Puebla, México.
4 Hospital General de Zona n° 1, Tepic, Nayarit-México.
5 Escuela de Medicina, Universidad Anáhuac Campus Norte, Estado de México-México.
a Médico Especialista en Pediatría, Maestro en Ciencias Médicas e Investigación.
b Médico Especialista en Medicina de Urgencias.
c Médico Especialista en Gastroenterología.
d Médico Especialista en Cirugía General, Maestro en Ciencias Médicas e Investigación.
e Médico General.
f Médico Cirujano Cardiotórácico.
g Médica Especialista en Anestesiología, Doctora en Investigación en Medicina.
ABSTRACT
Upper gastrointestinal bleeding of variceal origin has a high mortality. The sensitivity and specificity
of the ratio number of platelets / largest diameter of the spleen was determined for the diagnosis of
esophageal varices with risk of bleeding in patients with liver failure; A process study, carried out in
a second level medical care hospital, was performed ultrasound, hematic cytometry, liver function tests
and endoscopy.
There were 70 patients with liver failure, 28 women (20 with hepatitis C virus) and 42 men (31 with
alcoholism).
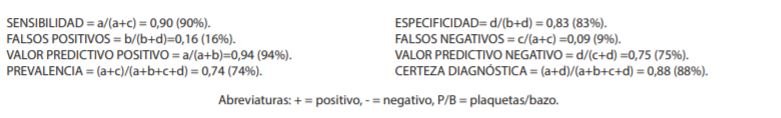
The spleen / platelet ratio has a sensitivity of 90%, specificity 83%, false positives 16%, false
negatives 9%, positive predictive value 94%, negative predictive value 75%, prevalence of 74% and
diagnostic certainty of 88% to diagnose esophageal varices with risk of bleeding.
The platelet / spleen ratio is useful and non-invasive to diagnose esophageal varices with risk of
bleeding, in hospitals where endoscopy is not available.
Key words: Esophageal and Gastric Varices, Gastrointestinal Hemorrhage, Hepatic failure, Hepatic Insufficiency, Diagnosis. (source: MeSH NLM).
RESUMEN
El sangrado de tubo digestivo alto de origen variceal tiene una mortalidad alta. Se determinó la
sensibilidad y especificidad del cociente número de plaquetas/diámetro mayor del bazo para diagnóstico
de várices esofágicas con riesgo de sangrado en pacientes con insuficiencia hepática; estudio de
proceso, realizado en un hospital de segundo nivel de atención médica, se realizó ultrasonido,
citometría hemática, pruebas de función hepática y endoscopia.
Fueron 70 pacientes con insuficiencia hepática, 28 mujeres (20 con virus de hepatitis C) y 42 hombres
(31 con etilismo).
El cociente bazo/plaquetas tiene una sensibilidad de 90%, especificidad 83%, falsos positivos 16%,
falsos negativos 9%, valor predictivo positivo 94%, valor predictivo negativo 75 %, prevalencia del 74%
y certeza diagnóstica del 88% para diagnosticar várices esofágicas con riesgo de sangrado.
El cociente plaquetas/bazo es útil y no invasivo para diagnosticar várices esofágicas con riesgo de
sangrado, en hospitales donde no se cuenta con endoscopía.
Palabras clave: Várices esofágicas y gástricas; Hemorragia gastrointestinal; Fallo hepático; Insuficiencia hepática, Diagnóstico. (fuente: DeCS BIREME).
INTRODUCTION
Portal hypertension is the increase of portosystemic pressure in any segment of the portal
venous system, caused by pre-hepatic or post-hepatic alterations or by other causes (1). It occurs when the portocaval gradient is higher than 5 mmHg and is the
most frequent and studied cause of hepatic cirrhosis. From 5 to 33% of these patients have varices,
which may appear at any part of the gastrointestinal tract, the most frequent site being the distal
centimeters of the esophagus. The presence of varices is correlated with the severity of liver disease
(1,2). The hepatic venous pressure gradient is the ratio
between portal pressure and vena cava pressure and predicts the appearance of varices. Clinically
significant portal hypertension is 10 mmHg, and is a prognosis factor in patients suffering from portal
hypertension (1).
When the gradient reaches 12 mmHg, variceal hemorrhage occurs. The main risk factors are:
international normalized ratio (INR) greater than 1.5, portal vein diameter greater than 13 mm, and
thrombocytopenia. When the patient has one or more of these conditions, it is necessary to perform upper
gastrointestinal endoscopy to look for varices and to perform primary prophylaxis against bleeding in
cirrhotic patients (1-3).
In upper gastrointestinal bleeding (UGH), endoscopy has a high sensitivity and specificity in
locating and identifying lesions that cause bleeding. In addition, it offers the possibility of a
therapeutic approach and primary prophylactic treatment (2,4,5).
Certain noninvasive tests are useful in detecting patients at risk of esophageal varices. These
include platelet count, splenomegaly, portal vein diameter greater than 13 mm by abdominal ultrasound
and lately elastography. However, none of these tests has diagnostic accuracy for large esophageal
varices (1,6,7).
The platelet count/spleen bipolar diameter (P/B) ratio of less than 909 is a non-invasive
parameter that predicts the presence of esophageal varices in cirrhotic patients (8). It can be a diagnostic and follow-up alternative to endoscopy, which is
expensive and difficult to access, and may be contraindicated in some patients (8,9).
The objective was to determine the sensitivity and specificity of the platelet count/spleen
major diameter (P/B) ratio for the diagnosis of esophageal varices with risk of bleeding in patients
with liver failure.
THE STUDY
A cross-sectional study was carried out in which a test of a test was performed in a secondary-level
hospital of Instituto Mexicano del Seguro Social (IMSS) (IMSS) in Puebla, Mexico. Patients with liver
failure of any degree of severity, of both sexes, over 18 years of age and who agreed to participate in
the study by filling out and signing an informed consent form were included; patients with acute liver
failure and those who died during the study were excluded.
Liver failure was defined by the presence of an INR >1.5, increased aminotransferases, anemia,
leukopenia, hypoalbuminemia, and liver disease manifested by anorexia, weight loss, weakness, fatigue,
osteoporosis, ascites, jaundice, asterixis, hepatic stench, gynecomastia, hepatomegaly, palmar erythema,
testicular atrophy, gynecoid hair, and encephalopathy (13-15).
Acute liver failure was considered when the duration of the disease was less than 26 weeks of
evolution and without previously known liver disease (10,11).
Patients were recruited from the gastroenterology department and evaluated for severity
according to the Child-Pugh classification (12).
Platelet/spleen indices lower than or equal to 909 were found to be normal (1,6).
Hematic cytometry, liver function tests (in those older than one month from the previous
control), upper gastrointestinal endoscopy with Fujinon endoscope model Eve EG 450WR5 and splenic
ultrasound with Siemens Acuson X300 ultrasound were performed to determine the largest diameter of the
spleen. For the statistical analysis, 2 x 2 tables were used for sensitivity, specificity, predictive
values and test efficacy. Correlation of severity scales was performed with Spearman's rank correlation
coefficient and a value of p≤0.05 was considered statistically significant. The study was approved by
the Comité Local de Investigación y Ética en Investigación en Salud 2102 with registration number:
R-2016-2102-12, and the anonymity of the participating patients was preserved at all times.
FINDINGS
Seventy patients were recruited. The sample was predominantly male and geriatric patients. The
characteristics in terms of sex, age and etiology of liver disease are shown in Table
1.
The average age was 59.58, minimum 35, maximum 85, SD=10.92 years. Regarding age groups, 3
(4.3%) patients were in the 18 to 40 years old group, 28 (40%) in the 41 to 60 years old group and 39
(55.7%) patients in the group older than or equal to 61 years old.
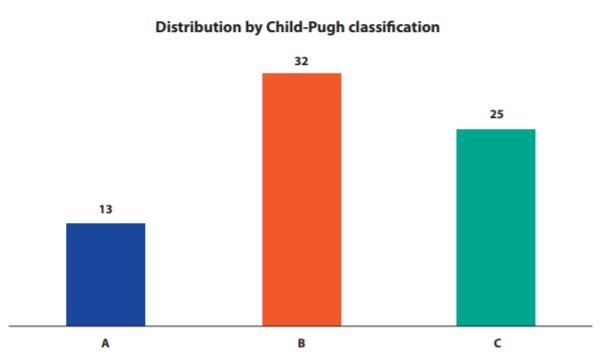
Regarding Child-Pugh classification, stage B was the most frequent with 32 (45.7%) patients.
Details are shown in Figure 1.
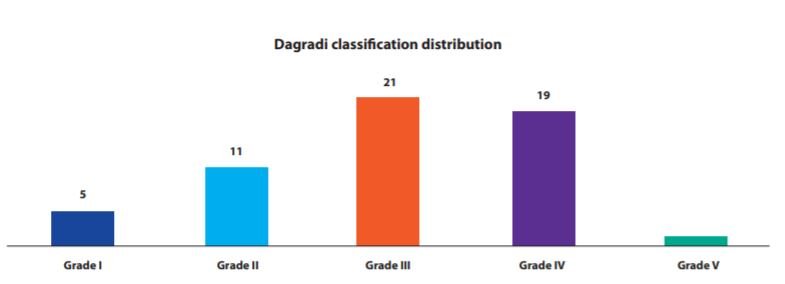
According to the Dagradi classification for esophageal varices (3),
there were 21 (30%) Grade III patients. The rest of the details can be seen in Figure 2.
The correlation between P/B and Child-Pugh was 0.723, p<0.05, and between P/B and Dagradi was
0.585 (p<0.05), (a value of p<0.05 Spearman was considered statistically significant).
Of the 70 patients included in the sample, 47 (67%) patients presented esophageal varices at
endoscopy and positive P/B index, 5 (7%) presented positive endoscopy for esophageal varices and 1.4% of
patients presented negative P/B, with the following results: sensitivity 90%, specificity 83%, false
positives 16%, false negatives 9%, positive predictive value of 94%, a negative predictive value of 75%,
prevalence of 74% and a diagnostic certainty of 88% for P/B as a predictor of esophageal varices with
risk of bleeding (Table 2).
Table 1. Population characteristics.
| Sex Etiology | Men | Women |
|---|---|---|
|
Virus hepatitis C |
0 |
20 |
|
Virus hepatitis B |
0 |
1 |
|
Etilism |
31 |
0 |
|
Unidentified |
11 |
7 |
|
Total |
42 |
28 |
|
Total of patients=70 |
Table 2. Comparison of the P/B index with endoscopy results.
| Endoscopic result | TOTAL | |||
|---|---|---|---|---|
|
+ |
- |
|||
|
Índice P/B <909 |
+ |
47 |
3 |
50 |
|
- |
5 |
15 |
20 |
|
|
TOTAL |
52 |
18 |
70 |
|
DISCUSSION
Portal hypertension is the main complication of chronic liver diseases that develop cirrhosis.
It can cause esophageal varices in up to 30% of patients (1,6-9,12). The most frequent causes are viral,
alcoholic and of unidentified cause (1).
Endoscopy is the diagnostic method of choice in HDA, it has high sensitivity and specificity
since it records and identifies the location of the lesions that cause bleeding in the esophagus,
stomach and duodenum. Nowadays, it is still the most accurate technique for diagnosing and staging
esophageal varices, especially those of grade I, and for visualizing signs of risk for hemorrhage. This
method provides the diagnosis and offers the possibility of a therapeutic approach (4,5,13).
The frequency of bleeding esophageal varices is 100 in every 100,000 persons per year; it is a
medical emergency associated with high mortality, especially in older adults (1-3,5-9).
Esophageal varices, which occur in 100 out of every 100,000 persons per year, are a medical
emergency associated with high mortality, especially in older adults (1-3,5-9,13,14).
However, since endoscopy is an invasive diagnostic method, it has both relative and absolute
contraindications. In developing countries, the availability of an endoscopic study is limited,
therefore, different less invasive methods such as the P/B index have been implemented (4,6-9,13,14).
The P/B index is inexpensive, is run quickly and requires no major skills for its performance.
It is seen as a safe alternative in countries with limited economic resources that do not have endoscopy
services, and another advantage is that it can be calculated rapidly (6,8,13-15).
Since 2003, the high value of P/B has been demonstrated, even in the subgroup of patients with
compensated liver disease (6).
The value of P/B 909 or lower has been considered an indicator of esophageal varices (6,8,14,15). Reports in the
Latin American population range from acceptable to very good for sensitivity, specificity and positive
and negative predictive values (8,14,15). In
this study the results of the test in comparison with endoscopy were very high in sensitivity (90%),
specificity (83%) and positive predictive value (94%), but low in negative predictive value (75%).
Some studies carried out in the Mexican population report a moderate correlation between P/B and
esophageal varices: a P/B value greater than 0.7 correlated with Baveno grade I varices (<5 mm), and
less than 0.7 with grade II varices (>5 mm) and with a low predominance in the advanced stages of
Child-Pugh (of liver function) and Dagradi (of esophageal varices) (14).
In this study, in which 70 patients were included, there was a higher correlation between
P/B and Dagradi, with a higher percentage of patients in Child-Pugh stages B and C, compared to
other studies.
As mentioned above, performing endoscopy for esophageal varices screening every one to two
years in high-risk patients can be difficult and impractical (9).
Non-invasive parameters associated with high-risk esophageal varices help to reduce the need for
endoscopic studies to be performed at this frequency and can be used to distinguish between high-
and low-risk patients. This could be used to follow up only high- or very high-risk patients with
endoscopic studies (6,9,10,12).
It is also necessary to mention that a diagnostic endoscopy for esophageal varices should be
performed in patients with risk factors, such as a Child-Pugh A (12,13,15).
However, the P/B index is useful for stratification of cirrhosis patients into risk
categories where portal hypertension data exist. This is especially relevant for those patients
whose health status and conditions do not allow an invasive study, but who are at high risk of
developing esophageal varices (6,9,10,12).
In this study, most of the patients had Child-Pugh B and C classification. These stages are
those with the highest risk to be associated with esophageal varices and bleeding according to
international literature (9,12-15).
The results of the test performed on the P/B index are consistent with other studies,
although some show wide ranges of variability among them (6,8,13-15).
The P/B is strongly associated with the presence of esophageal varices (1,6,13,14), and its
negative predictive value is reproducible, in this study with 75% and with a diagnostic certainty of
88%.
CONCLUSION
In conclusion, the P/B index presents false negatives of 9%, with a positive predictive value of 94%, a negative predictive value of 75%, with a prevalence of 74% and a diagnostic certainty of 88%, so it can be considered a useful and non-invasive study to diagnose esophageal varices especially in places , without availability of endoscopy.
Authorship contributions: All authors conceived and designed the article, collected,
analyzed and interpreted the data, revised the article critically and drafted the final version.
Funding sources: Self-funded
Conflicts of Interest: The authors declare that there is no conflict of interest
regarding the publication of this brief article.
Received: January 16, 2021
Accepted: February 20, 2021
Correspondence: Álvaro José Montiel-Jarquín.
Address: Calle 2 norte Nº 2004. Colonia Centro. CP 72000. Puebla,
Puebla-México.
Telephone number: +52 (222) 2424520 extensión 61315. Teléfono móvil: +521
2222384907
E-mail: dralmoja@hotmail.com ; neurogarciagalicia@yahoo.com.mx
REFERENCES