REPORTE DE CASO
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2021 - Universidad Ricardo Palma10.25176/RFMH.v21i4.3799
SHOCK CRYPTIC, EMERGING DIAGNOSTIC
SHOCK CRÍPTICO, DIAGNÓSTICO INCIPIENTE
Ricardo Ayala Garcia1,2,a, Sandra Soto Ticse1,3,b, Stephany Matos
Santiváñez1,4,b, Allison Ortiz de Orue1,4,b
1 Hospital Nacional Edgardo Rebagliati Martins. Lima, Perú.
2 Universidad Nacional de Piura. Piura.
3 Universidad Nacional Mayor de San Marcos. Lima, Perú.
4 Universidad Ricardo Palma. Lima, Perú.
a Médico Emergenciólogo.
b Médico Residente.
ABSTRACT
Cryptic shock is a poorly identified clinical entity, and it still describes a patient with signs of tissue hypoperfusion without affecting blood pressure. In the emergency department, it is important to identify signs of hypoperfusion and evaluate various hidden sources of infection by taking a complete medical history, a thorough physical examination, and, if necessary advanced imaging. It is necessary to conclude that the importance of the timely diagnosis of this clinical entity helps to improve the prognosis significantly.
Keywords: Sepsis; Shock; Lactic acid (source: MeSH NLM).
RESUMEN
El shock críptico es una entidad clínica poco identificada, describe aún paciente con signos de hipoperfusión tisular sin afectación de la presión arterial. En el departamento de emergencia es importante identificar signos de hipoperfusión y evaluar diversas fuentes ocultas de infección realizando una historia clínica completa, un examen físico exhaustivo y de ser necesario imagenología avanzada. Es necesario concluir que la importancia del diagnóstico oportuno de esta entidad clínica ayuda a mejorar significativamente el pronóstico.
Palabras Clave: Sepsis; Shock; Ácido láctico (fuente: DeCS BIREME).
INTRODUCTION
Shock is a pathophysiological entity consisting of tissue hypoperfusion, and it is frequent in emergency
services (1). Traditionally four types of shock have been described:
hypovolemic, obstructive, cardiogenic, and distributive; the reported incidence of the latter is 66%,
around 64% corresponding to septic shock (2). Shock is considered
life-threatening if it is not diagnosed and managed promptly, mortality ranges between 40-60% and septic
shock in 40%. When it is associated with organ dysfunction, lethality is significantly higher (3).
A significant proportion of patients who present with shock are associated with arterial
hypotension. There is a group of patients with “cryptic shock” who present with signs of tissue
hypoperfusion and normal ranges of blood pressure (4), Two profiles of septic
shock are described, classic (associated with hypotension) and cryptic (severe sepsis “old
classification, associated with lactate elevations) (5); Normotensive patients
with elevated lactate were found to have a 15% higher mortality rate (3).
Many of the patients admitted to the emergency services present hypoperfusion and can remain
undetected. Often many of these patients require alterations in blood pressure levels to be identified
with hemodynamic compromise (6).
We present the case of a patient with cryptic shock according to recent definitions with no
evident infectious focus on admission to the emergency service.
CASE REPORT
73-year-old male patient, independent baseline status, with a history of arterial hypertension, 3 days
before admission, was evaluated in the emergency service for presenting a level fall (not witnessed by
family members), causing contusion to frontal level, left periorbicular; discharged with symptomatic
medication.
He was admitted to the shock trauma unit due to a disorder of consciousness and an episode of
vomiting of food content. The evaluation found the patient in poor general condition, blood pressure 120
/ 80mmHg, heart rate 109, respiratory rate 24, oxygen saturation 91% with Venturi mask at FiO2 0.4. He
was found soporous, with the Glasgow Coma Scale (Ocular opening 1 Verbal response 2 Motor response 5)
8/15, with mobilization of the 4 extremities, evidence of periorbicular ecchymosis and edema of the left
eyelid, wound faced with purulent discharge at the level of left eyelid, erythema on upper lip; rhythmic
heart sounds of regular intensity; Audible vesicular murmur in both lung fields and bilateral snoring.
Capillary filling of approximately 4 seconds, predominantly marbled skin on the lower extremities. The
arterial blood gas showed mild acidemia due to respiratory acidosis and partially corrected hypoxemia
and elevated lactate; samples were sent to the laboratory for serum tests (Table
N°1). The diagnoses of hypoxemic-hypercapnic respiratory failure were raised, probably
attributed to a pneumonic process, a sensory disorder to rule out intracerebral hemorrhage due to head
trauma. A peripheral line and a drip saline infusion were placed, and intubation was carried out using
fentanyl, midazolam and was connected to mechanical ventilation with protective parameters. He was
transferred to the imaging room. A brain and thoracic tomography without contrast was performed, which
did not show ischemic or acute cerebral hemorrhagic lesions, the lung parenchyma without infiltrates, or
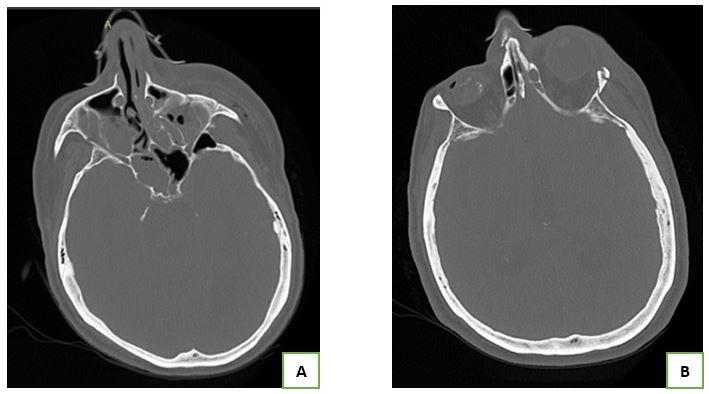
pleural effusion (Figure N°1).

B) Brain tomography without contrast, there is no evidence of ischemia or acute hemorrhage. aguda.
Despite not receiving sedative drugs, he persisted with impaired consciousness. In addition, a fever peak of 38.5 ° C was evidenced. Laboratory tests showed leukocytosis and neutrophilia (Table N°1) and he was carefully reassessed to locate the probable focus of infection. Physical examination revealed no changes concerning admission, and no meningeal signs were found. As the infectious focus was not objective, the radiologist was consulted to evaluate the tomographic images in detail, which in the three-dimensional reconstruction showed a fracture of the lateral wall of the left orbit and maxillary sinus on the same side accompanied by haemosen, associated with changes suggestive of an inflammatory process of the adjacent tissue (Figure N°2). Based on the findings, it was decided to perform lumbar puncture and start of corticosteroids and broad spectrum antibiotic coverage (ceftriaxone + vancomycin + ampicillin), cloudy cerebrospinal fluid (CSF) was obtained with an opening pressure of 35 cm H2O, samples were sent for cultures and cytochemicals.
B) Left orbit lateral wall fracture. aguda.
Table 1. Laboratory results.
| Test | Results | Reference |
|---|---|---|
| Arterial gases | ||
| FiO2 | 0.4 | |
| PO2 | 67 mmHg | 86 – 100 |
| PCO2 | 47 mmHg | 35 – 45 |
| PH | 7.3 | 7.35 – 7.45 |
| HCO3 | 21 mmol/L | 22 – 26 |
| Lactato | 5.2 mmol/L | 0.5 – 1.6 |
| Hemogram | ||
| Leucocytes | 36.04 k/ul | 4.00 - 11.00 |
| Neutrophil | 92.9 % | 40 – 74 |
| Hemoglobin | 13.7g/dl | 14 -18 |
| Hematocrit | 42.1 % | 42 – 52 |
| Platelet | 380 k/l | 130 – 400 |
| Biochemical and electrolytes | ||
| Creatinine | 0.92 mg/dl | 0.6 - 1.1 |
| Glucose | 279 mg/dl | 74 – 106 |
| Urea | 39.9 mg/dl | 22 – 55 |
| Potassium | 2.99 mmol/L | 3.5 - 5.5 |
| Sodium | 149.4 mmol/L | 132 – 146 |
| Chlorine | 101.9 mmol/L | 99 – 109 |
| Urine test | Negative | |
The patient presented with arterial hypotension, initiating fluid bolus without obtaining a response. The norepinephrine infusion proceeded until an adequate mean arterial pressure was obtained. CSF cytochemical and lactate results are obtained (Table N°2), which shows predominantly polymorphonuclear cells, hypoglycorrhachia and protein sprain, significantly elevated lactate.
Table 2. CSF laboratory results.
| Test | Results | Reference |
|---|---|---|
| CSF cytochemical | ||
| Color | Xanthochromic | |
| Appearance | Hazy | |
| Glucose | 1 mg/dl | 45 – 80 |
| Proteins | 898.5 mg/dl | 15 – 40 |
| Rcto, leukocyte | 1120 cel x mm3 | |
| Pmn | 95 % | |
| Mononuclear | 5 % | |
| Lactate | 23 mmol/L | |
The diagnoses of septic shock due to meningoencephalitis secondary to maxillary sinus-orbit fracture were reconsidered. Fluid therapy was optimized, and vasoactive titration was continued until stabilization. He was transferred to the neurocritical unit to continue treatment and monitoring. Three days the positive culture for Streptococcus Pneumoniae was confirmed; At the moment, the patient continues in the hospitalization area, finishing treatment for in-hospital pneumonia, stable without the need for supplemental oxygen.
DISCUSSION
However, the identification of patients with hemodynamic compromise in the emergency rooms is frequently
discriminated by the existence of an alteration in blood pressure; it is evident that many patients
present with signs of tissue hypoperfusion on physical examination, significant elevations of lactate
and normal blood pressure levels; therefore, it makes early identification and timely management
difficult, with mortality being higher in this group of patients (3). The
emergency physician must be judicious when assessing the compromise of the airways and the existence of
signs of tissue hypoperfusion and establish appropriate management in the first hours until hemodynamic
stabilization is guaranteed and proceed in a more exhaustive manner to search for the cause of shock
(1). Currently within the systematized evaluation of the patient with shock,
rapid diagnostic methods have been introduced at the bedside, ultrasound is a useful tool used by
emergency physicians for the non-invasive evaluation and classification of the hemodynamic profile of
the patient with shock, the same; allows to reduce the differential diagnosis and increase the
diagnostic precision for timely management (7) (8).
Not all centers have this tool, in the case reviewed it was not possible to perform an ultrasound
evaluation, in addition to the presence of normal blood pressure values and underestimating the signs of
tissue hypoperfusion, an adequate diagnostic and therapeutic approach was not directed. Distributive
shock is one of the most frequent types of shock reported (2), the most
frequently described infectious foci are respiratory 42.1%, gastrointestinal 31.4%, genitourinary 6.1%.
No infectious focus is found in the initial evaluation in 11% of In patients, a minor proportion 1.5% is
attributed to infections of the central nervous system (9). It is important to
evaluate hidden sources of infection by taking a complete medical history, a thorough physical
examination, and, if necessary advanced imaging (1). In the case presented,
the history of recent head trauma led to the suspicion of probable involvement of the central nervous
system, despite the absence of meningeal-parenchymal involvement in the physical examination, on the
other hand, only the classic triad of fever - neck stiffness - altered mental status in 41 - 51% of
cases, so the absence of these findings cannot be used to rule out the possibility of bacterial
meningitis (10); It was reported that the incidence of post-ECT meningitis
varies from 0.2% - 17.8% and increases significantly in the presence of skull base fracture,
pneumocephalus, loss of cerebrospinal fluid (11), with high mortality of 29 -
57.9% (12).
Currently, some reviews try to introduce a new classification system for septic shock according
to vasoactive agents and serum lactate, however, the evidence is not sufficient (5). No differences in mortality were found in the septic shock profiles
described "classic septic shock" - "cryptic shock" (5), however; patients with
lactate levels of 2.5 - 4 mmol / L have an increased risk of death of 2.2, and those with lactate ≥4
mmol / L have a risk of 7.1 times higher (6).
CONCLUSION
The challenge for the emergency physician is to identify early patients who present with signs of tissue hypoperfusion, without alteration of blood pressure values. A medical history directed to the search for antecedents or triggers, a focused clinical examination and the aid of tools such as ultrasound are essential in the evaluation of the patient with shock. The importance of timely diagnosis and avoiding hemodynamic deterioration where the alteration of blood pressure levels is evident significantly improves the prognosis. Cryptic shock as a recently described clinical entity will allow early identification of patients with shock without significant hemodynamic compromise and thus establish early management and reduce patient morbidity and mortality.
Authorship contributions: RAG participated in the conception, design of the article,
writing and approval of the final report. In addition, SST, SMS and AOO have participated in the
collection of data from the clinical history and approval of the final report.
Financing: The research was self-financed.
Conflicts of Interest: The authors declare no conflict of interest.
Received: May 13, 2021
Approved: July 11, 2021
Correspondence: Ricardo Jonathan Ayala García
Address: Av Prolongación Iquitos 1542. Dpto 1503, Lince, Lima, Perú.
Telephone: 961066414
E-mail: jag-mrng@hotmail.com, ricardo.ayala@unmsm.edu.pe
BIBLIOGRAPHIC REFERENCES
