REPORTE DE CASO
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2021 - Universidad Ricardo Palma10.25176/RFMH.v21i4.3902
POSNER – SCHLOSSMAN SYNDROME: CASE REPORT
SINDROME DE POSNER - SCHLOSSMAN: REPORTE DE CASO
Diego José Mamani Maquera 1,2,a Nahuel Pantoja Dávalos 1,3,b
1 Hospital Nacional Carlos Alberto Seguín Escobedo - EsSalud. Arequipa, Peru
2 Universidad Nacional de San Agustín. Medical school, Arequipa, Peru
3 Universidad Nacional Mayor de San Marcos. Medical school, Lima, Peru
a Resident Physician of Ophthalmology
b Assistant Ophthalmology Physician
ABSTRACT
Introduction: Posner - Schlossman Syndrome (PSS) is a rare disease, more prevalent in men between 20 and 50 years old, characterized by recurrent attacks of anterior uveitis and ocular hypertension. Clinical case: We report the case of a 42-year-old patient with a single eye. He came to the consultation presenting decreased visual acuity, photobobia, halos around the lights, and intense pain in his left eye. The ophthalmological examination revealed inflammatory signs in the anterior segment, elevated intraocular pressure and damage to the optic nerve. Medical treatment was started with corticosteroids and topical antiglaucoma drugs, oral acetazolamide and intravenous mannitol, obtaining no response and it was decided to perform a surgical intervention (Ahmed valve implantation) in the left eye, subsequently achieving a good clinical evolution and resolution of the case. Conclusion: This report highlights that the episodic and recurrent nature of SPS requires strict monitoring.
Keywords: Posner-Schlossman syndrome, anterior uveitis, ocular hypertension (Source: MeSH NLM).
RESUMEN
Introducción: El Sindrome de Posner - Schlossman (SPS) es una enfermedad infrecuente, de mayor prevalencia en hombres de entre 20 a 50 años, que se caracteriza por presentar ataques recurrentes de uveítis anterior e hipertensión ocular. Caso clínico: Reportamos el caso de un paciente de 42 años, con ojo único. Acudió a consulta presentando disminución de la agudeza visual, fotobobia, halos alrededor de las luces y dolor intenso en su ojo izquierdo. Al examen oftalmológico se evidenciaron signos inflamatorios en segmento anterior, presión intraocular elevada y daño en el nervio óptico. Se inició tratamiento médico con corticosteroides y antiglaucomatosos tópicos, acetazolamida oral y manitol endovenoso, no obteniendo respuesta y se optó por realizar una intervención quirúrgica (implante de válvula de Ahmed) en el ojo izquierdo, logrando posteriormente una buena evolución clínica y resolución del caso. Conclusión: Este reporte resalta que la naturaleza episódica y recurrente del SPS requiere un seguimiento estricto.
Palabras Clave: Sindrome de Posner - Schlossman, uveítis anterior, hipertensión ocular (Fuente: DeCS BIREME).
INTRODUCTION
Posner-Schlossman Syndrome (PSS) or glaucomatocyclitic crisis is a rare disease characterized by
recurrent attacks of non-granulomatous anterior uveitis and elevated intraocular pressure (IOP) (ocular
hypertension). This is frequently classified as a secondary inflammatory glaucoma (1,2,3).
PSS main clinical manifestations are elevated IOP and blurred vision, tending to affect patients
between 20 and 50 years old, most often men than women. The episodes are unilateral, although in 50% of
patients the other eye is involved at some point. Intervals between attacks vary, but usually lengthen
over time (1,4).
The etiology of PSS has been investigated in some studies, which indicated that PSS may be
associated with cytomegalovirus (CMV) infection, genetic susceptibility, inflammatory cytokines, and
vascular endothelial dysfunction. Among these, CMV infection is considered a vital risk factor for PSS
(5,6).
PSS diagnosis is inherently difficult. The subtlety of some features of low-grade anterior
uveitis and the short-lived nature of each attack makes it hard to diagnose. PSS must be differentiated
from acute angle-closure glaucoma, primary open-angle glaucoma, uveitic glaucoma, and Fuchs
heterochromic iridocyclitis (7).
Treatment for PSS is aimed at controlling inflammation and elevated IOP. However, some patients
do not respond to corticosteroids or antiglaucoma medications. In these cases, surgery is needed to
lower the IOP and thus prevent the visual field defects progression and damage to the optic nerve
(3,8).
This case refers to a patient with a history of SPS attacks, who initially received maximum
anti-inflammatory and anti-glaucoma medical treatment, but as there was no response, surgical treatment
was required.
Clinical case
We present the case of a 42-year-old man who presented with decreased visual acuity,
photophobia, halos around lights, and severe pain in his left eye (LE) for 5 days. The patient refers
that these symptoms have been presenting for 4 years in a mild and transitory way, so he has not
required medication.
As an ophthalmological history, the patient underwent surgery for ocular trauma in the right eye
(RE) approximately 30 years ago, with poor subsequent evolution. At ophthalmological examination, he
presents a corrected visual acuity of no light perception in RE and 20/70 in LE. IOP was 15 mmHg in the
RE and 50 mmHg in the LE. In the anterior segment examination with a slit lamp in the RE, an extensive
corneal opacity of central predominance of whitish-gray appearance with stromal deposits was evidenced,
which did not allow to see other details of the anterior segment; n the LE, mild corneal edema was
evidenced, with the presence of fine keratic precipitates in the middle third and lower 1/3 of the
corneal endothelium, no atrophy or heterochromia of the iris, anterior chamber reaction: Tyndall and
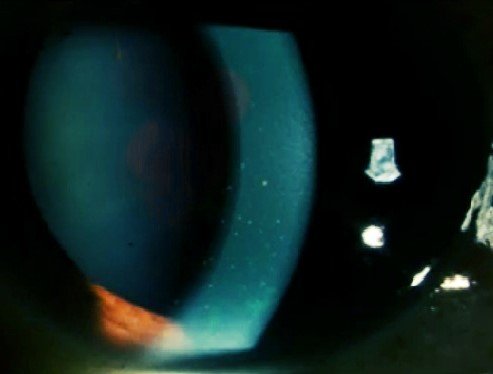
Flare (1+), wide anterior chamber, lens opacity NO1 NC1 C2 P1, 360 ° cilium-conjunctival injection (Figure 1). At gonioscopy, the RE could not be evaluated due to corneal opacity, the
LE showed an open angle (Shaffer grade IV). In the fundus examination, the RE could not be evaluated due
to the opacity of the media, in the LE a papilla with defined edges was evidenced, excavation of 0.4,
with nasal rejection of the central vessels, with preserved macular shine, without inflammation signs in
the posterior segment (Figure 2).
|

|
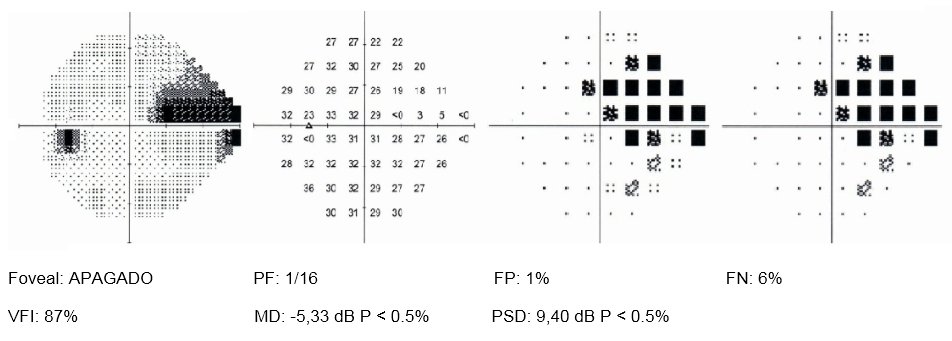
Visual field exploration was performed with program 24-2 of the Humphrey visual field analyzer, which revealed the presence of a nasal step in the LE (Figure 3).
Laboratory tests were requested: complete blood count (CBC), acute phase reactants, antinuclear
antibodies, rheumatoid factor, toxoplasmosis serology, serology for cytomegalovirus, serology for
syphilis, serology for HIV, serology for HTLV 1 and 2, serology for hepatitis, all of which were normal.
Due to all the above, the diagnosis of Posner-Schlossman syndrome is made and medical treatment
with Acetazolamide (250mg) is started. 1 tablet every 8 hours, Brimonidine (0.2%) 1 drop every 12 hours,
Dorzolamide (2%) 1 drop every 8 hours, Timolol (0.5%) 1 drop every 12 hours and Prednisolone (1%) 1 drop
every 4 hours in the LE. It was reassessed 48 hours after starting the medical treatment, the patient
reported that the symptoms had not improved, the decrease in IOP to 40 mmHg and the persistence of
inflammatory signs in the anterior segment of the LE. Mannitol (20%) 250 ml is added every 8 hours
intravenously. A new evaluation is carried out 5 days after starting medical treatment and a decrease in
IOP to 30 mmHg in LE is observed, therefore it is evident that there was not an adequate response to
maximum medical treatment.
Faced with this situation, it was decided to place a drainage device and extract the cataract
from the LE. Surgical treatment is performed by implanting the Ahmed valve, phacoemulsification, and
placement of an intraocular lens in LE
In the postoperative period, the IOP was normal, without any pharmacological medication. A week
after surgical treatment, a visual acuity of 20/25 was obtained with correctors and an IOP of 10 mmHg
with clinical relief of ocular symptoms in the LE.
The follow-up was carried out initially once a week, then monthly, IOP remained normal without
any pharmacological medication for more than 6 months after surgery, without attacks of PSS.
DISCUSSION
Posner - Schlossman syndrome is a rare disorder, a form of anterior uveitis with ocular
hypertension and a higher prevalence in men between 20 and 50 years old(9),
characteristics that correspond to our patient, who was 42 years old and presented the characteristic
clinical picture of this disease.
Posner-Schlossman syndrome has some clinical features of glaucoma and uveitis, such as ocular
hypertension and the presence of retrokeratic precipitates (10). These
inflammatory signs (retrokeratic precipitates and reaction in the anterior chamber) and the markedly
elevated intraocular pressure were described in the initial clinical picture presentation in our
patient.
Early diagnosis and proper treatment may lower the risk of advanced glaucoma. Frequent attacks
of ocular hypertension are particularly dangerous because they can easily affect vision by causing
progressive visual field defects. Therefore, IOP control is the most important goal of treatment
(1,10).
Initial treatment for PSS is a combination regimen of anti-inflammatory and anti-glaucoma drugs.
A topical corticosteroid is often successful in controlling inflammation. Ocular hypertension usually
normalizes with control of inflammation. Topical β-blockers and / or carbonic anhydrase inhibitors are
the drugs of choice in patients with PSS. Prostaglandin analogs efficacy in PSS is not well established.
α2-agonists may also represent a good therapeutic option. If PSS attacks show higher frequency and IOP
fluctuations are significant with attacks, surgical intervention may be indicated (10,11). The most commonly indicated technique is filtering
surgery (Trabeculectomy), especially in patients with recurrent attacks and IOP peaks, with damage to
the optic nerve and visual field defects (12). Another technique also used is
valve implant drainage device surgery, which in many studies is considered the preferred first-line
surgery in the treatment of uveitic glaucomas(13,14). Our
patient received maximum medical treatment, which was insufficient for IOP control, so a surgical
intervention was finally performed, placing a valved drainage device (Ahmed valve).
PSS is known as a self-limited ocular disease with benign prognosis, but glaucomatous
deterioration of visual function in some patients is increasingly reported, therefore, early diagnosis
and appropriate treatment of SPS could decrease the risk of progression to advanced glaucoma (15,16).
CONCLUSIONS
Posner-Schlossman syndrome or glaucomatocyclitic crisis is a rare disease, characterized by recurrent attacks of anterior uveitis and ocular hypertension. PSS usually has a good response to medical treatment, but as observed in the present case, IOP could not be controlled, so a surgical intervention was required, achieving a good clinical evolution after this. The episodic and recurrent nature of PSS requires close monitoring, therefore, patients with SPS should have regular evaluation of visual acuity, visual field, and IOP.
Authorship contributions: The authors carried out the design, information gathering,
preparation, critical review and approval of the final version of the article.
Funding sources: Self-financed.
Interest Conflicts: The authors declare that they have no conflicts of interest in the
publication of this article.
Received: May 15, 2021
Approved: July 11, 2021
Correspondence: Diego José Mamani Maquera
Address: Calle Ronda Recoleta 303 – Yanahuara - Arequipa
Telephone: 942943535
Email: md.diegojose@gmail.com
REFERENCES