ARTICULO ORIGINAL
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2021 - Universidad Ricardo Palma10.25176/RFMH.v21i3.3905
Cost of pulmonary arterial hypertension in Peru
Costo de la hipertensión arterial pulmonar en el Perú
Fabián Hernández1; Julieta Larrosa2; Jessica Nacazume3; Oscar
Aguirre4; Nelson Larrea5; Sarah Franco-Watanabe3; Jorge
Álvarez5; André Morais5
1. IQVIA Colombia – Bogotá, Colombia
2. IQVIA México – Ciudad de México, México
3. IQVIA Brasil – São Paulo, Brasil
4. Instituto Nacional Cardiovascular (INCOR) – Lima, Perú
5. Janssen Pharmaceuticals
ABSTRACT
Introduction: Pulmonary arterial hypertension (PAH) is a low prevalence condition for which there is very little information in Peru. Various studies indicate that it generates significant costs for health systems in the world. Objective: To establish the economic burden of PAH in the Peruvian context. Methods: Information on the use of health resources was collected through consultations with clinical experts and opinion leaders. The cost information was obtained from two tariff manuals and the Observatory of Pharmaceutical Products. Results: The experts indicated that about 68% of the patients were in an intermediate stage of the disease and that sequential combination therapy is predominant in the FC III and FC IV stages, compared to earlier stages. The annual cost of PAH treatment in Peru was $ 14,842 USD (S / 25,885), where the main item were drugs (81.72%), followed by diagnosis (8.96%) and outpatient follow-up (5, 75%). Conclusion: Information on pulmonary arterial hypertension in Peru is critical for decision-makers due to the high economic impact. Furthermore, studies in this therapeutic area are relevant for disseminating knowledge of the disease to different health professionals.
Keywords: Pulmonary Arterial Hypertension, Cost of Illness, Peru.
RESUMEN
Introdución: La hipertensión arterial pulmonar (HAP) es una condición de baja prevalencia para la que existe muy poca información en el Perú. Diversos estudios indican que genera costos importantes para los sistemas de salud en el mundo. Objetivo: Establecer la carga económica de la HAP en el contexto peruano. Métodos: La información de uso de recursos en salud se recolectó por medio de consultas a expertos clínicos y líderes de opinión. La información de costos fue obtenida de dos manuales tarifarios y del Observatorio de Productos farmacéuticos. Resultados: Los expertos indicaron que alrededor del 68% de los pacientes se encontraban en un estadio intermedio de la enfermedad y que el uso de terapia combinada secuencial es predominante en los estados FC III y FC IV, en comparación con estadios más tempranos. El costo de tratamiento anual de la HAP en el Perú fue de $14.842 USD (S/ 25.885), donde el principal rubro fueron los medicamentos (81,72%), seguido del diagnóstico (8,96%) y seguimiento ambulatorio (5,75%). Conclusión: La información sobre la hipertensión arterial pulmonar en el Perú es crítica para los tomadores de decisión, debido al alto impacto económico que conlleva. Más aún, estudios en esta área terapéutica son relevantes para la difusión del conocimiento de la enfermedad a los diferentes profesionales de la salud.
Palabras clave: Hipertensión Arterial Pulmonar, Costo de Enfermedad, Perú.
INTRODUCTION
Pulmonary hypertension groups have different low prevalence conditions that have a similar
clinical presentation. It is defined as a mean pulmonary arterial pressure greater than 25 mmHg at rest
and greater than 30 mmHg during exercise. Among the conditions grouped by pulmonary hypertension,
pulmonary arterial hypertension (PAH) stands out, which, in addition to the previous criteria, is
characterized by a wedge pressure of the pulmonary artery less than 15 mmHg (1,2). The increase in pressure is mainly caused by an increase in the vascular
resistance of the pulmonary arteries that can have genetic, environmental, or idiopathic etiology;
therefore, the risk factors for the development of PAH are related to genetic mutations (especially in
the BMPR2 gene) (3), congenital heart problems (4),
living in high altitude regions (5) and the consumption of some drugs or
substances (6).
Currently, there is no information on the prevalence or incidence of PAH in Peru. However, the
prevalence of this disease in high-income countries is estimated to be between 5 and 52 cases per
million inhabitants, with an incidence of 2.5 to 7.1 new cases per million inhabitants (7). Given its low prevalence, this disease has been classified as an orphan
disease, according to Ministerial Resolution 1075 of 2019 of the Ministry of Health of Peru, so its care
and treatment are guaranteed by the national government (8,9).
Since the diagnosis of PAH usually requires active screening of patients with risk factors and
preexistence (10), and that the pharmacological treatments indicated for this
condition are expensive (11), the burden imposed on the health of the system
is considerable. In this sense, a systematic review of cost studies in PAH found that the monthly cost
per patient per month varies between the US $ 2,476 and $ 11,875, where the costs related to
pharmacological treatment and medical care were the key sources of direct medical costs (12). Similarly, some studies have estimated that there are significant
differences in the cost of the disease by Functional Classification (FC) of the World Health
Organization (WHO) (13), so it becomes relevant to know this economic burden
within the Peruvian health system.
The objective of the present study was to estimate the economic burden associated with the
diagnosis, treatment, and follow-up of PAH from the perspective of the Peruvian third-party payer.
METHODS
Design and study area
This study was based on in-depth interviews with four cardiologists with experience in the management of PAH in reference centers in Peru.
Population and sample
The universe of patients covered by these specialists was 186 patients during 16 years of clinical practice.
Variables and instruments
The analysis variables are the costs related to the events associated with PAH. Information collection instruments were developed based on the proposed objectives, which guided the conduct of the interviews. These were intended to identify the use of resources and relevant cost-generating events in the treatment of patients with a diagnosis of PAH from the perspective of the Peruvian third-party payer, in this case, MINSA and EsSalud only those that generated costs were considered to direct physicians.
Procedures
The study consists of two phases: the first consists of interviews with clinical experts to determine the management of PAH; the second focuses on the performance of microcosting related to events associated with PAH. The approach followed both in the interviews and in the cost estimation is summarized below.
Identification of resources and cost-generating events
The four cardiologists were consulted regarding five relevant aspects of these patients’ health care: diagnosis, drug treatment, outpatient follow-up, in-hospital care, and adverse events (AE). The questionnaires that guided the interviews were prepared based on the guidelines of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS) for the treatment of PAH (14). Similarly, the experts were questioned regarding the functional classification of the patients they treated and its etiology.
Cost estimation
Each resource and the cost-generating event was assigned a price-weighted by the frequency of use and the proportion of patients to which each was prescribed to estimate the total cost of PAH in Peru per patient per year. This approach is called microcosting, and its use is common in economic evaluations (15). In Peru, the sources of costs for procedures and consultations were the rate manuals of the National Institute of Neoplastic Diseases and the Cayetano Heredia Hospital (16,17). For drugs, the database of the Pharmaceutical Products Observatory (DIGEMID / MINSA) was consulted Statistical analysis. The final cost of the disease was expressed in United States dollars (USD) adjusted for Purchasing Power Parity (PPP), which allows the comparison of the acquisition of goods and services between different economies since this value is less sensitive to changes in supply and demand. In this study, the conversion rate of the Peruvian sol to USD PPP for 2018 was used, which is equivalent to S / 1,744 for each USD.
Ethical consideration
This study did not require intervention in humans, so there is no need for review by an ethics committee.
RESULTS
Within the universe of patients comprised by the cardiologists interviewed, it was evidenced that 63.7%
of patients with PAH had a diagnosis associated with congenital heart disease, 20.8% corresponded to
patients with a disease of idiopathic etiology, and 8.5% of the patients had a disease associated with
connective tissue disorders. On the other hand, the experts consulted indicated that they stratified the
patients mainly by functional class, showing that 68% of them were in intermediate stages of disease
severity (32% in FC II and 36% in FC III). In contrast, 15% and 16% of patients were in FC I and FC IV
states, respectively.
In general, the report on the use of resources (procedures and laboratories) for the diagnosis
of PAH was quite homogeneous among the experts interviewed, generating an average annual cost of
diagnosis of $ 1,329.9 per patient. Regarding the cost of outpatient follow-up, the use of resources was
more heterogeneous among specialists, and its total annual cost was $ 852.9 per patient. On the other
hand, the annual cost of non-pharmacological treatment and adverse events corresponded to $ 276.4 and $
1.10, respectively (Table 1).
Regarding hospitalizations and length of hospital stay, the experts consulted indicated that
patients in FC I and II states usually do not report hospitalizations or admissions to the Intensive
Care Unit (ICU); therefore, they do not incur costs related to this item. In contrast, FC III and FC IV
patients spend an average of 12 and 14 days a year in the general hospitalization room and 7 and 7.5
days a year in the ICU, respectively. The cost of the general inpatient ward stay is $ 595.5 and $ 693.1
for FC III and FC IV patients, respectively. The cost of staying in the ICU is 1,404.6 and 1,490.7,
respectively.
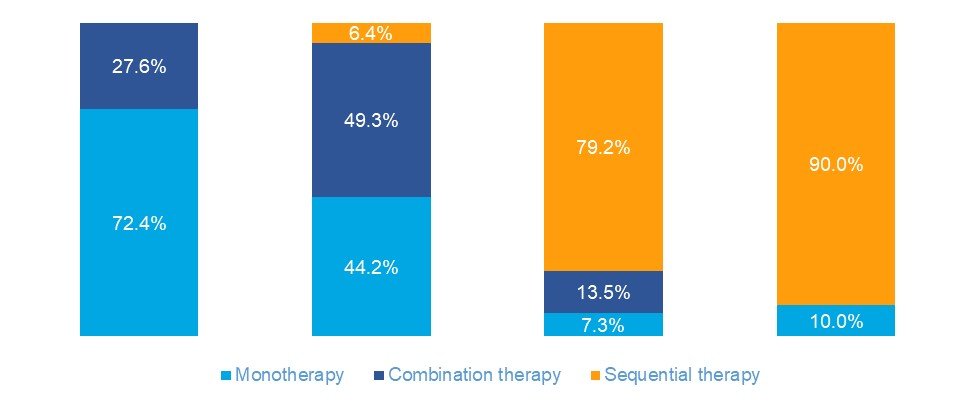
Regarding pharmacological treatment, it was evidenced that sequential combination therapy is
predominant in the FC III and FC IV states. In contrast, in the FC I and FC II state, the use of
monotherapy and initial combination therapy is much more common (Figure 1).
Similarly, it was observed
that the most widely used pharmacological alternative for the treatment of PAH in Peru was sildenafil,
followed by the combination of sildenafil + bosentan (Figure 2). Adjuvant treatment
in this setting
consisted of anticoagulants, diuretics, and digoxin.
In general, the distribution of the costs of diagnosis, follow-up and non-pharmacological
treatment within the total cost of treatment remained constant throughout the different stages of
disease severity. Additionally, it was observed that the cost of pharmacological therapy constitutes the
largest proportion of the total cost of treatment (Table 2) per year per patient,
which, in this case,
was $ 14,841.7.
Table 1. MAIN PROCEDURES AND LABORATORIES FOR EACH TREATMENT STEP IN USD. PPA: PURCHASING POWER PARITY
| Procedure | Quantity | Proportion | Annual cost per patient (PPA) |
|---|---|---|---|
|
Diagnostic procedures |
|||
| Left heart catheterization | 1 | 100.0% | $ 251.48 |
| Pulmonary exploration by ventilation/perfusion | 1 | 100.0% | $ 202.07 |
| Transesophageal echocardiography | 1 | 100.0 % | $ 160.73 |
| MRI of the heart | 1 | 37.6% | $ 157.49 |
| Pulmonary angiography | 1 | 37.6% | $ 86.42 |
| Computed tomography | 1 | 93.0% | $ 85.43 |
| Right heart catheterization | 1 | 100.0% | $ 57.41 |
| X-ray of chest | 1 | 100.0% | $ 47.65 |
| DLCO (Carbon monoxide pulmonary diffusion test) | 1 | 93.0% | $ 45.92 |
| Electrocardiogram | 1 | 100.0% | $ 29.85 |
| Other procedures | 1 | - | $ 205.46 |
|
Outpatient follow-up |
|||
| Transesophageal echocardiography | 1 5 | 100.0% | $ 241.10 |
| brain natriuretic | 2.5 | 100.0Peptide% | $ 107.63 |
| thyroid function test | 2 | 100.0% | $ 99.89 |
| right heart catheterization | 1.5 | 100.0% | $ 86.11 |
| Electrocardiogram | 1 5 | 100.0% | $ 74.63 |
| Ionogram | 2.5 | 100.0% | $ 47.36 |
| Hematocrit | 2 | 100.0% | $ 34.44 |
| 6MWT: Test 6 minute walk | 1.5 | 10 0.0% | $ 26.69 |
| Serum iron | 2 | 100.0% | $ 26.41 |
| Prothrombin time | 3 | 100.0% | $ 18.94 |
| Other procedures | - | 100.0% | $ 89.66 |
|
Adverse events |
|||
| Headache | 1 | 44.3% | $ 0.49 |
| Elevation of transaminases | 1 | 44.4% | $ 0.49 |
| Hypotension | 1 | 11.2% | $ 0.12 |
|
Other follow-ups and outpatient treatments |
|||
| Physical rehabilitation therapy | 1.6 | 100.0% | $ 121.0 |
| Consultation with a PAH specialist | 5.3 | 100.0 % | $ 61.1 |
| Psychological assistance | 2.6 | 100.0% | $ 34.6 |
| Consultation with other specialists | 2 | 100.0% | $ 22.8 |
| Immunization against pneumococcal disease | 1 | 67.2% | $ 18.6 |
| Social assistance | 1.7 | 100.0% | $ 13.6 |
| Iron supplementation for anemia | 1 | 34.0% | $ 3.5 |
| Oxygen therapy | 1 | 25.9% | $ 1.2 |
Table 2. DISTRIBUTION OF ANNUAL TREATMENT COST PER PAH PATIENT IN PERU IN USD.
PPA: PURCHASING POWER PARITY
PAH: Pulmonary arterial hypertension
| Item | Total Cost (PPA) | Percentage |
|---|---|---|
| Diagnosis | $ 1,329.9 | 8.96% |
| Outpatient follow-up | $ 852.9 | 5.75% |
| Other follow-up and outpatient treatments | $ 276.4 | 1.86% |
| Adjuvant treatment | $ 148.8 | 1.00 % In- |
| hospital treatment | $ 91.0 | 0.61% |
| Transplantation | $ 12.7 | 0.09% |
| Adverse events | $ 1.1 | 0.01% |
| Pharmacological treatment | $ 12,128.9 | 81.72% |
| Total | $ 14,841.7 | 100.0% |
DISCUSSION
Information regarding the economic impact of PAH in Peru is scarce. However, this study makes it
possible to establish clear treatment patterns and some relevant cost-generating events within the
management stages of this pathology. Similarly, it is evidenced that most patients are in a moderate
stage of the disease, specifically in stages FC II and FC III, in which the evidence indicates that
there is a significantly different survival prognosis (18).
The drugs used in patients with functional classes I and II agree with the norms in
international guidelines. However, a group of patients that even in functional class II requires therapy
with drugs that use the prostaglandin pathway, specifically an agonist of selective IP receptors that
have shown a reduction in morbidity and mortality in this phase (19). In
patients with functional class III and IV, there are still cases with the use of monotherapy, which
reveals the limited access to recommended drugs at this level of the disease. Also, even when most
patients have indicated sequential therapy, it is restricted mostly to Sildenafil and Bosentan (Figure 2), making clear the risk of disease progression in advanced stages given
the need for prostaglandin
analogs in this group of patients. Of special attention is the group of patients in functional class IV,
who have a high risk of death or require transplantation. The indication of prostaglandin analogs should
be administered parenterally (20), drugs that are not yet available in the
national market.
Early diagnosis continues to be the best alternative to improve the prognosis of patients since
drugs are available locally for the early stages of the disease. However, it is known that even in
developed countries the delay in diagnosis ranges around 2 years (21), for
which early stratification is the next decision to be taken, there is evidence even in patients with FC
III and high risk where the Early and effective pharmacological intervention reduces rehospitalization
and disease progression (20). Finally, for patients diagnosed in advanced
stages, resources should be directed to specialized centers of reference, where the opportunity is given
to administer parenteral drugs in a protocolized manner, which allows the stabilization of the patient
and subsequent overlap with oral drugs that facilitate their treatment, administration, and adherence.
Pulmonary arterial hypertension (PAH) is a rare disease and, at the same time, generates a high
cost that can be analyzed from different aspects of the disease. The rapid progression towards
hospitalization and premature death in young adults is definitely reflected in high hospitalization
rates, Lacey et al., (22) reported that more than 75% of PAH patients were
hospitalized within the first year of diagnosis (mean hospital stay: 11 days), of which 20% were
readmitted again within 30 days (mean hospital stay 24.5 days) (23), which
significantly increases the cost of treatment. The advance in treatment, with the development of new
molecules that reduce hospitalization and stop the progression of the disease, is also related to a high
cost. The analysis focuses on establishing whether the new therapies impact reducing the costs
progression of the disease.
Retrospective studies have analyzed the costs of health care and medical resources used in the
diagnosis of PAH in the United States, Copher et al., (24) estimated costs
since diagnosis, reporting 8,187 US dollars (USD) per month, 94% of The patients were on monotherapy
(Sildenafil or Bosentan), being necessary to titrate the therapy in 13% of them, given this trend
established in the treatment routine, Sikirica et al., (25) estimated costs
during the diagnosis process (visit index) and 12 months later, the changes in treatment were:
titration, change of medication or discontinuation. The costs at this time estimated per year were
116,681 and 98,243 USD in the index visits and in the follow-up respectively, the decrease of these
estimates was despite an increase in the cost of the drugs used (Sildenafil, Bosentan, Ambrisentan,
Tadalafil, Iloprost Treprostinil, and Epoprostenol), they postulated that the result was due to the
reduction in hospital costs, which were significantly reduced (81,577 USD and 26,297 USD at the baseline
and follow-up visit respectively). This association was observed more recently in the study by Burger et
al., (26), with a greater number of patients included, where a greater than
50% reduction in the frequency of hospitalization for pulmonary hypertension was evidenced after
initiating specific vasodilator therapy. Hospitalization is a prognostic variable that is currently used
to measure in studies of pulmonary arterial hypertension, not only because of the high incidence
described and the costs involved (22), but also because it is a factor that
increases the mortality rate (27).
The low-risk profile is the goal to be achieved in patients with PAH (28). The goal is to avoid hospitalization as a proxy for mortality, for which
treatment adherence is essential. Some instruments allow it to be measured, such as the Morisky Scale or
the Proportion of days covered; Under these scales, patients with PAH generally show favorable adherence
values (29,30). However, these could be affected by multiple
factors, such as the need to use more than 1 drug, requiring multiple daily doses, or having PAH
associated with connective tissue diseases. The presence of comorbidities is a factor in favor of
adherence to multiple pharmacological therapies (29). Other clinical
variables considered were the presence of adverse events and hospitalization, which were associated with
lower compliance with treatment (30,31). The cost is not
mentioned within the related factors, but it is mentioned that more than 95% of the patients have
financial support from different assistance programs or foundations (30).
Among the limitations of this study is the use of the opinion of clinical experts as the primary
source of information since the estimates made could be biased towards the clinical practice of these
specialists and do not reflect the real-world scenario in this pathology. Similarly, since the only
specialty consulted for this study was cardiology, the characteristics described of the patients in this
research could only reflect those of the patients who attend cardiology to treat this condition. On the
other hand, considering that the experts consulted have extensive experience in the treatment of PAH,
the use of resources and the patient's time probably correspond to the ideal or recommended course of
treatment for these patients; however, in the real world, many patients may not arrive quickly for
consultation with a PAH specialist, so their use of resources and treatment alternatives may differ
significantly from the estimates presented in this study.
Finally, this reality prompts us to do more outreach and education about this disease towards an
increasingly early diagnosis that improves the prognosis of patients. It alleviates the economic burden
on the health systems that assume the financing of health programs.
CONCLUSIONS
This study shows that patients with greater functional impairment (functional class III and IV) mostly require combined therapy. Because they are more likely to be hospitalized even with a longer stay, a higher cost is generated not only due to the use of drugs but also due to the use of drugs due to hospital causes.
Authorship contributions: Fabián Hernández: Drafting the manuscript, conducting the
study, analyzing the results. Jéssica Nacazume, Julieta Larrosa: Study design, results report.
Óscar Aguirre, Nelson Larrea: Contributions to the discussion and conclusions of the study. Sara
Franco Watanabe, André Morais, Jorge Álvarez: Management of the study, final approval of the
manuscript.
Funding sources: The development of this study was funded by Janssen Pharmaceuticals.
Declaration of conflicts of interest: Dr. Oscar Aguirre has served as speaker for
Janssen, Nelson Larrea, Jorge Álvarez and André Morais are employees of Janssen
Pharmaceuticals.
Received: May 05, 2021
Approved: June 08, 2021
Correspondence: Fabián Hernández
Address: Calle 100 # 13 - 21, Bogotá DC, Colombia
Tolnahuac, Cuauhtémoc, 06920 Tolnahuac, CDMX – México.
Telephone: +57 316 5299829
E-mail: fabian.hernandez1@iqvia.com
BIBLIOGRAPHIC REFERENCES