ARTICULO ORIGINAL
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2021 - Universidad Ricardo Palma10.25176/RFMH.v21i3.3921
BILATERAL BREAST CARCINOMA IN VISCERAL CRISIS
CARCINOMA BILATERAL DE MAMA EN CRISIS VISCERAL
José M. Vela- Ruiz1,2,a, Diana I.Ferrer-Ponce2,b , Miguel J. Sotelo2,c , Reina Bustamante –Coronado 3,d , Nury León-Nué 4,e
1 Instituto de Investigación de Ciencias Biomédicas, Facultad de Medicina Humana, Universidad
Ricardo Palma, Lima- Perú.
2. Unidad de investigación Oncológica Hospital María Auxiliadora
3. Dirección de control y prevención de Cáncer – MINSA , Lima – Perú
4. Institución Liga Contra el Cáncer Lima-Perú.
a Médico residente oncología médica, Hospital María Auxiliadora, Lima, Perú, Miembro Comité del
Médico Joven Consejo Regional Lima - Perú.
b. Especialista en Oncología Medica, Coordinadora Servicio Oncología Médica Hospital María
Auxiliadora.
c. Especialista en Oncología Médica y Doctor en Ciencias Biomédicas.
d. Especialista en Oncología Quirúrgica mamas , piel y tejidos blandos , Maestría Gestión y
Servicios en Salud y Doctor en Medicina.
e. Especialista en Anatomo Patología.
ABSTRACT
Bilateral breast carcinoma is rare and infrequent , it is good to define if it occurs synchronously or metachronously, to define if the lesion in the second breast is metastasis or a primary tumor using pathological criteria, the state and clinical condition . For the prognosis and specialized treatment to follow. We present the case of a patient with ECIV breast cancer due to contralateral breast metastasis in a state of visceral crisis at debut, with pathological anatomy of grade 2 infiltrating ductal carcinoma of the breast, absent in situ component in both breast , RE (70%) , RP (80%), Cerb2 negative, Ki67 30% in the right breast and RE (100%) RP (80%) Cerb2-Ki67 20% left breast. A chest-abdomen-pelvis tomography was performed, showing pleural effusion. bilateral and large volume ascites. It was decided to start treatment with systemic chemotherapy, reaching a complete radiological and clinical response. After achieving good control of the disease, the first hormonal line will be sought.
Keywords: Infiltrating ductal breast carcinoma, contralateral metastasis, visceral crisis. (fuente: MeSH NLM).
RESUMEN
El carcinoma bilateral de mama es poco frecuente y raro, es bueno definir si ocurre de forma sincrónica o de forma metacrónica , definir si la lesión en la segunda mama es metástasis o un tumor primario usando criterios patológicos , el estadío y condición clínica . Ya que orienta en el pronóstico y tratamiento especializado a seguir. Presentamos el caso de una paciente con cáncer de mama ECIV por metástasis de mama contralateral en estado de crisis visceral al debut , con anatomía patológica de carcinoma ductal infiltrante de mama, grado 2, componente in situ ausente en ambas mama , RE(70%)RP(80%)Cerb2-,Ki67 30% en mama derecha y RE(100%)RP(80%)Cerb2-Ki67 20% en mama izquierda. Se realizó tomografía de tórax-abdomen-pelvis, evidenciándose derrame pleural bilateral y ascitis en gran volumen. Se decide iniciar tratamiento con quimioterapia sistémica alcanzándose respuesta completa radiológica y clínica. Tras conseguir buen control de la enfermedad se decidió iniciar primera línea hormonal.
Palabras Clave: Carcinoma ductal infiltrante de mama , metástasis contralateral , crisis visceral (fuente: DeCS BIREME).
INTRODUCCION
Breast cancer is the most common neoplasm in women and the 5th leading cause of death around the
world (1)
Bilateral breast cancer (BCC) has an incidence of approximately 0.7 to 1.8% (2, 3) and even in
other literature it is mentioned that there is a risk of presenting BCC of approximately 0.5% to 0.75%.
(4.5).
It is good to define if it occurs synchronously <1 year according to Heron, or
metachronously> 1
year, to define if the lesion in the 2nd breast is a metastasis or another primary cancer using the
Chaudary pathological criteria (6,7) .
We know that having a BCC have worse prognosis than unilateral breast cancer (8,9). All this is important both in the prognosis and
specialized treatment (9,10)
CASE REPORT
We present the case of a 48-year-old patient with no significant family oncological history, no relevant
pathological history, with a 2-year illness time characterized by asthenia and abdominal pain, who was
admitted by emergency due to exacerbated dyspnea, marked abdominal distention, whose preferential
physical examination revealed tumors in both breasts, both on the right side of approximately 5 x 5 cm
with an axillary ganglion more or less 2x2 cm with little hard motility, and a tumor in the left breast
measuring 5 x 5 cm without palpable ganglion. On examination of the chest and lung: decreased vesicular
murmur at the base with increased vocal vibrations, at the abdominal level a wave sign +, displaceable
dullness, in lower limbs edemas marked with fovea ++ / +++ was evidenced.
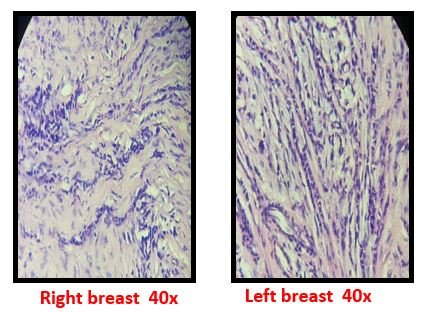
A biopsy of both breast lesions was performed, the result being in the right breast was
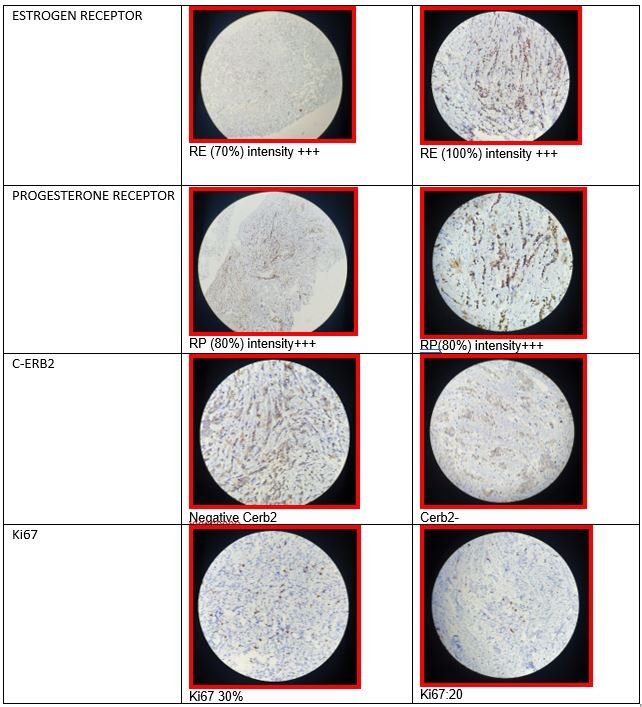
infiltrating ductal carcinoma of the breast, grade 2, component in situ absent with immunohistochemistry
in which the estrogen receptor (ER) + 70%, progesterone receptor (PR) + 80%, Cerb2 negative, Ki67 30%;
and in the left breast, infiltrating ductal carcinoma of the breast, grade 2, absent in situ component
with immunohistochemistry RE (100%) RP (80%) Cerb2-Ki67: 20% (Figure 2 y 3).
The emergency analysis showed hypoxemia due to AGA: pO2 55 mmHg, gauze ascites fluid study
(blood albumin / ascites gradient (GASA)) <1.1, negative ascites fluid PAP, leukocyte hemogram 5300 /
mm3 (neutrophils 43.2%) with rest of the hemogram, coagulation profile and biochemistry in normal
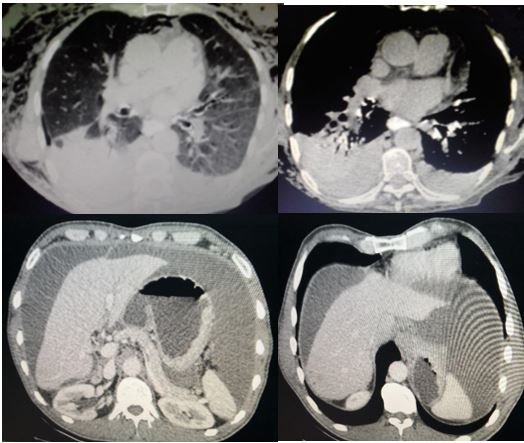
values, for this reason it was decided to perform a chest-abdomen-pelvis tomography, showing large
volume ascites and bilateral pleural effusion. (Figura 1)
Considering that the patient was found in visceral crisis at that time: respiratory failure,
ascites and massive pleural effusion and considering it a case of clinical stage IV infiltrating lobular
breast cancer due to contralateral breast metastasis according to the criteria of Chaudary et al., In
crisis state visceral, for which it is decided to start systemic chemotherapy of the 1st line Adriamycin
- Cyclophosphamide (Cyclophosphamide 600 mg / m2 and doxorubicin 60 mg / m2) 4 courses + 12 courses
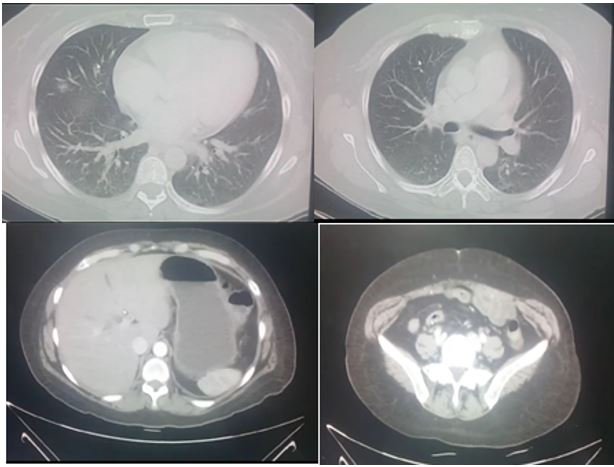
Paclitaxel (80mg / m2) weekly with contrast tomographic control chest, abdomen and pelvis (09-01-18):
showing complete remission of ascites, pleural effusion. (Figure
4).
Bone scan (GGO) 10/17/18: no evidence of metastatic disease. Clinically, there is a reduction
in tumor size in both breasts, remission of respiratory failure, and ascites. Being a luminal B patient:
she began treatment with tamoxifen on a palliative basis with stable disease at the time.
DISCUSSION:
48-year-old female patient, native and from Lima, with an illness time of approximately 2 years
characterized by asthenia and abdominal pain. Whoever is admitted as an emergency due to exacerbated
dyspnea, marked abdominal distention. On examination of the chest and lung: decreased vesicular murmur
at the base with increased vocal vibrations compatible with pleural effusion clinically, at the
abdominal level a wave + sign was evidenced, displaceable dullness compatible with ascites clinically,
in the emergency laboratory tests hypoxemia due to AGA and related to the respiratory condition already
described. Ascites fluid study (GASA) <1.1, negative ascitic fluid PAP, with this it should be
remembered that the serum albumin gradient - ascites: GASA, allows us to identify if the ascites is due
to portal hypertension or other causes. It is obtained by subtracting the value of serum albumin minus
the albumin of the ascites fluid from samples obtained on the same day. If it is higher than 1.1g / dl
it may be due to cirrhosis, cardiac ascites, Budd-Chiari syndrome or liver metastasis; if it is <1.1
g /
dl, it may be due to peritoneal carcinomatosis, peritoneal tuberculosis, nephrotic syndrome or
pancreatic ascites.
For all these reasons, it was decided to perform a chest, abdomen and
pelvic tomography with contrast, showing bilateral pleural effusion and marked ascites compatible
with the aforementioned symptoms. (Figure 1).
Preferential physical examination revealed tumors in both breasts both on the right side with
axillary ganglion present with little hard motility, and a tumor in the left breast without palpable
ganglion, which suggests that the suggestive symptoms could be due to a neoplastic process.
Therefore, it was decided to perform core biopsy in both breasts with the following histology:
infiltrating carcinoma, intermediate histological grade, infiltrating lobular carcinoma, ER +. RP +,
Cerb b2 -, Ki 67 left breast: 20%, Ki 67 right breast: 30% both absence of in situ component, and
negative cadherin, for which we are facing a case of: clinical stage infiltrating lobular breast cancer
stage IV due to metastases of the contralateral breast. We consider CS IV based on the pathological
criteria of Chaudary et al.
In bilateral breast cancer there is an incidence of approximately 0.7 to 1.8% (2, 4, 5). It is
good to define if it occurs synchronously <1 year according to Herón, or metachronously> 1 year, to
define if the lesion in the 2nd breast is a metastasis or 2nd primary cancer using the Chaudary
pathological criteria (6,7). We know that having a BCC is a
worse prognosis than unilateral breast cancer (8,9). All of
this is important both in the prognosis and specialized treatment (9,10).
We define whether it is really a metastasis or a second primary tumor using the Chaudary
criteria (7), which are summarized in 4 items:
- Which describes whether the lesion in the 2nd breast has an in situ component, makes us suspect a second primary cancer
- If we have a higher degree of differentiation, it is suggestive of a second primary cancer.
- If we have a different histology, let's think about a second primary cancer
- Last but not least: if we have similar histologies in both breasts and with the absence of locoregional or distant metastasis, it could indicate a second primary cancer
- In both breasts component in situ absent,
- Similar degree of differentiation in both tumors according to pathology
- Histology in both breasts as evidenced by a negative single row and cadherin pattern indicating invasive lobular carcinoma
- Faced with the fourth criterion, our patient presented a hard, non-mobile axillary adenopathy that inferred a probability of locoregional metastasis without even taking into account ascites and pleural effusion, which could be considered as distant metastasis
We show marked intensity estrogen receptors as evidenced in right breast (RB), left breast (LB), as well as similar progesterone + receptors in both breasts, negative cerb-b2 in RB and LB, ki67 30% in RB and 20% LB : cataloging Luminal B breast cancer
Our patient is in visceral crisis state because she presents an organ dysfunction characterized by signs, symptoms and laboratory tests (dyspnea, ascites, surge sign +, respiratory failure and hypoxemia demonstrated by AGA) that show marked clinical deterioration plus a visceral commitment, which forces us to act quickly and effectively (11).
Treatment depends on the clinical stage at the time of diagnosis. Considering a metastatic CS IV , it should be mentioned that in patients with hormone receptor (HR) positive metastatic breast cancer, starting chemotherapy before hormone therapy has not been shown to increase survival as evidenced in the Cochrane meta-analysis with studies by Dixon, Tashiro and Taylor in their respective investigations (12,13).
We have to take in consideration that currently in RH positive metastatic breast cancer the standard first-line treatment is hormone therapy + cyclin CDK 4-6 inhibitors, which has been shown to significantly prolong progression-free survival in this scenario.
With great examples such as the clinical benefit of palbociclib as initial therapy for postmenopausal women with estrogen receptor positive, epidermal growth factor 2 negative (ER +, HER2-) metastatic breast cancer, the phase 3 PALOMA-2 study demonstrated that the combination of palbociclib + letrozole vs letrozole improved disease-free survival of 24.8 months vs 14.5 months, showing a net benefit of 10 months HR 0.58 CI (0.46-0.72), it should also be noted that the combination of palbociclib and letrozole exceeded two years of PFS (progression-free survival), making it the best first line in this population of women. Benefit was also mentioned in the MONALEESA-7 study with hormone therapy + ribociclib with 23.8% vs 13.0% PFS HR 0.55 (0.44-0.69). (14, 15)
However, there is a scenario in which the probability of starting chemotherapy is indicated: only in the visceral crisis state according to the NCCN 2020 guidelines (12)
In our patient we started with 4 AC cycles and 12 weekly Paclitaxel cycles, showing disappearance of ascites and pleural effusion Figure 4 GGO, no metastasis was evident
In September 2018 we started with tamoxifen until now with good disease control
There is little evidence and reported cases of contralateral metastatic breast cancer at the time of diagnosis as debut, using the criteria of Chaudary et al., and that they have responded to chemotherapy as first line in a state of visceral crisis, prolonging their disease-free survival, which our work contributes to the scientific and academic literature.

|
CONCLUSIONS
It is important to differentiate between a second primary vs metastatic breast cancer due to the
respective prognostic and therapeutic implications.
In patients with metastatic RH + breast cancer, the standard treatment is hormone therapy + CDK
4/6 inhibitors according to the bibliography and guidelines.
Patients with visceral crisis are candidates for first-line treatment with CT.
There are few reported cases, it is necessary to deepen in more studies in breast cancer with
contralateral metastases.
Received: January 10, 2021
Approved: May 19, 2021
Correspondence: José M. Vela- Ruiz
Addres: Av. Benavides 5440, Surco – Instituto De Investigaciones En Ciencias
Biomédicas, Universidad Ricardo Palma
Telephone: 945322888
email: semaxxvr@gmail.com
BIBLIOGRAPHIC REFERENCES