CLINIC CASE
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2024 - Universidad Ricardo Palma10.25176/RFMH.v21i3.3923
FEOCROMOCITOMA: ENFOQUE MULTIDISCIPLINARIO, CONSIDERACIONES PERIOPERATORIAS
FEOCROMOCITOMA: ENFOQUE MULTIDISCIPLINARIO, CONSIDERACIONES PERIOPERATORIAS
Miryam Céspedes-Morón 1,a,b; Roxana Camargo-Román 2,b; Nicanor
Rodríguez-Gutarra3 y Alicia Mispireta-Castañeda4,c
1 Cardiovascular Anesthesiology and Intensive Care, Clínica Internacional. Lima, Peru.
2 Anesthesiology and Pain Therapy, Clínica Internacional. Lima, Peru.
3 Oncological and General Urological Laparoscopy, Clínica Internacional San Borja. Lima, Peru.
4 Clínica Internacional Lima, Peru
a MSc in Health Services.
b MSc in Medicine.
c Clinical Cardiologist, Echocardiographer
ABSTRACT
Patient scheduled for an adrenalectomy with laparoscopic technique, due to a tumor of the left adrenal gland. The diagnosis of chronic arterial hypertension was difficult to control, so a test was requested to rule out pheochromocytoma, resulting in a tumor of the left adrenal gland. The teamwork of the specialties involved in the care of the patient, effective communication, pre-surgical preparation and perioperative management, resulted in minimal perioperative complications in the patient, remaining in the intensive care unit for one day and reducing the hospital stay.
Keywords: pheochromocytoma; laparoscopic adrenalectomy; perioperative considerations (Source: MeSH Terms).
RESUMEN
Paciente programada para una suprarrenalectomía con la técnica laparoscópica, debido a un tumor de la glándula suprarrenal izquierda, su diagnóstico Hipertensión arterial crónica, se volvió difícil de controlar, por tal motivo se le solicita batería para descartar Feocromocitoma, resultando portadora de un tumor de la glándula suprarrenal izquierdo. El trabajo en equipo de las especialidades involucradas en el cuidado de la paciente, la comunicación efectiva, la preparación pre quirúrgica y el manejo periopertorio; dió como resultado que la paciente presentara mínimas complicaciones perioperatorias, permaneció en unidad de cuidados intensivos un día y se disminuyó la estancia hospitalaria.
Palabras Clave: feocromocitoma; suprarrenalectomía laparoscópica; consideraciones perioperatorias (Fuente: DeCS BIREME).
The purpose of this case presentation is to provide an analysis of the perioperative approach and effective communication between the surgical team before, during, and after surgery. Likewise, the perioperative considerations since the diagnosis was made, the preoperative treatment, the perioperative anesthetic considerations, and the surgical implications of pheochromocytomas, constitute a challenge for the anesthesiologist and the entire medical team. The multidisciplinary management allowed us to reduce complications and morbimortality; likewise, there are very few case reports of this pathology published in Peru; there is only one report of female patients more than 20 years ago, despite the fact that the incidence of this pathology is equal between men and women.
CLINICAL CASE
A 62-year-old female patient of mixed race, from the city of Lima, underwent laparoscopic left adrenalectomy for pheochromocytoma at the Clínica Internacional. She had no family history of tumor surgeries. As personal history she had hypertension for 4 years, dyslipidemia, and abdominal hysterectomy and breast biopsy.
Clinical picture: Patient presented headache, anxiety, palpitations, but no sweating, approximately 3 months before surgery. Her treatment was amlodipine 5 mg/day, losartan 50 mg/day, spironolactone 25 mg/day, hydrochlorothiazide 12.5 mg/day, and atorvastatin 10 mg/day. The patient was prepared 20 days before surgery; treatment was started gradually with alpha-blockers such as terazosin, until reaching a dose of 5 mg/day. Losartan was suspended when she presented hypotension during treatment; likewise, 5 days before the operation, she received beta-blockers such as atenolol 50 mg/day. After surgery, she required only the antihypertensive amlodipine 5 mg/day.
DIAGNOSTIC TESTS
Pre-surgical profile: hemoglobin 12.4g/dL, normal blood count, platelets 362,000, glucose 80mmHg, urea 31mg/dL, creatinine 0.70mg/dL, blood group O+, clotting time 7.30 minutes, bleeding time 2.15 minutes, plasma metanephrines 46.0 pg/mL, normetanephrines 180 pg/mL, urine metanephrines 0.25 mg/24 hours, metanephrines/creatinine ratio 0.28, 24-hour urine free catecholamines 65.0 ug/24h.
Chest X-ray: parahilar bronchiectasis in right hemithorax.
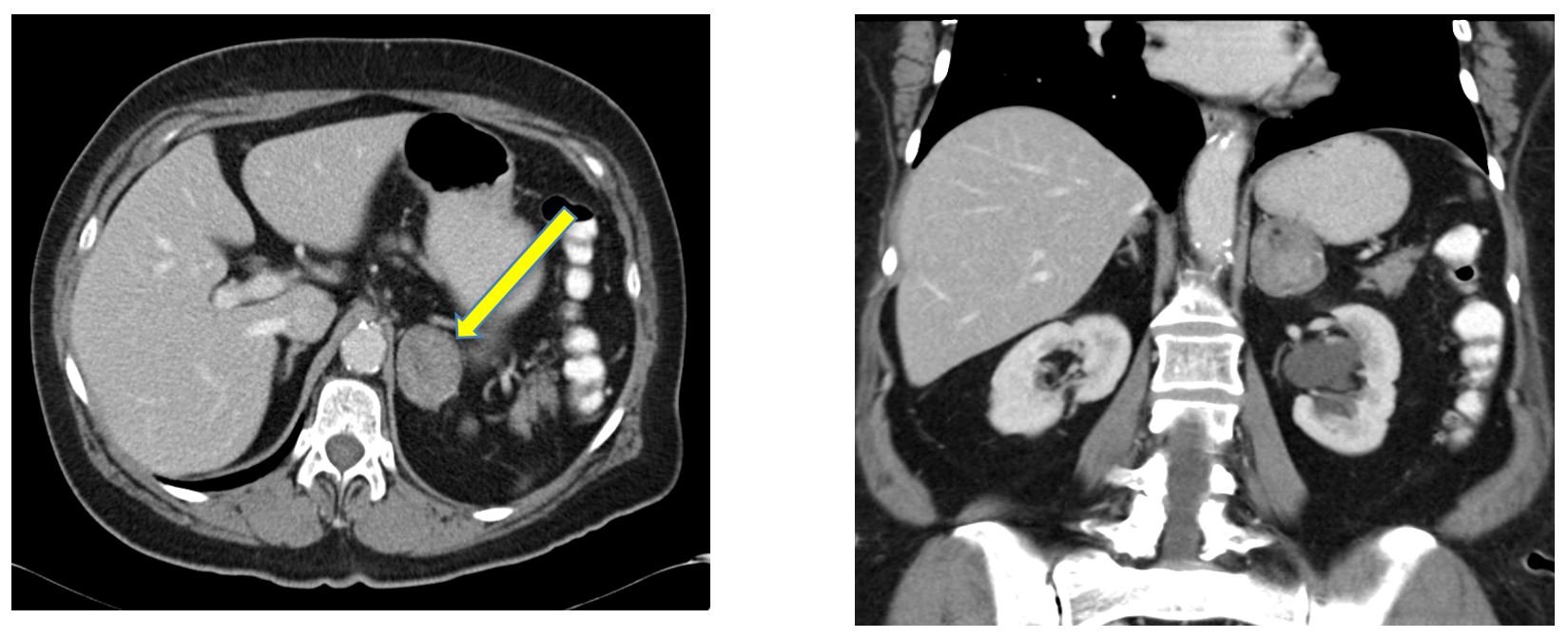
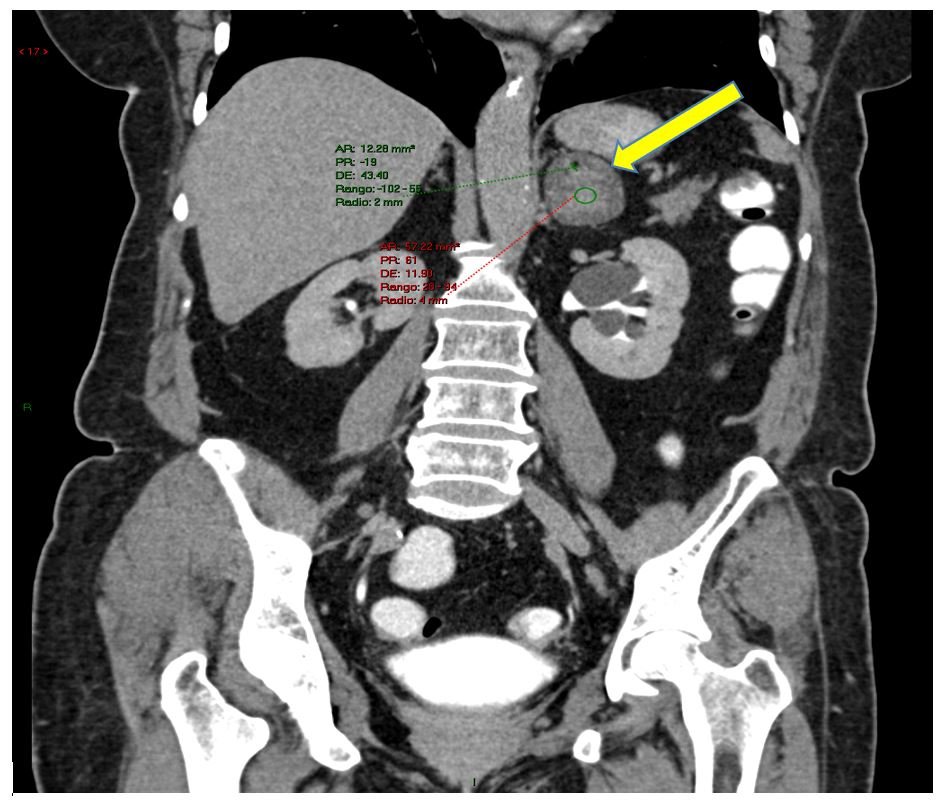
Multislice tomography of abdomen and pelvis: left adrenal gland, nodular morphology formation is observed, well-defined contours of 4 cm, major diameter, low density nodule measuring on average 10 HUH.
MRI: Heterogeneous expansive formation, dependent on the left adrenal gland, is replaced by a heterogeneous tumor with well-defined borders, with a larger diameter of 4.6 cm. There is no alteration of the peritumoral fat, nor infiltration of the underlying structures. After the contrast substance, heterogeneous enhancement, no infiltration.
Echocardiogram: EF: 60%. Diastolic dysfunction, mild LV hypertrophy predominantly septal, preserved systolic function.
Surgical risk: ASAIII. Intermediate Pneumological Risk.
Patient was evaluated in preanesthesia care unit, two days before the operation by the anesthesiologist. The patient signed the informed consent for anesthesia. When exploring the airway, Mallampati: II, good oral opening and cervical mobility, thyromental distance grade I, bite test class II.
Physical Examination: Skin and mucous membranes pallor, apparatus and systems within normal limits. The patient was hospitalized one night before surgery and was evaluated the day of surgery by the anesthesiologist on duty (second evaluation of anesthesia) who made the pre-anesthesia record. No premedication is indicated.
On the day of surgery, the patient enters the operating room with both informed consents, the specialized surgical one and the anesthesia one. She was monitored and an anesthesia checklist was performed. Monitoring was done with EKG (electrocardiographic monitoring), non-invasive blood pressure, oxygen saturation, capnography, intra-arterial catheter was placed to measure invasive blood pressure, and central venous catheter to measure central venous pressure. Anesthetic induction was then performed with fentanyl citrate 7 ug/kg, propofol 2 mg/kg, and rocuronium 0.6 mg/kg. Endotracheal intubation was performed without complications, nasogastric tube and esophageal thermometer were placed. She received balanced general anesthesia, maintained with remifentanil 0.50- 0.20 ug/kg/minute, ultra-short-acting opioid, and sevoflurane 1%. Intraoperatively, she required minimal doses of sodium nitroprusside 0.1- 0.2 ug/kg/min during gland manipulation, and two doses of phenylephrine 2- 3 ug/kg STAT after gland removal. Before extubation, sugammadex 2 mg/kg was administered to reverse the neuromuscular blockade. Intraoperative glycemia was measured twice in the operating room; the result was normal. For postoperative analgesia, multimodal analgesia was used with ketoprofen 1.5 mg/kg and tramadol 1 mg/kg.
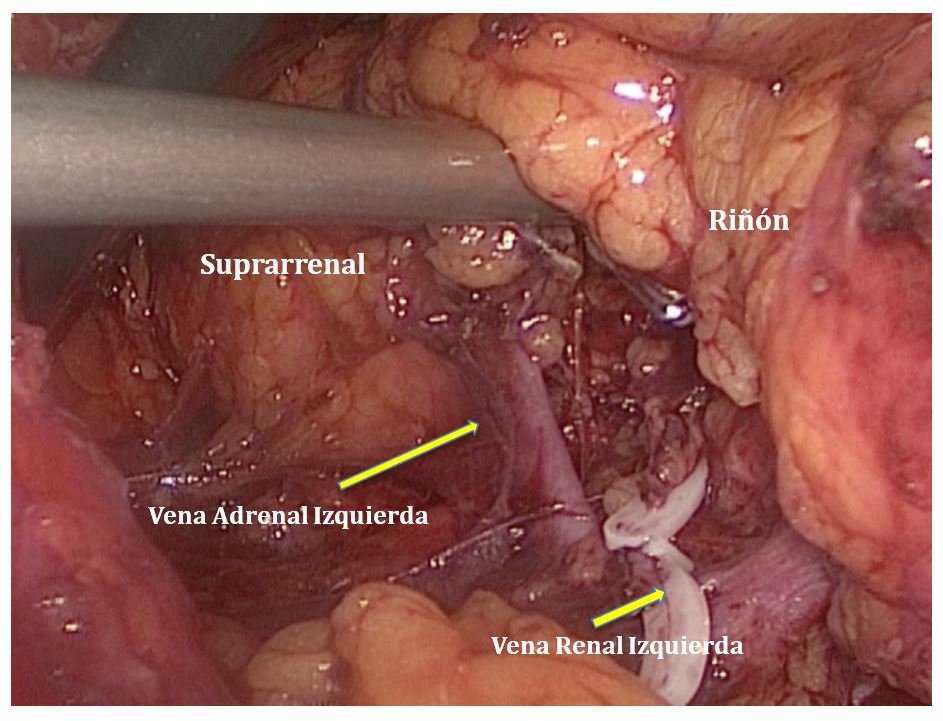
Before starting the surgical procedure, the second part of the checklist was performed; the technique used by the surgeon will be commented on in the discussion. Approximately after 2 hours, the surgery was finished and the last part of the checklist was performed. The patient is extubated without complications, goes to the ICU (intensive care unit) awake, calm, with stable vital functions and no pain.
In the immediate postoperative period, after 8 hours of her stay in the ICU, the patient presented hypoxemia, oxygen saturation 87%, and pulmonary congestion. She was treated with furosemide 20 mg/12; she also presented mild hyperglycemia. The patient remained stable and was discharged to her floor the following day. In hospitalization, she did not present any complications and was discharged two days later after presenting a favorable clinical evolution.
DISCUSSION
Pheochromocytoma is a rare neuroendocrine tumor derived from the embryonic neural crest, which produces catecholamines, mainly in the chromaffin cells of the adrenal medulla or in extra-adrenal paraganglioma chromaffin tissue (1,2,3). It has an incidence of 0.4 to 0.5 new cases per 100,000 in adults and occurs in 0.1 to 1% (4) of patients with arterial hypertension; our patient is included in this group. The literature reports that, of the pheochromocytomas discovered at autopsy, 75% died suddenly of myocardial infarction or cerebrovascular catastrophe; 1/3 of sudden deaths occurred during or immediately after a minor operation (1).
The patient's diagnosis included plasma fractionated metanephrines screening, a study that has a sensitivity of 98% for adrenal and 94% vs. 90% for extra-adrenal (5), as well as 24-hour urine metanephrines and catecholamines, with plasma normetanephrine being found at the upper limit. As for the localization diagnosis, computed axial tomography and magnetic resonance imaging (MRI) were used, where the left adrenal gland-dependent tumor was evidenced.
Preparation for surgery of patients diagnosed with pheochromocytoma should begin at least 2 weeks before surgery, to allow complete alpha-adrenergic blockade; this single precaution can decrease perioperative mortality from 43% to 3% (4). Pre-surgical preparation for pheochromocytoma surgery is essential for an optimal outcome, the standard protocol (6) is with phenoxybenzamine; it does not currently exist in the national market, but we do have others such as the selective alpha-antagonist terazosin, which was used in it and serves to prevent life-threatening cardiovascular complications, such as hypertensive crises, arrhythmias, myocardial infarction, and pulmonary edema. Five days before surgery, treatment with beta-blockers was initiated, which should not be started before a good alpha blockade has been achieved (7,8,9) and never in the absence of alpha-blockers. This is because it could cause an increase in catecholamine-induced vasoconstriction, unopposed deep alpha vasoconstriction, which may lead to hypertensive crisis or pulmonary edema.
From the surgical decision of the patient, there must be good communication and teamwork between the treating physician, in this case, cardiologist, with the specialized urologist surgeon and the anesthesiologist, before the patient is scheduled, to avoid suspensions of surgeries and prevent adverse events during the perioperative period. Likewise, it is very important that the anesthesiologist who will attend the patient is the one who evaluates her, identifies and assesses all additional risk factors, establishes the patient-physician relationship, or if she needs an interconsultation to another specialty, educates the patient, and explains the anesthesia procedure. These processes can be concretized with interprofessional care flows and care processes that are established in the institution.
Premedication, the night before or the day of surgery, is not part of our care protocols because of the risk of postoperative cognitive dysfunction. This is especially true in patients over 60 years, when adding the effects of anxiolytics or sedatives used to the effects of hypnotics used during anesthesia. Intraoperative considerations include avoiding factors that may trigger a hypertensive crisis (10), such as superficial anesthesia during tracheal intubation (4) and during surgery. We must be aware of all factors, such as tumor compressions, patient positioning, intraperitoneal insufflations of carbon dioxide, and during laparoscopy, direct manipulation of the tumor, which could trigger a hypertensive crisis. Similarly, avoid anticholinergic drugs such as atropine, sympathomimetics such as pancuronium bromide, drugs that release histamine such as morphine, atracurium besylate, and others such as droperidol, halothane, defluorane (2).
Pre-load was monitored by measuring central venous pressure, according to institutional guidelines. Other authors, such as (11), propose monitoring preload by measuring systolic volume variations in patients undergoing laparoscopic adrenalectomy. The anesthetic management was with balanced anesthesia, and the anesthetic induction was with moderate doses of opiate, to avoid pain response during endotracheal intubation, and propofol, which is a hypnotic with a protective profile for these patients. Likewise, it is advisable to have sodium nitroprusside ready because of the risk of catecholamine increase, as happened in this case during resection. An alpha vasoconstrictor such as Phenylephrine or Noradrenaline should also be available. In Peru, it is difficult to have access to phenylephrine drug because it is not commercialized; it has a potent alpha effect that causes immediate recovery from hypotension. This drug was available in the institution, therefore 2 boluses were applied and it was enough.
Peridural conductive anesthesia with catheter was used for laparotomies of suprarenalectomies and for postoperative pain control; it should be noted that its use is controversial because patients may present regurgitations or aspirations. In the case of laparoscopies, capnography must be obligatorily measured, therefore it is advisable to use balanced general anesthesia.
The laparoscopic technique has rapidly become the standard for the treatment of these tumors, however, this depends on the size of the tumor which must be < 6 cm (12). The laparoscopic approach is associated with shorter hospital stay, less use of analgesics, less postoperative pain, less hemodynamic effects, lower levels of circulating catecholamines, and less morbidity than laparotomies.
As for the treatment, a minimally invasive laparoscopic approach was used, since the tumor measured < 6 cm, the surgical technique used by the urologist was by transperitoneal access. He first dissected the mesocolon and Gerota’s fascia, identifying the gonadal vein up to the renal vein to facilitate access to it. He also avoided dissection of the adrenal gland before ligation of the vein, which must always be ligated first to avoid release of catecholamines. In that sense, he ligated the adrenal vein with 10mm Hem-o-lock, transected the adrenal vein, and performed the removal of the adrenal gland in a laparoscopic extractor bag.
Surgical resection is the mainstay of treatment, but patients are at risk of presenting many complications (13,14,15). The prognosis was favorable, there was no recurrence after two years of follow-up, the patient almost regularized her blood pressure, and currently continues to use minimal doses of antihypertensive medication.
Preoperative, intraoperative, and postoperative medical, pharmacological, and surgical management of pheochromocytoma constitute challenges for the medical team, which must be multidisciplinary and constitute the path to achieving a successful outcome.
CONCLUSIONS
An effective and timely communication between the surgeon, anesthesiologist and cardiologist, an adequate preoperative preparation, as well as the use of minimally invasive surgical techniques as described in the report and in the anesthetic techniques, result in minimizing perioperative complications and adverse events, improving the prognosis of patients requiring pheochromocytoma surgery. In our country, we need more scientific publications of patients with this pathology in order to standardize our care processes for the safety of our patients.
Authorship contributions:
All authors have
contributed to data collection and have participated
in the conception and design of the article.
Financing:
Self-financed
Declaration of conflict of interest:
The authors declare that they have
no conflicts of interest.
Recevied:
May 21, 2021
Approved:
July 9, 2021
Correspondence author:
Miryam Céspedes Morón
Address:
Calle Murillo 281 Dpto: 203 San Borja, Lima-Perú.
Phone:
998703847
E-mail:
miryamc18@hotmail.com
Article published by the Journal of the faculty of Human Medicine of the Ricardo Palma University. It is an open access article, distributed under the terms of the Creatvie Commons license: Creative Commons Attribution 4.0 International, CC BY 4.0 (https://creativecommons.org/licenses/by/4.0/), that allows non-commercial use, distribution and reproduction in any medium, provided that the original work is duly cited. For commercial use, please contact revista.medicina@urp.edu.pe.
BIBLIOGRAPHIC REFERENCES