REPORTE DE CASO
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2021 - Universidad Ricardo Palma10.25176/RFMH.v21i4.3956
CLINICAL PERFORMANCE OF A NEW PREDICTION RULE OF SYSTEMIC LOXOSCELLISM. CASE REPORT
RENDIMIENTO CLINICO DE UNA NUEVA REGLA DE PREDICCION DEL LOXOSCELISMO SISTÉMICO. REPORTE DE CASO
Rafael Pichardo-Rodriguez 1, 2; Marcos Saavedra-Velasco2; Cesar Sánchez-Alvarez3; Juan-Jesús Bracamonte-Hernández4; Abel Aldave-Visurraga5; Oscar Ruiz-Franco6
1. Instituto de Investigaciones en Ciencias Biomédicas (INICIB). Universidad Ricardo Palma,
Lima-Perú.
2. Centro especializado de enfermedades infecciosas, Lima, Perú.
3. Servicio de Enfermedades Infecciosas y Tropicales, Hospital Nacional “Dos De Mayo”-MINSA,
Lima, Perú.
4. Human Medicine student at Ricardo Palma University.
5. Servicio de Emergencia y Desastres, Hospital Nacional “Dos De Mayo”-MINSA, Lima, Perú.
6. Servicio de Hematología, Hospital Nacional “Dos De Mayo”-MINSA, Lima, Perú.
ABSTRACT
Systemic or cutaneous-visceral loxoscelism is the most severe clinical presentation of loxoscelism. Currently there is no validated laboratory diagnostic method that allows us to confirm the presence of this disease in the face of arachneism. However, there is a clinical prediction rule (CPR), which allows us to predict the evolution of a bite towards a systemic condition and which would be useful in emergency rooms. We present the case of a woman who developed the systemic picture of loxoscelism to whom a new CPR was applied for the early detection of systemic loxoscelism, presenting adequate performance for early evaluation in emergency services.
Keywords: Spider Bite, Hemolysis, Clinical Decision Rules (Source: MeSH NLM).
RESUMEN
El loxoscelismo sistémico o cutáneo-visceral, es la presentación clínica más severa del loxoscelismo. Actualmente no se cuenta con algún método diagnóstico laboratorial validado que nos permita confirmar la presencia de esta enfermedad frente a un aracneismo. Sin embargo, existe una regla de predicción clínica (RPC), que nos permite predecir la evolución de una picadura hacia un cuadro sistémico y que sería de utilidad en las salas de emergencia. Presentamos el caso de una mujer que desarrollo el cuadro sistémico del loxoscelismo a la que se le aplicó una nueva RPC para la detección temprana del loxoscelismo sistémico, presentando un rendimiento adecuado para la evaluación temprana en los servicios de emergencia.
Palabras Clave: Venenos de Araña, Hemólisis, Reglas de Decisión Clínica (Fuente: DeCS BIREME).
CASE REPORT
Systemic or cutaneous-visceral loxoscelism is the most severe clinical presentation of
loxoscelism(1). This is generated after a spider bite of the genus Loxosceles.
The pathophysiology is still unknown and is probably associated with a direct action of the venom on
tissues, mainly erythrocytes, causing complement-mediated intravascular hemolysis and probably
immunoglobulins, ultimately leading to acute renal failure and death (2,3). Treatment is based on the early application (within 12 hours) of antivenom
(anti-loxoscelic serum) and support measures (hydration, antibiotic therapy, corticosteroid therapy,
antihistamines, among others). (1).
Currently there is no validated laboratory diagnostic method that allows us to confirm the
presence of this disease in the presence of arachneism. Nevertheless, there is a clinical prediction
rule (CPR), which would allow us to predict the evolution of a bite towards a systemic condition, with
the drawback that it still requires external validation (4). Despite this, it
represents an important resource for emergency services, where it is necessary to make quick decisions
for the treatment of pathologies that may compromise the patient's life.
We present the case of a woman who developed the systemic picture of loxoscelism to whom a new
CPR was applied for the early detection of systemic loxoscelism, presenting adequate performance for
early evaluation in emergency services
CASE PRESENTATION
Past medical history and clinical presentation
A 21-year-old woman, with no significant medical history, went to the emergency service due to jaundice and a violaceous lesion associated with paresthesia at the level of the right iliac fossa (RIF). She refers two days before the admission, while dressing, feels a bite at the RIF level, seeing a spider fall and escaped through the clothes. After this, she presented fever (38.5 ° C), hemoglobinuria, jaundice and violation of the sting area, associated with decreased urinary volume.
CLINICAL EXAM
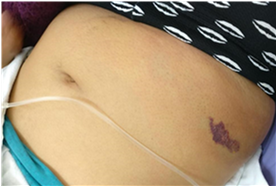
Examination revealed jaundice of the skin and mucosa and a violaceous lesion at the RIF level of approximately 7x4 cm with increased volume and heat, painful on palpation (see Figure 1).
|
LABORATORY RESULTS
The diagnosis of systemic loxoscelism associated with cellulitis is proposed and the pertinent laboratory tests and consultation with the infectology service are requested. The results are presented in table 1
Tabla 1. Laboratory test results
| Admition | Second day in emergency | |
|---|---|---|
| Hemoglobin (g/dL) | 14,2 | 12,9 |
| Lymphocytes (Lymphocytes /mm3) | 850 | 850 |
| Indirect bilirubin (mg/dL) | 4,02 | 3,2 |
| Urea (mg/dL) | 0,60 | 0,40 |
| Creatinine (mg/dL) | 31,52 | 26,54 |
| Rapid test for COVID-19 (IgG e IgM)* | Non reactive |
Spiders of the genus Loxosceles photos are presented to the patient, who recognizes its as responsible for the accident. The CPR elaborated by Pichardo-Rodriguez et al is applied, obtaining a score of 7, confirming the presence of a systemic condition with a specificity of 93.8%. table 2 shows the CPR for the prediction of systemic loxoscelism.
Table 2. Clinical prediction rule for predicting systemic loxoscelism.
| Variables | Score |
|---|---|
| Male gender | 2 |
| Threw up | 2 |
| Fever | 3 |
| Hemoglobinuria | 4 |
A score of ≥4 would indicate, with a sensitivity of 79.1% and a specificity of 93.8%, the presence of systemic loxoscelism.Source: R. Pichardo-Rodriguez, M. Saavedra-Velasco, J. Ascarza-Saldaña, C. Naquira-Velarde, Development and validation of a clinical prediction rule to identify systemic compromise in cases of loxoscelism, Mag. Fac. Med. Humana. 20 (2020) 1–1. https://doi.org/10.25176/RFMH.v20i1.2642.
Therapeutic interventions
It was decided to start antiloxoscelic serum (1 ampoule in 100ml of physiological saline), showing no adverse reactions to antivenom. Energetic hydration and antibiotic therapy are established (intravenous Oxacillin 2g every 6 hours).
Follow-up and result
The patient evolves favorably, recovering normal urinary volume. Infectology confirms the presence of a systemic Loxoscelism and her hospitalization is decided to continue the medical management.
DISCUSSION
The systemic picture of loxoscelism in our patient was adequately predicted using the CPR
elaborated by Pichardo-Rodriguez et al. The main limitation of this clinical tool is the absence of
external validation, however, in our case, it demonstrated adequate clinical performance to detect the
event in emergency department. The CPR is conformed by four variables: Male gender, vomiting, fever and
hemoglobinuria, with a respective score of 2, 2, 3 and 4 for each one (4). The
cut-off point for the score is 4, which predicts a sensitivity of 79.1% and a specificity of 93.8% for
the presence of a systemic picture of loxoscelism (4). Our patient had a score
of 7, confirming the presence of the disease. It is important to carry out prospective studies to
validate this tool in our population and evaluate its predictive capacity in emergency services or
primary care, as well as the inclusion of new predictors that allow us to improve its performance.
Systemic loxoscelism, unlike in our case, is more frequent in men. The association of the
systemic condition with the spider bite has been reported in the chest and abdomen, and this association
was found in our patient (5). The exact pathophysiology of the disease is
still unknown, but a direct action of sphingomyelinase D toxin on the surface of erythrocytes is
postulated with a direct complement interaction, the presence of erythrocytes covered with C3 as well as
those covered with antibodies has been reported. , sphingomyelinate D is probably a trigger for this
alteration (2,3). Paresthesias such as those presented by our
patient are part of the neurological compromise of loxoscelism, it has been found that some components
of the venom have direct action on the nervous system, causing symptoms such as paresthesia and in
animals causing damage to the choroid plexus and area postmas (6, 7). However, it has not been
associated with seizures.
Jaundice of the skin and mucosa associated with hemoglobinuria were clinical signs of the
presence of intravascular hemolysis, probably associated with renal tamponade that improved with
hydration, however, renal function tests remained within normal ranges (1).
Intravascular hemolysis is the most important alteration of systemic loxoscelism that subsequently leads
to tamponade and acute renal failure (1,3,4).
Therefore, it is relevant to start and continue with vigorous hydration in order to avoid kidney damage,
taking special care in those who cannot handle high intravascular volumes (heart failure, liver
cirrhosis, chronic kidney disease, among others) (1). Cellulitis is a frequent
finding in loxoscelism which was found associated in our patient (3).
Lymphopenia was a finding in our patient and its cause in loxoscelism is not fully understood,
however, it has been reported in pediatric patients (8). In a study where
Loxosceles Apachea venom was applied experimentally at different doses in rats, it was possible to
observe leukopenia, lymphopenia, neutrophilia and acantocytosis in peripheral blood (7). Loxosceles venom appears to be directly toxic to blood cells.
In relation to treatment, the specific intervention for loxoscelism is the application of
antivenom (4). There is still no evidence based on clinical trials or large
prospective cohorts that allow us to evaluate the safety and efficacy of this treatment, but early
application is recommended, if possible before 12 hours after the event occurred. There is still no
evidence based on clinical trials or large prospective cohorts that allow us to evaluate the safety and
efficacy of this treatment, but early application is recommended, if possible, less than 12 hours after
the event occurred. It is recommended to dilute a 5ml ampoule in a bottle in 100ml of physiological
saline in adults (1). There are no reports of adverse effects or anaphylaxis
to antivenom, and based on our experience, we have not observed adverse or anaphylactic reactions.
CONCLUSION
In conclusion, CPR present an adequate clinical performance predicting the systemic symptoms in patients with loxoscelism treated in emergency departments. External validation of this clinical tool is required, as well as prospective studies on systemic loxoscelism.
Authorship: The authors RPR, MSV, AAV participated in the study
conception, collection, analysis and data discussion. RPR, MSV, AAV, CSA and ORF participated in
the manuscript preparation, bibliographic search and approval of the final version of the
manuscript.
Financing: Self-financed
Declaration of conflicts of interest: No conflicts of interest are declared
received: June 04, 2021
Approved: July 11, 2021
Correspondence: Juan-Jesús Bracamonte-Hernández
Address: Calle Julio Mini Rivas 281 Urb. San Amadeo de Garagay, San Martin de
Porres, Lima.
Cellphone: 997473135
Email: juanjesus.bracamonte@gmail.com
REFERENCES
