REPORTE DE CASO
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2021 - Universidad Ricardo Palma10.25176/RFMH.v21i4.3985
PARAPHARYNGEAL SCHAWANNNOMA.CASE REPORT
SCHWANOMA PARAFARINGEO
Enrique Moyano Navarro1,a, Manuel Inostroza Fernández1,a, Pedro Sotelo Jiménez1,a, Ethel Vargas Carrillo2,b, Alan La Torre Zúñiga1,c, Luis González Domínguez1,d
1 Hospital Nacional Edgardo Rebagliati Martins – Essalud – Lima- Peru.
a Assistant Physician in Internal Medicine.
b Resident Physician in Internal Medicine.
c Assistant Physician of Pathology.
d Assistant Physician in Maxillofacial Surgery.
ABSTRACT
Parapharyngeal tumor lesions present a low incidence, representing between 0,5 and 0,8% of all head and neck tumors. Approximately 80% show benign behavior. The uniqueness of these lesions derives from their complex anatomical situation and the symptoms with which they usually appear, being in most cases nonspecific and almost always derived from the compressive effect produced by the lesion on the oropharynx and the oropharynx. Schwannomas of the parapharyngeal space are very rare tumors that originate from the sheath of schawnn, generally slow growing, and are usually asymptomatic. Treatment is surgical, often complex due to the anatomical location.The case of a 42-year-old female patient with a diagnosis of Schwannoma in the left parapharyngeal region, demonstrated by incisional biopsy, is presented; undergoing surgical treatment, which was carried out without complications.
Keywords: Parapharyngeal space; Schwannoma (source: MeSH NLM).
RESUMEN
Las lesiones tumorales de localización parafaríngea presentan una escasa incidencia, representando entre el 0,5 y el 0,8% de todas las tumoraciones de cabeza y cuello. Aproximadamente el 80% presentan un comportamiento benigno. La singularidad de dichas lesiones deriva de su compleja situación anatómica y de la clínica con la que suelen debutar, siendo en la mayoría de los casos inespecífica y casi siempre derivada del efecto compresivo producido por la lesión sobre la oro y rinofaringe. Los Schwannoma del espacio parafaríngeo son tumores muy infrecuentes, que se originan de la vaina de schawnn, generalmente de crecimiento lento, suelen ser asintomáticos. El tratamiento es quirúrgico, muchas veces complejo por la localización anatómica. Se presenta el caso de una paciente femenina de 42 años de edad con diagnóstico de Schwannoma en la región parafaríngea izquierda demostrada mediante biopsia incisional; realizándosele tratamiento quirúrgico, el cual se llevó a cabo sin complicaciones.
Palabras Clave: Espacio parafaríngeo; Schwannoma (fuente: DeCS BIREME).
INTRODUCTION
Schwannomas are the second most frequent tumors located in the parapharyngeal space. Although most of
these tumors are found in the head and neck, those with an extracranial location only constitute 10% of
the total(1). Parapharyngeal tumor lesions present a low incidence,
representing between 0.5 and 0.8% of all head and neck tumors(1,2). Approximately 80% show benign behavior(2-4).
The uniqueness of these lesions derives from their complex anatomical situation and the symptoms with
which they usually appear, being in most cases nonspecific and almost always derived from the
compressive effect produced by the lesion on the oropharynx and rhinopharynx, presenting symptoms such
as dysphonia, compressive pain or pharyngeal mass.Secretory paraganglioma, although uncommon, can cause
hypertension, sweating, nausea, palpitations or headache(3) These are usually
tumors that affect adults, without differences between the sexes and are mostly benign.
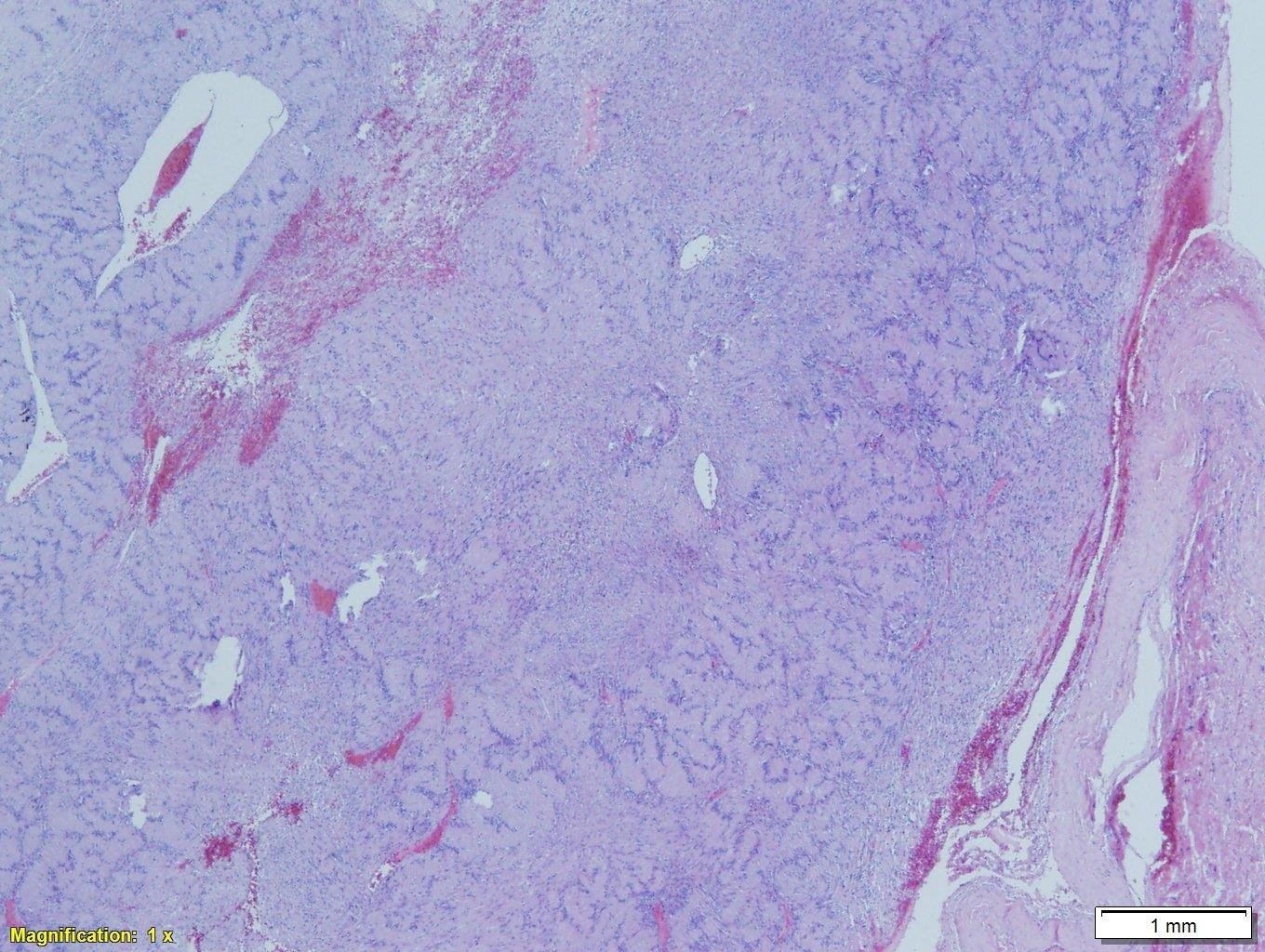
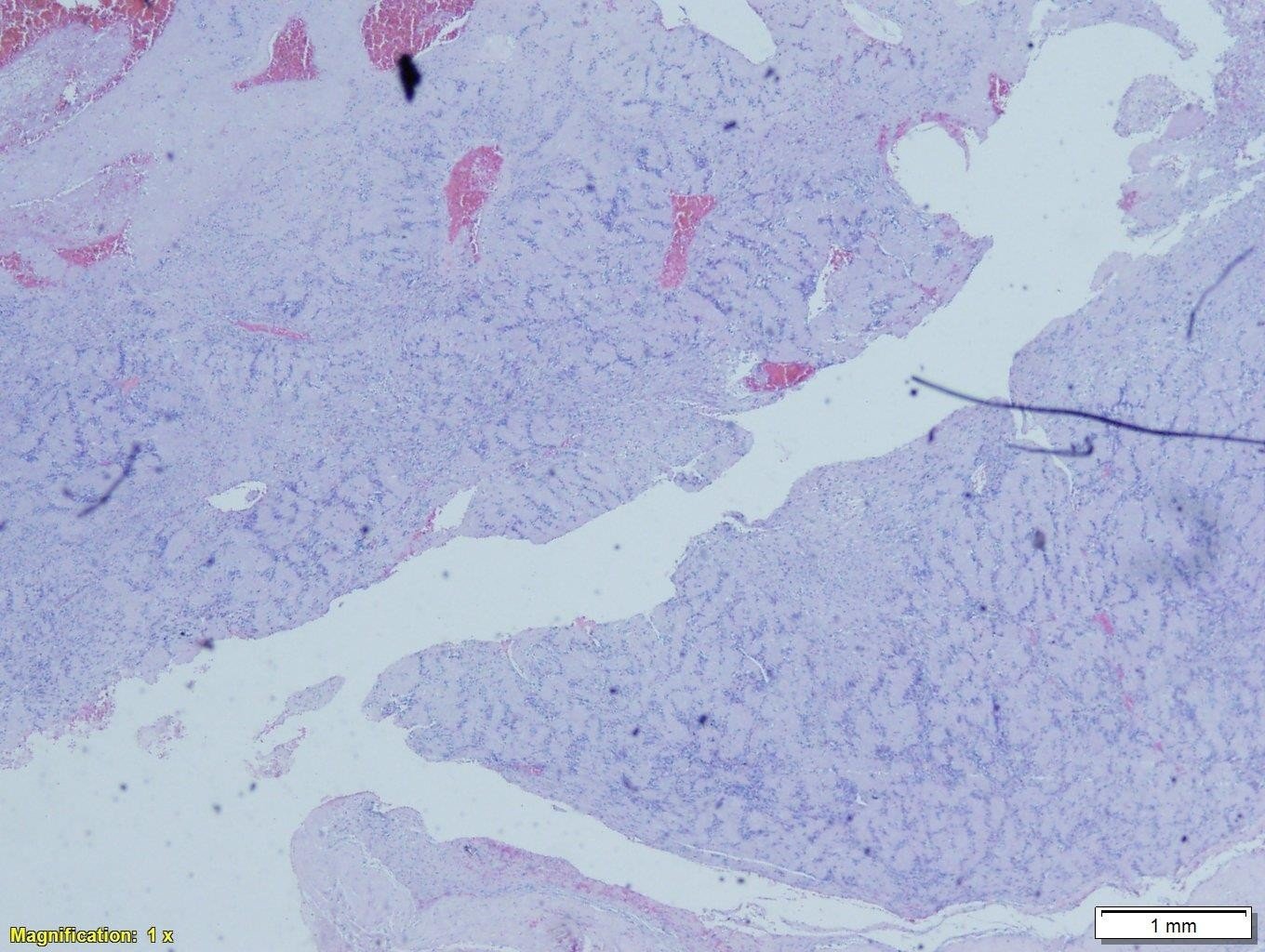
The pathological study of the tumor reveals a well encapsulated mass made up of spindle cells
type A of Anoni and type B of Antoni, the immunohistochemistry shows an intense expression of the S-100
protein(5).
The prognosis for a person with schwannoma is excellent when the mass has been completely
removed. Local recurrence is infrequent, being related to incomplete exegesis of the neoplasm(6,7).
CLINICAL CASE
42-year-old female patient with a 20-year history of migraine. She presented to the Internal Medicine service of the Hospital Edgardo Rebagliati Martins in Lima, Peru, reporting a 2 months disease of progressive onset and characterized by hemicranial and left mandibular headache, of moderate intensity, accompanied by increased volume in the cervical region on the same side; also, mild odynophagia and dysphonia. Physical examination revealed a mass of approximately 5 cm in diameter in the left maxillary region, not adhered to deep planes, with non-hyperthermic surrounding skin and no color changes, nor fixed to deep planes, on bimanual manipulation it was discreetly painful on palpation. shallow and deep. Given the suspicion of an expansive parapharyngeal process, an imaging study was carried out using a Cervical Tomography with contrast (Figure 1), where a large solid left parapharyngeal mass with heterogeneous contrast enhancement and areas of peripheral calcification measured TD 38mm DL 50mm DBH 40mm , and that extends cranially towards the jugular foramen and displaces the cervical vascular structures anteriorly, without infiltration; causes mass effect with airway compression. In addition, a nuclear magnetic resonance study was performed (Figure 2, Figure 3), where it shows a solid image with well-defined edges, an ovoid shape in the left parapharyngeal space, exerting an expansive effect and moving the midline from left to right. Intramedullary extension is not observed. Subsequently, a BAAF was performed with ultrasound guidance of the lesion, the result of which was not conclusive for the diagnosis, which is why the case was reassessed, deciding to take an incisional biopsy by the Head and Neck Surgery Service, which was sent to histopathological study; Schwannoma was reported, being transferred for surgical treatment definitive; A cervical approach was used (Figure 4, Figure 5), and the surgical specimen was sent for histopathological study, the result of which confirmed our initial diagnosis: Parapharyngeal Schwannoma



DISCUSSION
Parapharyngeal space tumors account for 0.5% of all head and neck neoplasms (2). Most of the lesions located in this space are benign primary tumors that
originate from the vagus nerve, the most common being the schwannoma. Schwannoma is the most common
histologic subtype of vagus nerve tumor after paraganglioma. It usually appears between the third and
sixth decades of life, being more frequent in young adults (5), presenting a
similar frequency in both sexes. (3). Clinically without symptoms, it is
diagnosed as a unilateral laterocervical mass mobile only in a solitary lateral direction, except in Von
Recklinghausen's disease (6,8) and in a rare syndrome known as
schwannomatosis (24) where the presentation is multiple. They can be palpated
as masses on the medial border of the sternocleidomastoid muscle. Its expansive growth through the
parapharyngeal space can make it go unnoticed to a large size. If its size is considerable, it can cause
very nonspecific signs such as pharyngeal paresthesia, cough, odynophagia due to pharyngeal compression,
dysphonia. A characteristic, although not always present, clinical sign of cervical vagal schwannoma is
paroxysmal cough on palpation of the tumor and even serous otitis (5,6,9). Symptoms derived from compression of nerve structures IX,
X, XI, XII, of the sympathetic will be seen in cases of large neurinomas, or in malignant tumors and
chemodectomas. Pain, trismus, and cranial nerve lesions suggest malignancy.
The diagnosis will be based on the clinic, the physical examination, being important the
bimanual palpation, which allows to recognize the continuity of the tumor and determine its origin.
Oropharyngeal and oral cavity visualization is important to rule out other primaries in these locations
that could be producing secondary metastatic involvement in the parapharyngeal space. A pulsatile
cervical mass may indicate the presence of a vascular tumor, such as a paraganglioma. The physical
examination should include an examination of the cranial nerves and the performance of a flexible
nasopharyngolaryngoscopy (2).
The radiological study using Computed Tomography (CT) and Magnetic Resonance (MRI) will be of
vital importance. On CT, they are tumors with a density similar to the muscle, more less rounded and
well defined with a medial and lateral fatty plane, as their most frequent origin is the X pair or the
sympathetic chain, they usually displace the internal carotid artery anteromedially. MRI provides
excellent information in the study of soft tissues, being very useful in this type of tumors and that
region,they are hypointense tumors on T1 and hyperintense on T2 and on T1 with gadolinium. Differential
diagnosis should be made with carotid artery aneurysm, with neurogenic tumors of cranial nerves IX, X,
XI and XII or of the cervical sympathetic plexus (14), with paraganglioma,
meningioma, lymphoma and teratoma (15) However, the majority of lesions
involving the retrostyloid parapharyngeal space are peripheral nerve sheath tumors, head and neck
paragangliomas, or metastatic lymphadenopathy (24).
The performance of FNAB in tumors of the pararaphinx can reach 86% - 99% especially in lymphoma,
primary malignant tumors or metastases of malignant tumors (22,24). However, FNAB would not be helpful in distinguishing benign from
malignant paragangliomas or benign from malignant peripheral nerve tumors. As in our case, it was not a
contribution for diagnosis.
The macroscopic examination usually corresponds to a white, yellowish, well-defined mass with a
firm and elastic consistency, sometimes with cystic areas. being typical the presence of necrosis,
hemorrhage and intratumoral cystic degeneration (23). From the microscopic
point of view there are two groups: Antoni A, a compact cellular composition in palisade and Antoni B,
formed by a loose structure characterized by myxoid degeneration, although most of the time they are
associated, while others defend that hemorrhage it is responsible for vacuolar degeneration due to
hemosiderin deposition. Immunohistochemical techniques show an intense expression of the S-100 protein
in these tumors, an antigen of the tissues derived from the neural crest (20, 21).
The treatment is surgical, although due to the infrequent presentation of tumors in this
location it is difficult to obtain surgical experience, there are different approaches, which will
depend on the size and location of the tumor, the most used being the cervical route, suitable for most
tumors, in larger cases or for tumors of pre-style location, the cervico-parotid approach can be useful.
The most frequent complications in surgery are injury to the nerve itself and its resulting deficit.
Recurrences are rare and are usually the result of incomplete excision, generally having a good
postsurgical prognosis. Regarding the prognosis, in cases of benign tumors, when a complete resection is
achieved, the risk of recurrence should be low to null.
Authorship contributions: The authors
participated in the genesis of the idea, project
design, data collection and interpretation, analysis
of results, and preparation of the manuscript of this
case report.
Financing: Self-financed.
Conflicts of Interest: The authors declare that they
have no conflict of interest.
Received: July,19 2021
Approved: August 18, 2021
Correspondence: Javier Enrique Moyano Navarro
Address: Av. Rebagliati s/n – Jesús María- Lima-Perú
Telephone: 999025042
E-mail: enriquemoyano_ica@hotmail.com
BIBLIOGRAPHIC REFERENCES
