ARTICULO ORIGINAL
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2021 - Universidad Ricardo Palma10.25176/RFMH.v22i1.4095
DECREASE OF CARDIOVASCULAR RISK IN OBESE PATIENTS WHO PARTICIPATED IN A LIFESTYLE MEDICINE PROGRAM
DISMINUCIÓN DEL RIESGO CARDIOVASCULAR EN PACIENTES OBESOS QUE PARTICIPARON EN UN PROGRAMA DE MEDICINA DE ESTILO DE VIDA
Eymard Torres-Rodriguez1,a, Lucy Cedillo-Ramirez2,b
1Internal Medicine Specialist in Nutrition, Diabetes, Metabolism and Lifestyle Medicine
2Medical surgeon.
aLifestyle Medicine SAS- IPS, Cartagena Colombia
bLatin American Lifestyle Medicine Association. Lima, Peru
ABSTRACT
Lifestyle Medicine in the management of chronic diseases such as obesity is essential to reduce cardiovascular risk and to reverse the disease process (1). Objective: To determine if a Lifestyle Medicine program can reduce cardiovascular risk in obese adults in Colombia. Material and methods: Descriptive observational study cases series type followed for 6 months in a Lifestyle Medicine Clinic. 9 patients were included taking into account 2 measures of cardiovascular risk as a parameter to complete the program. The following measurements were taken: cardiovascular risk using the Pan American Health Organization (PAHO) calculator, Body Mass Index (BMI), lipid profile, history of smoking, history of diabetes, and systolic blood pressure. Results: Of the 9 obese patients, 22% had an intermediate cardiovascular risk and 78% had a low risk at the beginning of the study. After 6 months, it was achieved that 100% of the participants had a low cardiovascular risk; Furthermore, 11% of the patients managed to normalize their blood pressure values and 20% showed a decrease in high blood pressure values. In addition, 22% went from type 3 obesity to type 2 obesity. Finally, through psychological consultation, it was possible to reduce anxiety levels from high to intermediate in at least 44% of the participants. Conclusions: The Lifestyle Medicine program, in a group of obese patients, managed to achieve a low cardiovascular risk, the decrease and normalization of blood pressure figures and reduction in BMI in participants who completed the study.
Keywords: Obesity, cardiovascular diseases, lifestyle, comorbidity, essential hypertension, diabetes mellitus(fuente: MeSH NLM).
RESUMEN
La Medicina de estilo de vida en el manejo de enfermedades crónicas como la obesidad, es fundamental para disminuir el riesgo cardiovascular y para revertir el proceso de enfermedad (1) . Objetivo: Determinar si un programa de Medicina de Estilo de Vida logra disminuir el riesgo cardiovascular en adultos obesos de Colombia. Material y Métodos: Estudio observacional descriptivo tipo serie de casos seguidos por 6 meses en una Clínica de Medicina de Estilo de Vida. Se incluyeron 9 pacientes teniendo en cuenta 2 medidas del riesgo cardiovascular como parámetro para completar el programa. Se tomaron los siguientes mediciones: el riesgo cardiovascular mediante la calculadora de la organización panamericana de la Salud (OPS), Índice de Masa Corporal (IMC), perfil lipídico, antecedentes de tabaquismo, antecedentes de diabetes y presión arterial sistólica. Resultados: De los 9 pacientes obesos, el 22% tuvo un riesgo cardiovascular intermedio y 78% presentaron riesgo bajo al inicio del estudio. Luego de 6 meses, se logró que el 100% de los participantes tuvieran un riesgo cardiovascular bajo; además, el 11% de los pacientes lograron normalizar los valores de presión arterial y un 20% evidenciaron disminución de valores elevados de presión arterial. Además, el 22%, pasaron de obesidad tipo 3 a obesidad tipo 2. Por último, mediante la consulta psicológica se logró disminuir los niveles de ansiedad de alto a intermedio en al menos el 44% de los participantes. Conclusiones: El programa de Medicina de Estilo de vida, en un grupo de obesos, logró disminuir el riesgo cardiovascular, logrando la disminución y normalización de las cifras tensionales y la reducción del IMC en los participantes que concluyeron el estudio.
Palabras Clave: Obesidad, enfermedades cardiovasculares, estilo de vida, comorbilidad, hipertensión esencial, diabetes mellitus (fuente: DeCS BIREME).
INTRODUCTION
In the last publication of the American College of Cardiology, where they studied the worldwide rates of cardiovascular disease from 1990 to 2019, they concluded that prevalent cases of cardiovascular diseases (CVD) almost doubled from 271 million (interval of uncertainty [IU] of 95%: 257 to 285 million) in 1990 to 523 million (IU of 95%: 497 to 550 million) in 2019, and number of deaths from CVD increased constantly from 12,1 million (95% IU: 11,4 to 12,6 million) in 1990, reaching 18,6 million (95% IU: 17,1 to 19,7 million) in 2019, concluded that the cardiometabolic, behavioral, environmental and social risk factors are the main promoters of cardiovascular diseases. Among the main risk factors and behaviors for developing cardiovascular disease in the general adult population, we found arterial hypertension and obesity at 45.9% and 39.6%, respectively (2).
In Colombia, the Non-Transmissible Chronic Diseases (NTCD) also represent the main cause of death. These diseases represent a true epidemic that increases due to population aging and current lifestyles that emphasize sedentarism and poor diet (3).
Obesity is strongly associated with a greater risk of cardiovascular mortality, all-cause mortality and mortality due to cancer (4). . On the other hand, decreasing at least 1 kg of weight reduces the possibility of developing type 2 diabetes by 16% (5) , and if the weight loss is greater or equal to 5% from the initial weight, we could reach a moderate improvement in arterial pressure, low density lipoprotein cholesterol (LDL-C), triglycerides, and glucose levels in overweight or obese people, hence reducing their cardiovascular risk (6).
A great amount of scientific and medical literature exists that supports the concept that habits, and daily actions have an enormous impact on health and short and long-term quality of life (7). This impact can be positive or negative. Diverse studies offer evidence that regular physical activity, maintaining a healthy body weight, not smoking cigarettes, and following solid nutrition habits and health promotion deeply influence health. These aspects are part of the fundamental pillars of which Lifestyle Medicine is based. This approach was created from the need of studying how daily habits and practices impact disease prevention as well as treatment, often together with pharmaceutical or surgical treatment, to offer an important complement to health in general. (8)
Adherence to a healthy lifestyle during one’s entire life i sable to significantly reduce cardiovascular risk up to 70%, and, therefore, it is a key component in the primary prevention of cardiovascular diseases (9). With an adequate nutritional plan, guided by an interdisciplinary team, we may be able to reach a decrease of 8 to 14mmHg, knowing that each decrease of 10mmHg in systolic arterial pressure, significantly lowers the risk of any cardiovascular disease occurrence (10).
There have been intensive programs carried out in Latin America that cover Lifestyle programs(11), however, we have not had the experience of a similar program applied to patients with obesity in Colombia.
Lifestyle Medicine in Colombia is currently represented by the Asociación Colombiana de Medicina de Estilo de Vida (AMESVIDA) and in Latin America by the Latin American Lifestyle Medicine Association (LALMA). The implementation of lifestyle medicine programs has been developing in Colombia through some health institutions whose objective was to implement strategies and programs to revert diabetes in the Colombian health system, as a first experience (11). However, efforts for promotion of Lifestyle Medicine intervention programs in the medical practice are needed for the purpose of preventing and treating different chronic and metabolic diseases. This is why, this research seeks to determine if a decrease in cardiovascular risk exists in an obese population that participates in a Lifestyle Medicine program in Colombia.
MATERIAL AND METHODS
Study design
Observational, descriptive, case series type study. The data was obtained from the medical history of patients seen in outpatient medical consult and who were included in the Lifestyle Medicine program, this data was consigned in a data collection sheet where age, body mass index (BMI), blood pressure values, complete lipid profile values were included, from which the 10-year cardiovascular risk was obtained. The before-mentioned data were measured at the beginning of the program (first month) and at the end (sixth month).
Population and sample
The population was made up of obese male patients who were seen at a Clínica Lifestile Medicina SAS to participate in a Lifestyle Medicine program between July and December 2019. A total of 13 patients with obesity participated, however, 9 patients were considered for the study, since they were the only ones who completed the intervention program. Since this study is a follow up of a case series presented in a private institution, it was not necessary to calculate sample size.
Inclusion and exclusion criteria
The study’s inclusion criteria were patients who attended at least two consultations during the program that lasted 6 months, and whose BMI was greater or equal to 30, history of arterial hypertension, diabetes mellitus and high lipid levels. We excluded the participants who did not complete the program or who only had one measure during the time of the study.
Variables
Through national and international literature review, the following variables were included: sociodemographic factors (age), obesity measured through Body Mass Index according to staging proposed by the World Health Organization – WHO, blood pressure (categorized using the American Heart Association classification – AHA), total cholesterol, LDL cholesterol, bioimpedance measurement (corporal composition study with the inbody 120 equipment) and cardiovascular risk determination, which was obtained from the Pan American Health Organization calculator (PAHO), which include the following dimensions: sex, age, smoking, diabetes, maximum systolic blood pressure (SBPmax), maximum diastolic blood pressure (DBPmax). All the variables mentioned were measured at the beginning and end of the study. This calculator was used since it was standardized for the Colombian population and for the easy access for health professionals in the measure of variables that take part in determining cardiovascular risk.
Procedure
A data collection sheet was used as an instrument. With the data collected during hte first as well as the last consultation, an Excel spreadsheet data base was created. This base was processed in the statistical program SPSS V.25 for its analysis. The information was obtained through review of medical history. The Lifestyle Medicine program was guided by an internal medicine physician specialized in nutrition and Lifestyle Medicine, who worked together with a team of medical specialists.
The Lifestyle Medicine program that was developed consisted of a personalized medical attention through the application of the 6 pillars of Lifestyle Medicine: 1) plant based nutrition free of ultra-processed foods: the activity was under the care of a nutrition specialist, who in addition to giving advice to participants, offered a list of ultra-processed products that the patients should avoid consuming, additionally, in the assessment by the nutrition/dietitian specialist the patients were told the healthy plate method referred to plant based nutrition;2) daily physical activity: in the consultation we prescribed physical activity of 30 minutes daily including, rapid walks, associated to resistance exercises;3)adequate daily rest: 8 hours of night sleep was prescribed, we also gave sleep hygiene recommendations such as how to avoid watching television in the bedroom, how to avoid stimulating drinks 2 hours before bedtime, avoiding the use of electronic devices during bedtime and keeping at least 3-4 hours of fasting prior to going to sleep; 4) stress control: a specialist taught the participants to practice a few techniques on how to face stress, based on behavioral cognitive therapy in a personalized and group format, furthermore, participants’ stress levels were measured through a perceived stress software specialized in stress and anxiety classification (PSS) 12; 5) avoid harmful substances such as alcohol and tobacco use, among others; 6) having a solid family and professional companionship system through the program: promoting family awareness, through group sessions about the importance of practicing Lifestyle Medicine with the aim of making them an effective support for the patients in the process of healthy activity selections. Furthermore, in the first consultation, the bioimpedance measurement, anthropometry (BMI), blood pressure control, and laboratory studies, which measure the initial levels of total cholesterol and LDL cholesterol, were taken.
Each time the participants went for their assessment by the health professional, a record of their prescribed activities was carried out with the purpose of controlling the activity compliance. The patient follow-up was done in person during consultations and evaluations indicated during the program, but we also followed-up by telephone during the 6 month duration of the program. Finally, in addition to basal measurement of the aspects mentioned in the beginning of the follow-up (first month), another one was carried out at the end of the program to compare and describe results evidenced in the patients.
Statistical analysis
The SPSS V.25 statistical software was used for the statistical analysis. The data was evaluated through descriptive statistics, using frequencies percentages, central tendency and dispersion method measures. The results were presented comparatively in tables and bar graphs.
Ethical considerations
For the study development, we considered the anonymity of personal data, for the data base used as well as for the information collection. Likewise, in order to include patients in the Lifestyle Medicine program we asked for the informed consent. Furthermore, the study was approved by the Medical Ethical Committee of the institution
RESULTS
The following are the results obtained in the evaluations by the medical team trained in lifestyle medicine. An initial report and a final report was presented at the end of the program. All the participants were obese male Colombians, with an average age of 51 years, average weight of 109 kg approximately. 33% of obese patients had dyslipidemia ad did not receive treatment, furthermore, 33% of patients had hypertension and were under treatment with antihypertensive medication. None of the participants smoked tobacco and only one of them had diabetes as personal history at the moment of initial evaluation and he was under pharmacological treatment.
We evidenced an intermediate Cardiovascular Risk (CVR) in 22.2 % of participants at the beginning of the study, after 6 months in the lifestyle medicine program, 100% of the study subjects were able to have a low CVR of developing cardiovascular disease in 10 years. Regarding obesity, 22% of total patients had obesity type 3 at the beginning of the study, after a 6 month follow up and at the end of the study none of the subjects had this type of obesity. As far as blood pressure measurements, 100% of participants had some level of arterial hypertension (elevated, stage 1, stage 2, or stage 3) at the beginning of the Lifestyle Medicine program. According to the last blood pressure control of the study subjects, 11,1% of participants were able to normalize the blood pressure values. At the beginning of the program, we were able to identify cases of dyslipidemia. 55.6% of participants presented hypercholesterolemia. The results from the second control evidenced that the percentage of hypercholesterolemia in participants decreased to 22.2%. Furthermore, 33.3% of patients studied had high LDL in the beginning of the program, with a decrease in LDL cholesterol levels to 22.2% at the end of the study. table 1 details the data regarding the variables mentioned, with measures at the beginning and end of the study. Furthermore, in table 2 the statistical data is indicated (mean, standard deviation, and confidence Interval) of the numerical variables measured at the beginning and at the end of case follow-up.
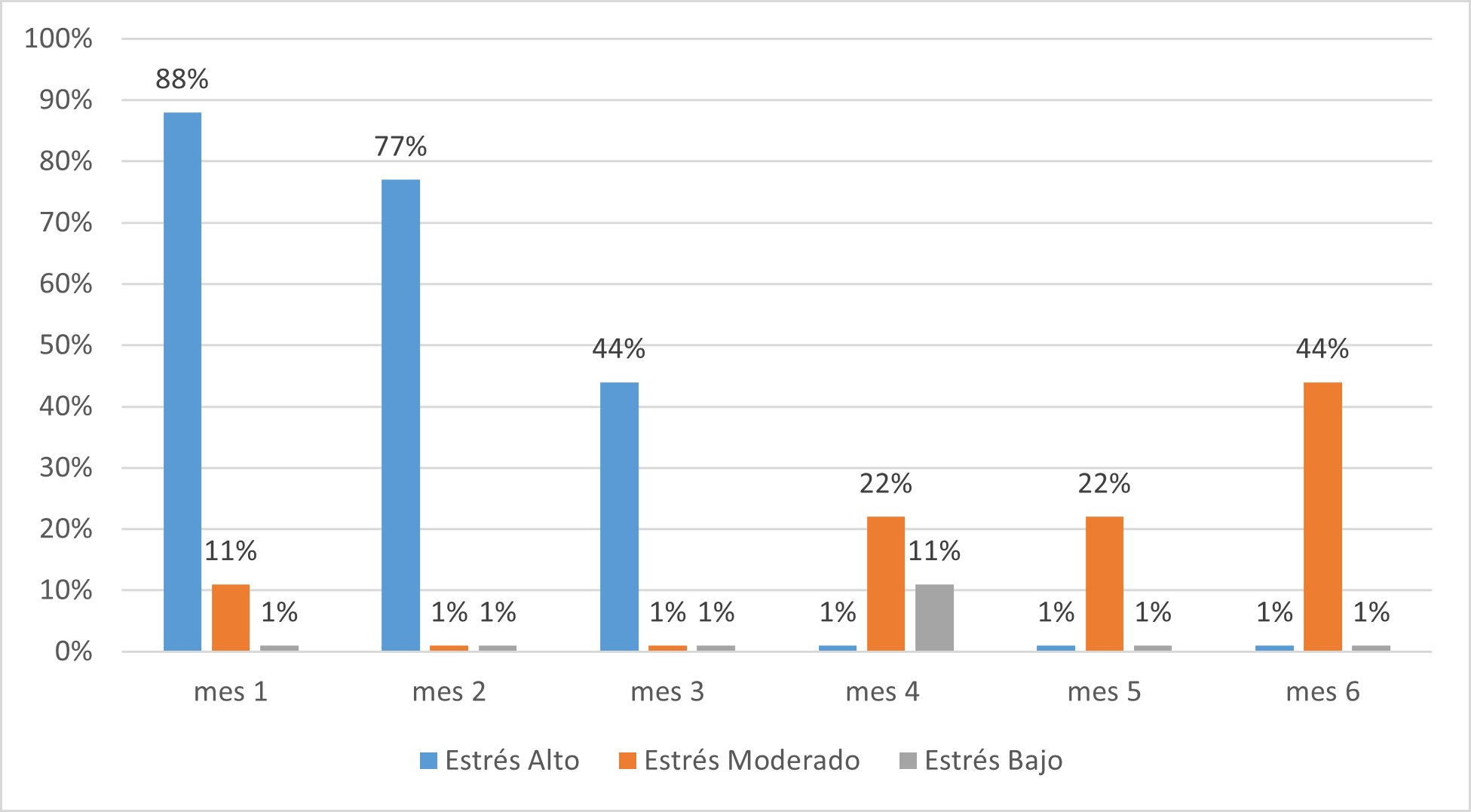
Among the findings of the perceived stress analysis through a systemized survey, we were able to evidence that all he patients went from high to moderate levels of stress in the course of 6 months of the program according to the sample in figure 2, furthermore, we obtained a percentage of absence of up to 54% in psychology consultations as is detailed in table 3.
The fat, muscle, and visceral fat percentage determination was carried out through bioimpedance measurement with our equipment Inbody 120. In table 4 the first and last measurement performed on these parameters in 9 study participants is described. Furthermore, according to the general body composition analysis (table 5), we observed the following results of the total number of patients during the study: decrease of body fat percentage of 4.2%, decrease of 6.5 kg of muscular mass and a decrease of up to 5% of average visceral fat.
Table 1. Variables measured at the beginning and end of the Lifestyle Medicine program in obese adult patients in a private institution of Colombia, 2019
| Variables | Initial Control | Last Control |
|---|---|---|
| n (%) | n (%) | |
| Cardiovascular Risk | ||
| Low | 7 (77.8%) | 9 (100%) |
| Intermediate | 2 (22.2%) | 0 (0%) |
| High | 0% | 0% |
| Obesity | ||
| Type 1 | 4 (44.5%) | 4 (44.4%) |
| Type 2 | 3 (33.3%) | 5 (55.6%) |
| Type 3 | 2 (22,2%) | 0% |
| Blood Pressure | ||
| Normal | 0% | 1 (11.1%) |
| Elevated | 3 (33.4%) | 4 (44.5%) |
| Stage 1 | 2 (22.2%) | 2 (22.2%) |
| Stage 2 | 3 (33.3%) | 2 (22.2%) |
| Stage 3 | 1 (11.1%) | 0% |
| Total Cholesterol | ||
| Normal Cholesterol | 4 (44.4%) | 7 (77.8%) |
| High Cholesterol | 5 (55.6%) | 2 (22.2%) |
| LDL cholesterol | ||
| Optimal LDL | 6 (66.6%) | 7 (77.8%) |
| Normal LDL | 3 (33.3%) | 2 (22.2%) |
Table 2. Numerical variables measured at the beginning and end of the Lifestyle Medicine program in obese adult patients in a private institution of Colombia, 2019
| Variables | Minimum | Maximum | Mean | SD* | Confidence Interval | |
|---|---|---|---|---|---|---|
| BMI 1 (kg/mts2) | 32 | 43 | 35,89 | 3,86 | 33.71 | 39.43 |
| BMI 2 (kg/mts2) | 32 | 39 | 35,11 | 2,42 | 33.71 | 37.14 |
| Total Cholesterol 1 (mg/dl) | 192 | 248 | 211,67 | 20,61 | 195.43 | 220.43 |
| Total Cholesterol 2 (mg/dl) | 190 | 217 | 199,29 | 9,19 | 193.72 | 206.00 |
| LDL Cholesterol 1 (mg/dl) | 51 | 160 | 121,78 | 32,36 | 91.73 | 135.86 |
| LDL Cholesterol 2 (mg/dl) | 65 | 150 | 117,44 | 23,56 | 113.86 | 134.00 |
| Weight 1 (Kg) | 89 | 141 | 109,67 | 16,99 | 100.57 | 125.57 |
| Weight 2 (Kg) | 87 | 127 | 106,89 | 12,99 | 99.43 | 118.28 |
| Systolic Pressure 1 (mmHg) | 120 | 150 | 132,22 | 10,92 | 122.86 | 138.57 |
| Diastolic Pressure 1 (mmHg) | 70 | 100 | 82,22 | 9,72 | 74.29 | 88.57 |
| Systolic Pressure 2 (mmHg) | 110 | 140 | 124,44 | 8,82 | 121.43 | 128.57 |
| Diastolic Pressure 2 (mmHg) | 70 | 90 | 78,89 | 6,009 | 75.71 | 84.29 |
Table 3. Frequency of attendance in the psychological consultations according to stress level in obese patients that participated in the Lifestyle Medicine program
| Stress | Month 1 | Month 2 | Month 3 | Month 4 | Month 5 | Month 6 |
|---|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | |
| High level | (8) 88% | (7) 77% | (4)44% | 0 | 0 | 0 |
| Moderate level | 0 | 0 | 0 | (2)22% | (2)22% | (4)44% |
| Low level | 0 | 0 | 0 | (1)11% | 0 | 0 |
| Did not attend | (1) 12% | (2) 23% | (5)56% | (9)67% | (7)88% | (5)66% |
Table 4. Bioimpedance measurements of the fat, muscle, and visceral fat percentages of obese patient during the 6 month follow up.
| PARTICIPANT | MEASURE | WEIGHT | %FAT | %MUSCLE (KG) | |
|---|---|---|---|---|---|
| VISCERAL FAT | |||||
| 1 | 1 | 94,5 | 29,3 | 36,7 | 13 |
| 2 | 99 | 32,9 | 37,2 | 15 | |
| 2 | 1 | 112,6 | 39,8 | 41,2 | 19 |
| 2 | 105,2 | 36 | 39,1 | 16 | |
| 3 | 1 | 94,4 | 30,6 | 37,4 | 12 |
| 2 | 93,9 | 29,8 | 37,5 | 12 | |
| 4 | 1 | 129,1 | 37,9 | 46 | 20 |
| 2 | 122,2 | 36,3 | 44,8 | 20 | |
| 5 | 1 | 88,5 | 39,8 | 29,9 | 17 |
| 2 | 86,6 | 39 | 29,8 | 17 | |
| 6 | 1 | 113,2 | 38,1 | 39,7 | 20 |
| 2 | 110,4 | 39,1 | 38,2 | 20 | |
| 7 | 1 | 141,4 | 39,9 | 48,7 | 20 |
| 2 | 126,5 | 35,1 | 47 | 20 | |
| 8 | 1 | 103,8 | 41,9 | 34 | 19 |
| 2 | 102,6 | 43,6 | 32,5 | 18 | |
| 9 | 1 | 109,7 | 37,8 | 38,3 | 19 |
| 2 | 114,9 | 39,1 | 39,3 | 20 |
Table 5. Analysis of body composition by Bioimpedance measurement according to parameters in 9 obese patients at the end of the 6 month follow up.
|
Parameters |
Final Results |
|---|---|
|
Body fat percentage (%) |
-4.2 |
|
Musculo-skeletal mass (kg) |
-6.5 kilograms |
|
Visceral fat level (%) |
-5 |
DISCUSSION
This intervention evidenced, as a relevant result, the decrease of cardiovascular risk from an intermediate level to a low level, due to the decrease in weight, blood pressure numbers, and blood lipid levels, with the intervention of the Lifestyle Medicine program in obese patients of a private institution in Colombia.
Upon performing the bibliographical search in different data bases, we found that no published articles exist that study the cardiovascular risk in an obese population through the application of the lifestyle medicine program in Latin America. However, a publication exists regarding the famous Diabetes Prevention Program (DPP), which is a closer vision to the Lifestyle Medicine approach applied in Latin American institutions (13). This was an uncontrolled intervention study implemented in five public clinics in northern Mexico, where health personnel were trained in the management of obesity. There was a high number of participant dropouts in the study after 12 months (60%), for this reason the study was centered mainly on the results at 6 months. In a similar way, this study was centered on the 6-month follow-up of obese Colombian patients who participated in a Lifestyle Medicine program, which included group activities, individual consultations with nutrition, psychology, and Lifestyle Medicine, bioimpedance measurements with inbody 120 equipment, which had a follow-up through text messages and phone calls.
The study performed in Mexico concluded that the intensive lifestyle medicine program is effective when applied by personnel that usually provides medical care to patients in real life, at least short-term. Furthermore, we accomplished the decrease of two factors that increased cardiovascular risk such as obesity and arterial hypertension (13) . IN our study we evidenced the decrease of intermediate cardiovascular risk in our patients from 22% to 0%, and patients with low risk at the beginning of the program were able to maintain the same level throughout the Colombian Lifestyle Medicine program. The program applied in our study improved the blood pressure values of the study subjects, revealing the normalization of arterial pressure in 11% of participants.
Some randomized controlled trials show that the subjects in the study evidence weight loss of 5% to 10% of their initial weight, up to 1 year after a high intensity lifestyle medicine intervention (14). Weight reduction was also an important result of our study. From the applied program, we were able to improve our patients who presented type 3 obesity to type 2 obesity over the course of 6 months the intervention lasted. This decrease could influence the reduction in risk of developing diabetes up to 20%, however, this must be shown by carrying out posterior analytical studies (15). Furthermore, the bioimpedance measurement which is a tool that proves the metabolic impact in obese patients allows us to measure the percentages of fat, muscle, and visceral fat, demonstrating an important decrease in body fat, muscle mass, and visceral fat percentages (16).
It is clearly evidenced that not only the decrease in weight is associated with a better control of diabetes and arterial hypertension, but also a diet low in carbohydrates(17), and plant-based(18), which is why a nutritional plan was provided, with a prescription of daily physical activity, in addition, the participants carried out a record of daily activities where the following data was included: amount of food per day, mood, daily hours of sleep, amount of daily minutes to perform physical activity, level of satiety with food. With the support of this program, we aim to reduce the need for pharmacological treatment for chronic diseases such as arterial hypertension and type 2 diabetes mellitus.
The approach and intervention of these patients was performed in a multidisciplinary form where an internal medicine physician expert in nutrition, a licensed psychologist, and a licensed nutritionist participated, all with lifestyle medicine training. Keeping in mind the presented statistics and what was evidenced during the psychological consultation we found that the greater drop-out was 88% of total participants, which was evidenced during the fifth month of follow-up. This could be because the treated patients did not show interest for the treatment they were offered, they had not internalize the problem of their situation, leaving aside the importance of mental health programs to achieve treatment adherence, especially regarding behavioral changes. This is supported by Orozco-Gomez, who argues that “one of the intervention techniques is the motivational interview, which enables acquiring a commitment for behavioral change, through acknowledgment and empowerment of present and potential problems”(19). , ==. Even when few patients attended the psychological consultation, we were able to decrease anxiety levels among the participants from a high level to an intermediate level, in their majority.
One of the study’s limitations was the sample size, not having the results of the other lipid profile parameters (HDL, TG) and glucose, which is why, these variables were not taken into account in this study. Furthermore, although we evidenced that patients were able to decrease the stress levels by attending psychological consultations, some of them did not attend these evaluations. We believe that multicentric research should be considered, not only for learning about the results of the Lifestyle Medicine Program application in other institutions but for generalizing the results obtained about the benefits of the lifestyle medicine application, and more so because this type of intervention has not been carried out in Colombian territory. Furthermore, the obtained results should be used to find the control or reversion of different chronic diseases, some of which are hypertension or type 2 diabetes mellitus, which is why we recommend performing longitudinal studies that imply follow-ups greater than six months
It is novel to apply a program with the mentioned characteristics in this study, where we did not use medication or drugs for weight loss, but only applied protocols under scientific evidence of Lifestyle Medicine. The decrease of costs for use of drugs was able to decrease the financial burden of obese patients. Posing this proposal would save health systems an economic burden that with time would become unsustainable, acknowledging that the economic impact of attention to comorbidities associated with obesity in Colombia rises to 2,158 million dollars (20) For the aforementioned, it would be convenient to continue strengthening the application of Lifestyle Medicine in the primary care, promotion and prevention and even secondary care programs, for the integral benefit of participants.
CONCLUSIONS
Due to the results presented and discussed, we conclude that the implementation of a Lifestyle Medicine program applied locally (Colombia) could reduce the magnitude of cardiovascular risk and improve the metabolic control of people with chronic diseases. According to this, institutional services rendered with a focus on Lifestyle Medicine could improve the burden of non-transmissible chronic disease such as obesity, affecting in the decrease of blood pressure levels. Finally, having a qualified team in Lifestyle Medicine in the health institutions of Colombia, offers the possibility of improving the health of people that access the national health services.
Authorship contributions: The authors participated in the genesis of the idea, Project design, data collection and interpretation, results analysis, and manuscript preparation of this research work.
Funding sources: info 2.
Conflicts of Interest: The authors declare not having conflicts of interest.
Received: August 30, 2021
Approved: November 22, 2021
Correspondence: Lucy Cedillo Ramirez
Address: Av. Alfredo Benavides 5440, Santiago de Surco 15039
Telephone: 993093310
E-mail: lucycedilloramirez.tj@gmail.com
References