CASO CLÍNICO
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2022 - Universidad Ricardo Palma10.25176/RFMH.v22i4.4746
PORTAL THROMBOSIS IN ANTIPHOSPHOLIPID SYNDROME: CASE REPORT
TROMBOSIS PORTAL EN SÍNDROME ANTIFOSFOLIPÍDICO: REPORTE DE CASO
Elkin J Pelaes-Cruz1,a,c, Yomayra S. Chigne-Castro1,a, Wagner Brando Rios-Pereda1,a, Yran Rebaza Castillo1,a, Magaly del Pilar Rodriguez Raza1,a, Brooke Marjorie Rodriguez-Cárdenas1,a, Wagner Brando Rios-Pereda1,a, Camilo Peña-Quispe2,b
1Facultad de Medicina de la Universidad Nacional de Trujillo, La Libertad, Perú
2Servicio de Cuidados Intensivos del Hospital Regional Docente de Trujillo. La Libertad. Perú
aMedical Student
bInternist Physician
cMember of the Scientific Society of Medical Students,Universidad Nacional de Trujillo
ABSTRACT
Antiphospholipid syndrome (APS) is a systemic autoimmune disorder characterized by arterial, venous, or small vessel thrombosis and recurrent early pregnancy loss, fetal loss, or pregnancy morbidity in the context of persistent antiphospholipid antibodies. Characterized by the development of multiple thrombotic manifestations, simultaneously or within a short period of time; portal vein thrombosis (DVT) being a rare and serious clinical manifestation and a predictor of poor prognosis.The case of an elderly patient with abdominal pain and portal vein thrombosis associated with APS with antithrombotic treatment and analgesics of favorable evolution is presented.
Keywords: Antiphospholipid syndrome; Venous Thrombosis; Antibodies; Antiphospholipid. (Source: MeSH NLM).
RESUMEN
El síndrome antifosfolípido (SAF) es un trastorno sistémico autoinmunitario caracterizado por trombosis arterial, venosa o de vasos pequeños y/o pérdida temprana recurrente del embarazo, pérdida fetal o morbilidad del embarazo en el contexto de anticuerpos antifosfolípidos persistentes. Caracterizada por el desarrollo de múltiples manifestaciones trombóticas, de manera simultánea o dentro de un corto período de tiempo; siendo la trombosis de la vena porta (TVP) una manifestación clínica rara, grave y un predictor de mal pronóstico.Se presenta el caso de una paciente de avanzada edad,con dolor abdominal y portadora de trombosis venosa portal asociada a SAF con tratamiento antitrombótico y analgésicos de evolución favorable.
Palabras Clave: Síndrome antifosfolípido; Trombosis de la Vena; Anticuerpos; Antifosfolípidos. (fuente: DeCS BIREME).
INTRODUCTION
Antiphospholipid syndrome (APS) is an acquired autoimmune thrombophilia mediated by autoantibodies, such as lupus anticoagulant or anticardiolipin or b2-glycoprotein 1, sometimes accompanied by thrombocytopenia (1). The description of FAS occurred in 1983 after several years of study of lupus, myelopathy and forms of connective tissue disease. In 1963, Bowie et al. reported the paradoxical occurrence of thrombosis and recurrent fetal loss in patients with lupus anticoagulant (LAC). Between 1970-1980, the nature of LAC is identified, and around 1980, the link with anticardiolipin (aCL) is established. In the 1990s, it is postulated that aPL requires a plasma protein as a cofactor, subsequently demonstrating the fundamental role of anti-β 2 glycoprotein 1 antibodies in the pathophysiology of PAS (2).
APS represents a public health problem since its prevalence in the general population is 1-5%. Epidemiological data indicate a worldwide incidence of approximately five new cases per 100,000 people per year and a prevalence of 40-50 cases per 100,000 population. aPL are positive in approximately 13% of patients with stroke, 11% with acute myocardial infarction (AMI), 9.5% of patients with deep vein thrombosis, and 6% of patients with pregnancy morbidity.(3,4)
This syndrome may be found in patients in whom there is no clinical or laboratory evidence suggestive of another entity or may be associated with other diseases, mainly systemic lupus erythematosus (SLE), but also occasionally with other autoimmune diseases, infections, drugs and malignancies. (5-7) In addition to the distinctive features of venous, arterial and/or small vessel thrombosis, as well as pregnancy-specific complications; other relatively common clinical features include livedo reticularis, thrombocytopenia or transient ischemic attack and in rare cases multiorgan failure due to small vessel thrombosis (catastrophic antiphospholipid syndrome) (8,9).
DESCRIPTION OF THE CLINICAL CASE
A 65-year-old female patient from Pataz, who worked as a cook in a mine, with no history of COVID-19; reported abdominal pain for a year in the left upper quadrant, non-radiated, of moderate intensity, intensifying in recent months, without an antalgic position. She has a history of hypercholesterolemia, arterial hypertension (AHT) with treatment of enalapril 20 mg b.i.d, with no relevant family history. She is being treated with pump inhibitors (Omeprazole), prokinetics (Levosulpiride), and NSAIDs without improvement. Two weeks ago the patient complained of abdominal pain, for which reason she sought consultation with private physicians, and an ultrasound was performed, which was taken to the hospital.
Normal vital signs were identified; and during the physical examination, abdominal pain in the left upper quadrant, non-palpable spleen, globular abdomen, without evidence of edema in the lower limbs, without other significant findings. Laboratory tests showed thrombocytosis, elevated rheumatoid factor, elevated triglycerides, and VLDL cholesterol. Normal PCR (See Table 1) anti B2 glycoprotein positive, ANCA C, ANCA P, and anti-DNA negative.
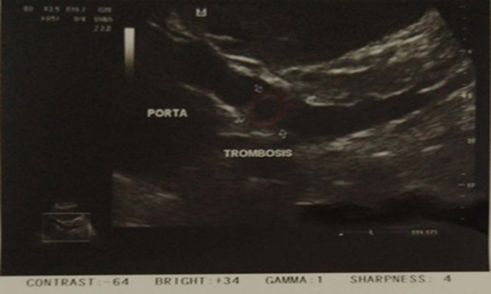
An abdominal ultrasound was requested to confirm the previous findings, where moderate hepatosplenomegaly was evidenced. In addition, focal thrombosis was observed at the level of the hepatic hilum, leading to a dilatation of the portal and splenic veins (See Figure 1).
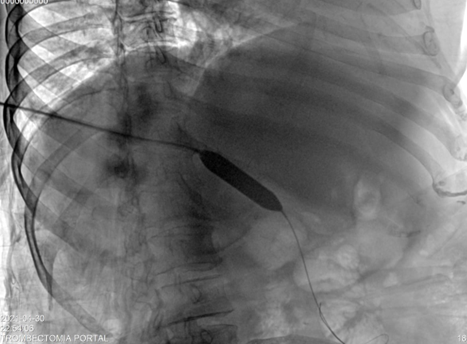
In addition, a Doppler ultrasound was performed, which revealed antegrade flow and mean portal velocity less than 10 cm/s. A diagnosis of portal thrombosis was confirmed with indication for percutaneous thrombectomy: the portal vein was entered, 10cc of alteplase was placed, the clot was fragmented and aspirated, leaving the angioplasty balloon catheter for 5 days, and then it was removed. (See Figura 2).
After the procedure, treatment with Rivaroxaban 20 mg/day, Paracetamol 325 mg b.i.d and Tramadol hydrochloride 37.5 mg b.i.d was started and Doppler was performed 5 days later, finding: anterograde flow towards the liver with average portal velocity of 22 cm/s (See Figura 3), maintaining the anticoagulant treatment until nowadays.
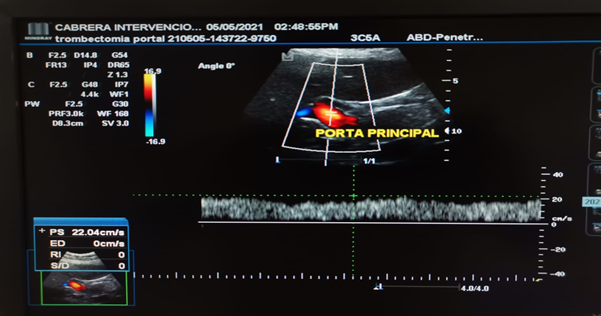
Tabla 1. Exámenes de laboratorio.
| Exámenes de laboratorio | Rango de referencia | Al ingreso | 1 semana después | 2 semanas después | 4 meses después |
|---|---|---|---|---|---|
|
Hemograma: Neutrófilos (%) |
55.0 - 65.0 | 65.5 | - | - | |
| Glóbulos rojos (106 / ul) | 4.00 - 5.00 | 7.81 | - | - | - |
| Hemoglobina (g/dll) | 12.0 - 13.6 | 15.9 | - | - | - |
| Hematocrito (%) | 37.0 - 42.0 | 54.6 | - | - | - |
| VCM (fl) | 80.0 - 99.0 | 69.9 | - | - | - |
| HMC (pg) | 27.0 - 34.0 | 20.4 | - | - | - |
| RDW-CV (%) | 11.0 - 16.0 | 22.9 | - | - | - |
| RDW-SD (fl) | 35.0 - 56.0 | 66.1 | - | - | - |
| Plaquetas (103 / ul) | 150 - 450 | 586 | - | - | - |
| PCT % | 0.108 - 0.282 | 0.443 | - | - | - |
| Electrolitos | |||||
| Na (mEq/l) | 135.0 - 148.9 | - | 131.1 | - | - |
|
Factor reumatoide (Ul / mL) |
82.3 | - | 0 - 20 | - | - |
|
triglicéridos (mg/dL) |
<150 | - | - | 214 | - |
|
Colesterol VLDL (mg/dL) |
5 - 40 | - | - | 43 | - |
|
Proteína C (%) |
70 - 140 | 141.4 | |||
|
Anticuerpos anti-B2 glicoproteína (U/ml) |
5 - 8 | 15.4 |
DISCUSSION
FAS is a systemic autoimmune disease characterized by thrombotic events and obstetric complications, with the presence of persistently positive aPL. Among the most common aPL subgroups detected are AL, anti-β2-glycoprotein I antibody and aCL (10).
The prevalence of aPL is 5% in the general population; however, few people develop FAS (11). This syndrome is based on attacks against phospholipids of the cell membrane and vascular endothelium through antibodies, which explains the basic lesion of thrombotic occlusion of small and large vessels that results in decreased blood flow, explaining in large part the manifestations present in the patient. In addition to the above, there are associations of antiphospholipid antibodies to thrombosis and vascular diseases that can be classified as primary or secondary according to the appearance of another autoimmune disease (12).
The diagnosis of APS is based on the Sapporo criteria, which include clinical and laboratory data. Within the former, vascular thrombosis, certain alterations during pregnancy, or both are considered. Laboratory criteria include the presence of lupus anticoagulant; anticardiolipin IgG, IgM or both and anti-B2-glycoprotein 1 IgG, IgM or both. To establish the diagnosis, at least one clinical and one laboratory criterion is required (10,13). In the patient's case, a marked thrombosis with decreased flow velocity of less than 10 cm/s in the portal vein was evidenced by Doppler ultrasound. Laboratory tests were positive for lupus anticoagulant, anticardiolipin and anti-B2-glycoprotein 1.
The Sydney criteria for diagnosis contemplate a clinical and a laboratory criterion with the persistent presence (more than 12 weeks) of one or more of the antiphospholipid antibodies: LA, anti-β2-glycoprotein I antibodies and aCL. Patients with PBS may present with one, two or three of these positive tests for aFL. The highest risk of thrombosis has been found to be associated with the presence of LA, while aCL antibodies and anti-β2-glycoprotein I antibodies to a lesser extent. Triple-positive patients (LA, aCL, and anti-β2-GPI) are at even greater risk of developing thrombosis than those positive for one or two antibodies (14,15).
CONCLUSION
APS is a pathology that can trigger prothrombotic pictures and that, if not adequately determined and treated, would evolve to catastrophic APS and subsequent death of the patient. Therefore, it is necessary to evaluate clinical, imaging and laboratory data together, with β-2 glycoprotein or apolipoprotein H being the most important antigen in the disease. Although the literature mentions that the classic triad is thrombocytopenia, thrombotic phenomena and fetal loss, in this case the patient presented thrombocytosis, so its diagnosis becomes a challenge if we do not have the analysis of antiphospholipid antibodies. The present clinical case helps us to define and treat a potentially fatal pathology, it will also serve as a starting point for the search of new cases, in such a way that it expands our knowledge about the possible diagnoses of a patient with abdominal pain, remembering what the books of semiology state: the abdomen is a pandora's box.
Authorship contributions: The authors participated in the original Genesis, data interpretation, and drafting of the manuscript.
Funding sources: Self-financed.
Conflicts of interest: The authors declare that they have no conflicts of interest with the content of the manuscript.
Received: March 30, 2022
Approved: August 17, 2022
Correspondence: Elkin Joel Pelaes Cruz.
Address: Jr. H. Valdizan 1382 Urb. Los Jardines - Trujillo.
Telephone number: 915385522
E-mail: elkinpelaescruz@gmail.com
Article published by the Journal of the faculty of Human Medicine of the Ricardo Palma University. It is an open access article, distributed under the terms of the Creatvie Commons license: Creative Commons Attribution 4.0 International, CC BY 4.0(https://creativecommons.org/licenses/by/1.0/), that allows non-commercial use, distribution and reproduction in any medium, provided that the original work is duly cited. For commercial use, please contact revista.medicina@urp.edu.pe.
REFERENCES
