CASO CLÍNICO
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2022 - Universidad Ricardo Palma10.25176/RFMH.v22i2.4792
TUBERCULOSIS ORCHIEPIDIDYMITUS IN INSULIN-DEPENDENT TYPE 2 DIABETES MELLITUS: CASE REPORT
ORQUIEPIDIDIMITIS TUBERCULOSA EN DIABETES MELLITUS TIPO 2 INSULINODEPENDIENTE: REPORTE DE CASO
Gonzalo Carrillo-Sanabria 1,2,a, Brayan Dávila-Aranda 1,2,a, Rodolfo Cairo-Huaringa 3,b, Richard Maita-Hinostroza 3,c, Jorge Chumbes-Pérez 3,d
1 Facultad de Medicina Humana, Universidad Peruana Los Andes. Huancayo, Perú.
2 Sociedad Científica de Estudiantes de Medicina Los Andes (SOCIEMLA). Huancayo-Perú.
3 Hospital Nacional “Ramiro Prialé Prialé” R.A.J. Huancayo-Perú.
a Estudiante del 6to año Medicina Humana.
b Médico especialista en Radiología.
c Médico especialista en Anatomía Patológica.
d Médico especialista en Infectología.
ABSTRACT
Introduction: Peru has little information about the association of tuberculous orchiepididymitis in relation to immunosuppressed patients, being a country endemic for tuberculosis and having an increased prevalence of chronic non-communicable diseases such as diabetes, leading to misdiagnosis. Clinical Case: We present the case of a 70-year-old man with a history of type 2 diabetes mellitus who was admitted to the outpatient clinic due to dysuria and frequent urination. On physical examination, the right testicle was hard, not painful. The ultrasound showed signs of epididymal abscess in the scrotal wall of the right testis, so an infected neoplasm is suspected, performing a right orchiectomy. Later in the histological study, they show giant multinucleated Langhans-type cells with granulomatous areas suggestive of tuberculosis, so it is suggested that in the presence of urological symptoms in patients immunosuppressed tuberculosis is ruled out.
Keywords: Tuberculosis; Orchitis; Epididymitis; Hyperglycemia. (Source : MeSH - NLM).
RESUMEN
Introducción: Hay poca información en el Perú sobre la asociación de orquiepididimitis tuberculosa en relación a los pacientes inmunosuprimidos, siendo un país endémico de tuberculosis y habiendo un incremento de la prevalencia de las enfermedades crónicas no transmisibles como la diabetes produciendo diagnósticos equivocados. Caso Clínico: Se presenta el caso de un varón de 70 años con antecedente de diabetes mellitus tipo 2 que ingresa por consultorio externo por disuria y polaquiuria, al examen físico testículo derecho duro, no doloroso, en la ecografía se evidencia signos de absceso epididimario en pared escrotal del testículo derecho por lo que se sospecha de una neoplasia infectada realizándose una orquiectomía derecha, posteriormente en el estudio histológico evidencian células gigantes multinucleadas tipo Langhans con áreas granulomatosas sugerente a tuberculosis por lo que se plantea que ante la presencia de síntomas urológicos en pacientes inmunosuprimidos se descarte tuberculosis.
Palabras Clave: Tuberculosis; Orquitis; Epididimitis; Diabetes mellitus. (Fuente: DeCS BIREME).
INTRODUCTION
Around 15% of extrapulmonary TB represents genitourinary tuberculosis; since it is the second common
manifestation in the countries of Europe. Commonly infected sites are the epididymis, seminal vesicle,
prostate, and testes(1).
Genital TB is rare, and testicular TB is even more infrequent, comprising only 3%. Thus, scrotal
infection by Mycobacterium tuberculosis occurs in 7% of patients (1); being
the most common site of genital TB, the epididymis, followed by the seminal vesicles, the prostate, the
testicles, and the vas deferens. As the epididymis is affected first, orchitis occurs by contiguous
extension and reflects a late stage of the disease. Other authors postulate dissemination through the
pelvic lymphatic system and venereal transmission(2), with the most affected
middle-aged men.
According to the World Health Organization, in 2016, there were an estimated 10.4 million new
cases of active tuberculosis (TB) per year, and 1.8 million deaths in 2015 from Mycobacterium
tuberculosis(3).
The global prevalence of diabetes is 8.3%; In Latin America, the prevalence of diabetes is 5%.
In Peru, there is insufficient epidemiological data on DM: however, some studies suggest a prevalence of
5 to 7% (4).
The association between TB and DM was described in the middle of the 20th century. Evidence
supports the hypothesis that DM increases the susceptibility to developing TB due to
immunodeficiency(5). However, the emergence of comorbidities such as HIV /
AIDS and diabetes mellitus (DM) jeopardize the goal of global TB elimination by 2050(6).
In Peru, the evidence on the effect of DM and TB is scarce; Only one cohort study in patients at
high risk of resistant TB was associated with 11% with DM(7).
Through this case, it is proposed that in the presence of urological symptoms in
immunosuppressed patients, tuberculosis should be ruled out before any surgical procedure, on the other
hand, it is proposed to analyze the relationship that exists between the state of immunosuppression of
patients with DM and the extrapulmonary forms of tuberculosis, emphasizing in the testicular
presentation.
DESCRIPTION OF THE CLINICAL CASE
This is a case of a 70-year-old man from Huancayo-Junín, with insulin-dependent diabetes mellitus type
2, prostatectomy 10 years ago, and intermittent urinary infection without response to antibiotic
treatment. The patient is admitted with dysuria and frequency of 1-month evolution; He denies contact
with tuberculosis, fever, sweating, and weight loss.
On examination: pain in the lower abdomen, PRU positive. Right testicle of hard consistency, not
painful; a normal left testicle.
Laboratory analysis: leukocytes 7650 cells/mm3, Hb 16.99 gr/dl, platelets 507000 cells/mm3,
glucose 195 mg/dl, glycosylated hemoglobin 7.3%. Urine test: glucose ++, leukocytes and red blood cells
1 per field and BAAR in urine x 2 negative. Prostate-Specific Antigen 2.69ng/ml.
Ultrasound: Right testicle of 34x13x25mm, echo hard structure, signs of epididymal abscess and
scrotal wall. Left testicle with normal shape, echostructure, and size (36x14x23mm), without signs of
varicocele hydrocele. Grade 3 prostatic hyperplasia and kidney stones.
A testicular neoplasm is suspected and added to the ultrasound findings of an epididymal abscess
based on age and physical examination. An infected testicular neoplasm is proposed as a diagnosis,
indicating right orchiectomy.
Macroscopic study: right testicle plus epididymis 8x4cm, smooth surface; On cut, yellowish brown
stroma with a focus of purulent secretion.
Histopathology: positive acid-fast bacillus (AFB) staining, areas of fibrosis, and mixed
inflammatory infiltrate with the presence of giant multinucleated Langhans-type cells with granulomatous
areas that defines a diagnosis of tuberculous orchiepididymitis and initiates antituberculous treatment
with isoniazid, rifampicin, pyrazinamide, and ethambutol (2HRZE + 4HR) for 6 months. The patient evolved
favorably. (Figure 1)

DISCUSSION
Tuberculosis is caused by aerobic, non-motile, airborne Mycobacterium tuberculosis. Pulmonary
tuberculosis (TB) is the most common type and represents 70% of cases, spreading especially in
immunocompromised patients and young children. The spread of TB to the testicle can result in a
secondary infection of the epididymis (8).
In relation to the case, we observed an important history of being an insulin-dependent
diabetic, therefore an immunocompromised person who, according to the evidence, describes the risk of up
to three times more possibilities of becoming infected and developing TB and being able to develop
extra-pulmonary disease between 15% and 28%. genitourinary tuberculosis was the outcome of our patient;
however, the involvement of other organs such as the prostate, seminal vesicle, vas deferens, testicle,
penis, and epididymis is also reported as a frequent complication(6). Thus, it
is pointed out that genitourinary TB represents 5% of cases of extrapulmonary tuberculosis, the most
frequent location being the epididymis, as it was in the case presented(7).
At the age of 40 years, urogenital tuberculosis is twice more frequent in men than in women,
suggesting that the presence of urinary symptoms and sterile pyuria has renal compromise. On the other
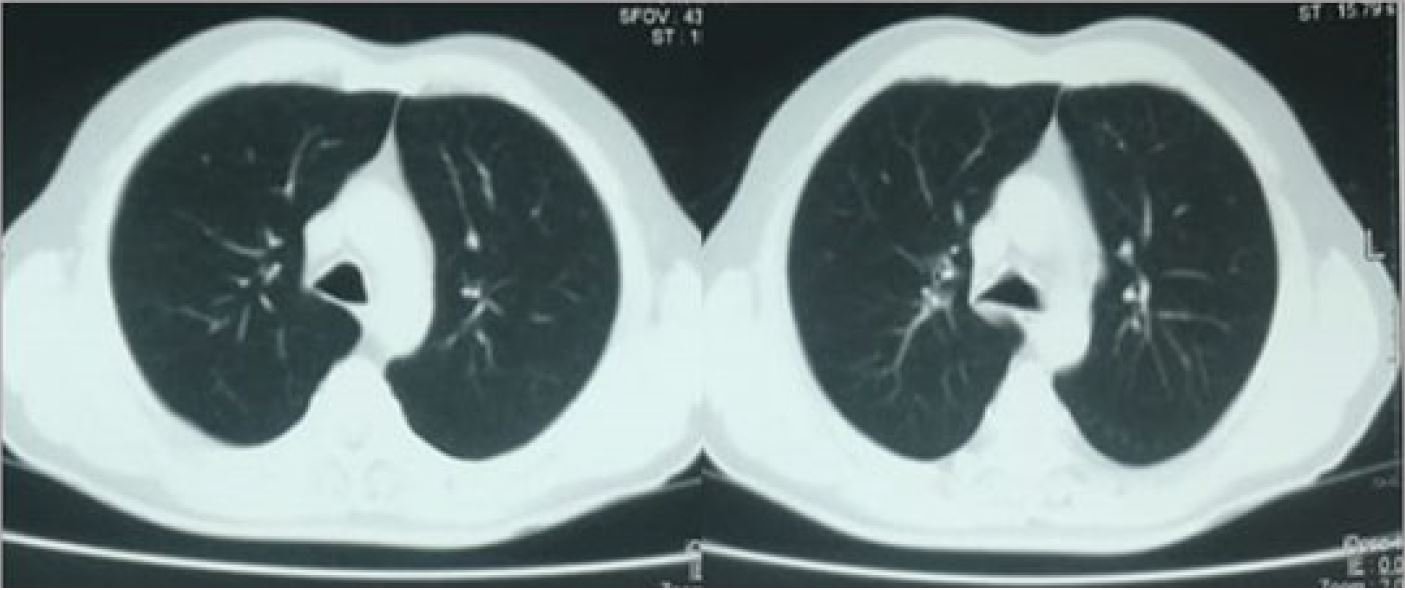
hand, a pulmonary alteration can be visualized in the imaging study even in 75%. In our case, the
patient reported having presented dysuria and intermittent frequency with an evolution time of up to one
month, coinciding with the literature(6).; however, no apparent primary
pulmonary focus was found since the chest tomography did not show characteristics of having suffered
from this disease. (Figure 2)
Physical examination findings may include a tender nodule, dilation, and thickening of the epididymis.
Testicular involvement can be unilateral or bilateral. Epididymal involvement classically shows up as a
heterogeneous hypoechoic mass on ultrasonography. In the urinalysis, albuminuria or hematuria may also
be observed. Others report cases of infertility(7).
Clinically, it is not usually distinguishable from the testicular tumor, acute infection
(bacterial or viral), granulomatous infection (sarcoidosis), or infarction, and can even, in some cases,
mimic testicular torsion(5). Epididymal enlargement and thickening of the
scrotum are the key points of infection.
Testicular ultrasound is currently the best technique for the diagnosis of testicular injury.
Here, a great thickening and formation of a dense, caseous mass are observed, which can rupture and give
rise to tedious fistulas. Other sonographic findings include thickening of the scrotal skin, hydrocele,
calcifications, and scrotal abscess. The addition of Doppler ultrasound serves to assess blood flow and
helps differentiate testicular infarction, tumor, or inflammation (5).
Regarding the presence of DM, data indicate that having HA1C greater than seven is a risk factor
for latent tuberculosis(9). In addition, there are differences in the
pharmacokinetics of drugs for TB and DM and other comorbidities such as hypertension or obesity, which
leads to a higher risk of death and relapse(10).
In our case, a patient with immunosuppression, diabetes, compatible symptoms, and histology with
epithelioid granulomas, caseous necrosis, and Ziehl-Neelsen staining confirmed the diagnosis.
The evidence recommends antituberculous treatment with the usual regimen of isoniazid, rifampin,
pyrazinamide, and ethambutol (2HRZE + 4HR) for 6 months, through which cure rates of 95% are obtained.
However, surgical intervention may be necessary, especially in severe cases, such as no clinical
response to treatment, increased testicular size, and edema or abscess formation (11).
One of the challenges that occur in patients with DM-TB is therapeutic management since it has
been shown that the levels of anti-TB drugs in plasma are below therapeutic values(12). This, added to hyperglycemia, makes management difficult.
There are still no randomized studies that evaluate an adequate treatment for TB-DM, and there
is not enough evidence to evaluate the effect of insulin or metformin(13),
with the use of the insulin being recommended in Peru(14).
In endemic countries such as Peru, patients with symptoms such as long-standing dysuria and
frequency, scrotal mass, or chronic epididymitis should be evaluated for tuberculosis. This would
significantly reduce any delay in establishing a diagnosis, increasing the chances of quick management
and recovery. A surgical approach should be considered only in cases where the diagnosis is not clearly
established or when there is a strong clinical indication. yellowish-brown stroma with a focus of
purulent secretion.
Authorship contributions: All the authors have participated in the article’s conception,
the data collection, its writing and approval of the final version.
Funding sources: This report was self-financed by the authors.
Conflicts of Interest: All authors declare that they have no conflicts of interest.
Received: July 29, 2021
Approved: October 30, 2021
Correspondence: Rubén Gonzalo Carrillo Sanabria
Address: Los Andes Peruvian University - Huancayo
Telephone number: 965053501
E-mail: rubengonzalo31@gmail.com
REFERENCES
-
div id="1">1. WHO. Global tuberculosis report 2016. World Health Organization, Geneva; 2016.
http://www.who.int/tb/publications/global_report/en/.Accessed May
12,2017.
