ARTICULO ORIGINAL
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2022 - Universidad Ricardo Palma10.25176/RFMH.v22i4.5066
SOFA AND QSOFA SCALES AS MORTALITY PROGNOSIS IN PATIENTS DIAGNOSED WITH SEPSIS IN A PERUVIAN CLINIC
ESCALAS SOFA Y QSOFA COMO PRONÓSTICO DE LA MORTALIDAD EN PACIENTES CON DIAGNÓSTICO DE SEPSIS DE UNA CLÍNICA PERUANA
Ottavia Scarsi-Mejia1,a, Katerine Maite Garcia-Moreno2,b
1Surgery, Ventanilla Hospital. Lima, Peru
2Universidad Científica del Sur, Faculty of Health Sciences,
Human Medicine Career, Lima, Peru
aGeneral Surgery Resident
bMedical Surgeon
ABSTRACT
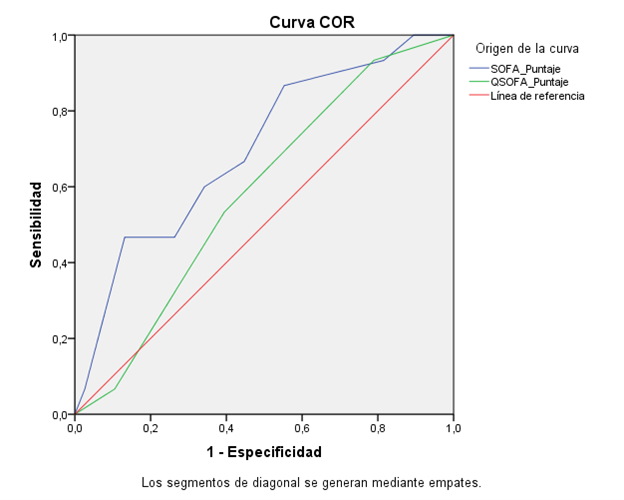
Introduction: Sepsis is a clinical condition that seriously threatens the balance of the organism and is still a leading cause of mortality. Therefore, clinical management aims at timely classification and implementation of emergency measures based on scale systems for detection that help reduce patient complications. Hence the importance of using SOFA (Sequential Organ Failure Assessment), qSOFA (quick SOFA) in the different services in hospitalized patients. Objectives: To evaluate the usefulness of the SOFA and qSOFA scales as a prognosis of mortality in patients with sepsis hospitalized in the intensive care unit (ICU) of the Good Hope Clinic from January to December 2015. Materials and Methods: Retrospective study of adult patients hospitalized in service ICU/NICU with sepsis diagnoses. The epidemiological, clinical, and laboratory data necessary to apply the SOFA and qSOFA scales were collected. A description of the variables studied, an analysis, and the scoring systems compared in the ROC curve were made. Results: The main infectious focus was respiratory (41.5%). 28.3% of the patients died. The variables creatinine and serum lactate proved to be statistically significant with OR=11.67 (95% CI 2.58-52.85, p<0.001) and OR=5.78 (95% CI 1.45-23.03, p=0.009), respectively. The SOFA AUC was 0.698, p=0.026, 95% CI (0.54-0.85), proving to be statistically significant. A cut-off point of 7.5 with a sensitivity of 46.7% and 86.8% specificity was found. The QSOFA scale did not show a statistically significant association. Conclusions: The SOFA scale was associated with the probability of death in patients with sepsis admitted to the ICU/NICU service.
Keywords: Sepsis; Critical care; Mortality; SOFA; qSOFA. (Source: MeSH NLM).
RESUMEN
Introducción: La sepsis es una condición clínica que amenaza gravemente el equilibro del organismo siendo aún una principales causas de mortalidad. Por lo que el manejo clínico es dirigido a una oportuna clasificación e implementación de medidas de emergencia basadas en sistemas de escalas para una detección que ayude a reducción de complicaciones en los pacientes. Ahí la importancia de utilización de SOFA (Sequential Organ Failure Assessment), qSOFA (quick SOFA) en los diferentes servicios en pacientes hospitalizados. Objetivos: Evaluar la utilidad de las escalas SOFA y qSOFA como pronóstico de mortalidad en pacientes con sepsis hospitalizados en la unidad de cuidados intensivos (UCI) de la Clínica Good Hope de enero a diciembre del 2015 Métodos: Estudio retrospectivo de pacientes adultos hospitalizados en servicio de UCI/UCIN con los diagnósticos de sepsis. Se recabaron los datos epidemiológicos, clínicos y laboratoriales necesarios para aplicar las escalas SOFA y qSOFA. Se realizó descripción de las variables estudiadas, análisis de las variables y los sistemas de puntuación comparados en la curva ROC. Resultados: El principal foco infeccioso fue el respiratorio (41.5%). Fallecieron 28.3% de los pacientes. Las variables creatinina y lactato sérico demostraron ser estadísticamente significativos con un OR=11.67 (IC 95% 2.58-52.85, p<0.001) y OR=5.78 (IC95% 1.45-23.03, p=0.009), respectivamente. El AUC de SOFA fue 0.698, p=0.026, IC 95% (0.54-0.85), demostrando ser estadísticamente significativa. Se halló un punto de corte de 7.5 con una sensibilidad de 46.7% y 86.8% de especificidad. La escala QSOFA no demostró asociación estadísticamente significativa. Conclusiones: La escala SOFA mostro asociación probabilidad de fallecimiento de los pacientes con sepsis admitidos en servicio de UCI/UCIN.
Palabras Clave: Sepsis; Cuidados críticos; Mortalidad; SOFA; qSOFA. (fuente: DeCS BIREME).
INTRODUCTION
Sepsis continues to be one of the major causes of death worldwide (1,2). The seriousness of clinical implications and the dysfunction given in the organism generates a high risk for the person, added to it the due specialized management that patients in this condition are granted; they suppose a complex clinical scenario that must be resolved following protocols that favor the recovery of the patient. Prognostic scales are the most used tools in intensive care services and contribute to decisions (3,4).
The prevalence of intensive care unit (ICU) sepsis varies between 5-19% (5). In a study carried out in the Community of Madrid in 2001, 6,968 episodes of severe sepsis were identified. The annual incidence was 14.1/10,000 inhabitants, highest in those over 84 years of age, with an overall mortality of 33% (6). A multicenter study conducted in Mexico, which included 135 ICUs from 24 states, concluded that 27.3% of annual admissions were due to sepsis, with a mortality of 30.4% (7). In Colombia, 10 ICUs from 4 cities were studied between 2007-2008; 51% of the patients developed sepsis in the community, 44% in the ICU, and 5% during hospitalization in the general ward, with a total mortality rate of 33.6%(8). In Chile, a study was carried out that included 94% of all ICUs in that country, severe sepsis was the admission diagnosis of 33%; in which severe sepsis was the reason for admission to the ICU, the lethality was 27.4% at 28 days, and 25.9% in the 112 patients who presented this condition on the day of the survey (5).
In our country, there are no national data; however, they do exist for hospitals in Lima. The study was conducted at the Edgardo Rebagliati Martins National Hospital on patients admitted to the ICU with a diagnosis of severe sepsis or septic shock; 25.2% died in the ICU, and 30% within 28 days of follow-up (9). Similar studies have not been carried out in our institution.
Taking into account the new recommendations published in February 2016 by the Society of Critical Care Medicine (SCCM) at the 45th Critical Care Congress in Orlando, Florida, which defines sepsis as “organ dysfunction caused by an abnormal host response to infection that is life-threatening,” and recommends using the SOFA scale and the new qSOFA scale to identify the patient with sepsis (11). Therefore, the objective of this study is to evaluate the usefulness of the SOFA and qSOFA scales as a prognosis of mortality in patients with sepsis hospitalized in the intensive care unit (ICU) of the Good Hope Clinic from January to December 2015 at the end of the year. to implement them for rapid diagnosis and allocation of resources; as well as for the development of management protocols for the service.
METHODS
Design and study area
It is an analytical, observational, and retrospective study
Population and sample
The population included patients hospitalized in adult ICUs of the Good Hope Clinic with a diagnosis of sepsis in the period from January to December 2015. The sample was census type which includes all patients hospitalized in adult ICU-NICU of the Good Hope Clinic with a diagnosis of sepsis in the mentioned period.
Variables and instruments
A data collection sheet was used detailing the variables of interest to study in the population. Double data entry was performed for quality control and the dependent variable was death. The sociodemographic variables used were: sex and age. Clinical variables: days of hospitalization, prolonged stay, use of vasopressors, Glasgow scale, infectious focus, comorbidities, septic shock. And finally, the laboratory variables measured were: platelets, serum bilirubin, creatinine, blood leukocytes, number of rods, Pa/FiO2 ratio, and serum lactate. Considering vital functions such as: temperature, saturation, heart rate, respiratory rate. The SOFA and QSOFA scales are widely used worldwide for assessing the severity of patients in health institutions.
Procedures
After approval by the institution, the medical records of patients who were hospitalized in the ICU-NICU service who had the ICD-10 corresponding to septicemia with and without specifications were obtained from the statistical department.
Statistical analysis
The descriptive analysis was performed through frequencies and percentages for the qualitative variables and for the quantitative variables through measures of central tendency (mean or median) and dispersion (standard deviation and ranges) according to the normal or non-normal distribution. of the data, respectively, found in turn with the Kolmogorov-Smirnov test.
In the bivariate analysis, the association between dependent and independent variables was evaluated using chi-square tests for qualitative variables, Student's T-test for qualitative vs. quantitative variables (with normal distribution), and Wilcoxon's signed-rank test.
The analysis of the ROC curve and area under the ROC curve was performed for the SOFA and QSOFA scales. A value of p<0.05 was considered statistically significant.
Ethical aspects
The study did not contemplate intervention of any kind on the patients nor did they alter their final outcome, the data obtained from the medical records was retrospective and anonymous. Likewise, the execution of the investigation was after the approval by the Department of Teaching and Research of the Good Hope Clinic, which allowed its elaboration.
RESULTS
The 145 medical records were reviewed, obtaining a sample of 53 that met the inclusion and exclusion criteria with which the following results were obtained.
Of the total of 53 patients hospitalized in the ICU and NICU services, 58.5% were female, the average age was 76 years. The majority (66%) of the patients came from the emergency service. 49.1% had a prolonged hospital stay and the average number of days hospitalized was 14. The main source of infection was respiratory (41.5%). 9.4% (5) of the patients presented septic shock (according to the new criteria), of which 40% (2) died.
The average score according to the SOFA scale was 5.08, and for the qSOFA scale, it was 1.36. According to the SOFA scale, 49 of the 53 patients (92.5%) would enter the sepsis classification; according to qSOFA only 23 (43.4%).
The total number of deaths was 28.3%. Of the total number of patients, 84.9% had some comorbidity. (Table 1).
Table 1. Sociodemographic and clinical characteristics of the sample.
| Variable | Frequency | % |
|---|---|---|
| Total population | 53 | 100 |
| Sex | ||
| Female | 31 | 58.5 |
| Male | 22 | 41.5 |
| Age | 76±20.7* | 18-100** |
| Origin Service | ||
| Hemodynamic | 1 | 1.9 |
| Emergency | 35 | 66.0 |
| Floor | 12 | 22.6 |
| Operating Room | 5 | 9.4 |
| Days hospitalized | 14±16.9* | 1-102** |
| Prolonged stay | ||
| No | 27 | 50.9 |
| Yes | 26 | 49.1 |
| Need to use vasopressors | ||
| No | 36 | 67.9 |
| Yes | 17 | 32.1 |
| Infectious focus | ||
| Gynecological | 1 | 1.9 |
| Respiratory | 22 | 41.5 |
| Urinary | 15 | 28.3 |
| Abdominal | 15 | 28.3 |
| Septic shock | ||
| No | 48 | 90 .6 |
| Yes | 5 | 94 |
| SOFA score | 5.08±2.7* | 0-11** |
| QSOFA score | 1.36±0.9* | 0-3** |
| discharge | ||
| Voluntary | 2 | 3.8 |
| Deceased | 15 | 28.3 |
| Improved | 19 | 35 .8 |
| Stable | 17 | 32.1 |
| Pre-existing comorbidities | ||
| No | 8 | 15.1 |
| Yes | 45 | 84.9 |
For the bivariate analysis, the variables observed in the table below were considered. (Table 2). Those that showed a statistically significant association with death were age (p<0.001), days hospitalized (p<0.001), oxygen saturation (p<0.001), bilirubin (p<0.001), mean arterial pressure (p<0.001), Glasgow Coma Scale (p<0.001), creatinine (p<0.001), respiratory rate (p<0.001), temperature (p<0.001), leukocytes (p<0.001), baton cells (p<0.001), serum lactate ( p<0.001), SOFA score (p<0.001) and QSOFA score (p<0.001)
Table 2. Analysis of mortality with various variables.
| Variable | Deceased | p-value | |
|---|---|---|---|
| Yes (%) | No (%) | ||
| Sex | |||
| Female | 10(66.7) | 21(58.3) | 0.448* |
| Male | 5(33.3) | 15(41.7) | |
| Age | 86 (46-96)~ | 83.5(18-100)~ | 0.000** |
| Department of origin | |||
| Hemodynamics | 0(0) | 1(2.6) | 0.442* |
| Emergency | 11(73.3) | 24(63.2) | |
| Floor | 4( 26.7) | 8(21.0) | |
| Operating room | 0(0) | 5(13.2) | |
| Days hospitalized | 5(1-24)~ | 10(3-102)~ | 0.000** |
| Prolonged stay | |||
| No | 9(60) | 18 (47.4) | 0.407* |
| Yes | 6(40) | 20(52.6) | |
| Pa/ FiO2 | 253.9(126.6)~~ | 285.1(136.4)~~ | 0.448∞ |
| O2(%) | 93(78- 99)~ | 95.2(72.2-99.6)~ | 0.000** |
| Platelets (103/mm3) | 199.1(128.4)~~ | 256.4(126.4)~~ | 0.145∞ |
| Bilirubin serum (md/dL) | 0.5(0.2-9.6)~ | 0.62(0.1-7)~ | 0.000** |
| Mean arterial pressure (mmHg) | 66.7(48.3-123.3 )~ | 78.3(43.3-133.3)~ | 0.000** |
| Use of vasopressors | |||
| No | 10(66.7) | 26(68.4) | 0.902* |
| Yes | 5(33.3) | 12(31.6) | |
| Scale Glasgow Coma | 14(8-15)~ | 14(8-15)~ | 0.000** |
| Creatinine (mg/dl) | 1.5(0.4-4.1)~ | 0.8(0.37-3.2)~ | 0.000 ** |
| Heart rate (beats/min) | 102.5(23.1)~~ | 98.2(23.7)~~ | 0.552∞ Respiration |
| rate atory (breaths/min) | 24(14-42)~ | 22(14-37)~ | 0.000** |
| Temperature (C°) | 36.6(36.2-38.5)~ | 37.1(36-39.5 )~ | 0.000** |
| Leukocytes (103/mm3) | 11.3(3.4-46.8)~ | 13(5.3-74.6)~ | 0.000** |
| Batoned (%) | 2(0-18)~ | 0 .0(0-12)~ | 0.001** |
| Serum lactate(mmol/L) | 1.3(0.89-8.9)~ | 1.2(1-8.9)~ | 0.000** |
| infectious focus | |||
| Gynecological | 0( 0) | 1(2.6) | 0.653* |
| Respiratory | 8(53.3) | 14(36.8) | |
| Urinary | 3(20) | 12(31.6) | |
| Abdominal | 4(26.7) | 11(29.0) | |
| Pre-existing comorbidities | |||
| No | 1(6.7) | 7(18.4) | 0.282* |
| Yes | 14(93.3) | 31(81.6) | |
| SOFA Score | 6(2-11)~ | 4(0-11)~ | 0.000** |
| QSOFA Score | 2 (0-3)~ | 1(0-3) | 0.000** |
| Septic shock | |||
| No | 13(86.7) | 35(92.1) | 0.542* |
| Yes | 2(13.3) | 3(7.9) | |
~Median (minimum and maximum value) ~~Mean and standard deviation
Those variables with statistical significance after performing the Odds Ratio were: serum creatinine with an OR of 11.667 (CI 95 % 2.576-52.845, p<0.001) and serum lactate with an OR of 5.775 (95% CI 1.448-23.032, p=0.009). Based on these data, it can be interpreted that having a high creatinine, ≥1.2 mg/dl, provides 11.7 more chances of dying than normal values. Likewise, serum lactate ≥ 2mmol/L offers 5.8 more chances of dying than normal values. (Table 3) For the analysis of the Odds Ratio of SOFA and QSOFA, the value of ≥2 was taken into account for the presence of sepsis, according to the latest consensus, and its association with the death of patients.
Table 3. Odds ratio of statistically significant quantitative variables.
| Variable | OR | CI 95% | p |
|---|---|---|---|
| Age | 4.345 | 0.5-37.758 | 0.154 |
| Oxygen Saturation | 4.242 | 0.82-21.939 | 0.069 |
| Serum bilirubin | 2.125 | 0.414-10.903 | 0.359 |
| Mean arterial pressure | 0.372 | 0.6924 | 1.282 |
| Glasgow Coma scale | 1,444 | 0,418-4,986 | 0.560 |
| Serum creatinine | 11,667 | 2,576-52,845 | 0.000 |
| Breathing frequency | 1,029 | 0,311-3,407 | 0.002 |
| Leukocytes | 0,708 | 0,214-2,350 | 0.572 |
| Rod-shaped | 9,250 | 0,878-97,475 | 5,775 |
| Serum lactate | 5,775 | 1,448-23,032 | 0.009 |
| Sepsis according to SOFA | 1,441 | 1,197-1,736 | 0.191 |
| Sepsis according to QSOFA | 1.752 | 0.525-5.847 | 0.359 |
In order to know if both scales, both SOFA and qSOFA were able to discriminate patients who were going to die from those who were not, an analysis of the ROC curve (Figure 1) and area under the curve. The area under the curve for SOFA was 0.698, with p=0.026, CI=95% (0.543-0.854), being statistically significant. For qSOFA, it was 0.583, with p=0.348, CI=95% (0.422-0.745), with no statistically significant association, as shown in Table 4.
Table 4. Area under the ROC curve.
| Test result variables | Area | Standard of error | Asymptotic significance | 95% asymptotic confidence interval | |
|---|---|---|---|---|---|
| Lower Limit | Upper limit | ||||
| SOFA score | 0.698 | 0.079 | 0.026 | 0.543 | 0.854 |
| QSOFA score | 0.583 | 0.082 | 0.348 | 0.422 | 0.745 |
The Youden index was obtained from the coordinates of the curve to find the cut-off point of both scales where their sensitivity and specificity was optimal to discriminate those who were going to die of those who did not. From these results, a graph of continuous lines was obtained, the highest points of each scale were taken as cut-off points. The cut-off point for SOFA was 7.5, with 46.7% sensitivity and 86.8% specificity. For qSOFA it was 0.5, with a sensitivity of 93.3% and a specificity of 21.1%.
DISCUSSION
In our study, the majority of patients with a diagnosis of sepsis admitted to the ICU/NICU were women (58.5%), which coincides with one of the largest studies conducted in Colombia in 10 general hospitals, where 51% of the patients were women (12), although it differs from most existing studies, where the predominant sex was male (6,9,12-14). The average age was 76.1, higher than in other studies carried out in public hospitals in Peru, Colombia, Saudi Arabia and Europe - SOAP multicenter study, with 24 countries - where it was 62 (9,13,15-18)(9,13,15-18). The establishment where this study was carried out, Good Hope Clinic, has special insurance for elderly adults, with a large part of its population belonging to this age group, which would explain the increased age of the female sex, as they have a greater life expectancy (19).
The main service of origin was emergencies, 66%, and hospitalization in second place. Although the literature does not specify where the patients were before their transfer to the ICU, a study carried out in Colombia in 10 ICUs indicates that 51% of the patients developed sepsis in the community, 44% in the ICU, and 5% during hospitalization (20).
The average stay was 14 days; this data considers both days in the ICU and out of it. Slightly higher than studies in Colombia (12) and Cuba (18) with 10 days and Saudi Arabia with 12 (16), but considerably lower than in Madrid, where one study showed an average stay of 28.9 days (6). A little less than half of the population had a prolonged stay (49.1%), which implies a high cost in health (6).
The main source of infection was respiratory in 41.5% of patients, followed by abdominal and urinary sources in 28.3% of patients. These results coincide with the epidemiology of studies carried out in Chile (13), with 48% respiratory and 30% abdominal, in Saudi Arabia (16), 69.5% respiratory focus, and in the aforementioned SOAP study (17), 68% respiratory, and 22% pulmonary. However, they oppose the data from the Hospital Edgardo Rebagliati Martins (HERM) in Lima, where the main focus was abdominal (9), as in Mexico (7). This can respond to several factors. First, as explained above, our study was conducted in a private clinic, where the population is older and similar to that of more economically developed countries. This could explain the similarity of the results. Secondly, it should be noted that, in the study carried out at HERM, most ICU patients came from the operating room, unlike our study. Of the total number of patients with sepsis, 9.4% met the criteria for septic shock. Of these, 40% died. The lethality in our study was higher than that presented in studies at the Hospital Nacional Hipólito Unanue (HNHU): 21.5% (15) and at a Hospital in Pereira-Colombia, with 33% (21), however similar to that of a multicenter study in Colombia with a rate of 45.6% of patients with septic shock (12).
The average score on admission to the ICU according to the SOFA scale was 5.08 and 1.36 for qSOFA. Regarding the SOFA score, this is very similar to the study carried out in the HNHU(15), with a value of 5, and to that of the multicenter study carried out in Chilean ICUs: 6; but well below that obtained in the HERM: 16.4 (9).
Mortality was 28.3%, considerably lower than in other studies, exceeding 50% (9,21,22). Taking into account the previous results, we could deduce that those studies where the average SOFA score was higher, so was the mortality rate.
According to these scales, 92.5% of the patients were classified as having sepsis according to SOFA, and only 43.4% according to qSOFA. This is because the use of these classifications as diagnostic criteria is not yet institutionalized and has been recommended as of 2016, while the study was carried out with data from 2015. According to the Third International Consensus on Definitions for sepsis and septic shock, the predictive validity for in-hospital mortality for SOFA was statistically superior to SIRS and QSOFA, supporting its use as a clinical criterion for sepsis. Among cases with suspected infection outside the ICU, the predictive validity for in-hospital mortality of qSOFA was statistically higher than SOFA and SIRS, supporting its use as a prognostic to consider possible sepsis (23).
84.9% of the patients presented some comorbidity. This percentage is slightly higher than in other studies (9), however, as we mentioned before, this responds to the characteristics of an aging population.
After finding the Odds Ratio, we concluded that the variables that showed a statistical association with mortality were creatinine, with an OR of 11.667 (95% CI 2.576-52.845, p<0.001) and serum lactate, with an OR of 5.775 (CI 95%1,448-23,032, p=0.009).
In order to assess kidney damage to obtain the SOFA score, the creatinine level was used. The appearance of acute renal failure in seriously ill patients shows that, despite the advances in renal replacement therapy, mortality from this condition in most studies exceeds 50%, and in recent years, it has remained unchanged. In a study carried out in Cuba, daily determination of serum creatinine and measurement of hourly diuresis were performed. 16.2% of the patients were complicated by kidney failure. Those who preserved urinary volume had a better prognosis in terms of recovery, the shock was the main cause of this condition, and lethality was 30% (24).
In a study carried out in Mexico, serum lactate levels were evaluated as a predictor of mortality in patients with septic shock, where it was found that patients with lactate levels greater than 4.9 mmol/L have a probability of dying 8.7 times greater than those with a lactate level below 4.9 mmol/L (95% CI, 1.03-72.3) (25). In the context of sepsis, “elevated serum lactate is due to an imbalance between genesis and clearance. A state of important tissue hypoperfusion blocks the synthesis of ATP by blocking the enzyme pyruvate dehydrogenase due to hypoxia with the deviation of the equation from Pyruvate to Lactate. Clearance is diminished due to poor metabolism of lactate in the liver and muscles, the main organs responsible for this, in addition to a greater flow of the amino acid alanine (result of pyruvate and glutamate) to the liver, and direct defects at the level of metabolism oxidative activity at the mitochondrial level due to the direct action of endotoxins and inflammatory mediators (TNF, NO, among others), leading to greater production of lactate due to accumulation and mass effect of its precursor”(26).
The presence of sepsis according to the SOFA or qSOFA scales showed a statistically significant association to predict mortality, with a cut-off point of 2. However, after finding the area under the curve, the SOFA scale was statistically significant (p=0.026), AUC -ROC=0.698, 95% CI (0.543-0.854). In other words, there is a 70% probability that it will adequately discriminate patients who are going to die from those who are going to survive. After finding the Youden Index, the cut-off point where the scale obtains the maximum sensitivity: 46.7% and specificity: 86.8% is from 7.5 points. This means that the scale was effective in identifying those patients with a lower probability of dying. The AUC-ROC was similar to that found in the study carried out in HNHU: 0.74 (15) and in the Hermanos Ameijeiras Hospital in Cuba: 0.782 (18). In a study conducted in Chimbote, the cut-off point found for SOFA was 10, with a sensitivity of 34% and a specificity of 89% (27), similar to ours. For a study carried out in Cuba, the SOFA was applied at 24 and 48 hours after admission, AUC-ROC of 0.85 and 0.95, respectively, with an accuracy percentage of 76, 9% for cut-off points ≥ 2 and 91, 4% for cut-off point ≥ 3, respectively. No reference literature was found for QSOFA as it is a new scale. In our study, no statistical significance was found, since this tool was designed primarily for an environment outside of intensive care, where coincidentally, SOFA has been shown to have inadequate performance (28). One of the limitations of our study was the small population, for which it is recommended that this study be replicated in large national hospitals. Take into account the use of a mechanical ventilator as a variable, since its presence increases the risk of mortality (29)
CONCLUSIONS
- In our study, the main source of infection was respiratory, in 41.5% of patients.
- 9.4% presented septic shock, according to the new criteria; 40% of them died.
- Of the total number of hospitalized patients diagnosed with sepsis, 28.3% died.
- The factors that showed a statistically significant association with mortality were serum creatinine with a value ≥1.2 mg/dl and serum lactate ≥2 mmol/L.
- Only the SOFA scale showed a statistically significant association with an area under the curve of 0.698, with p=0.026, CI=95% (0.543-0.854). The cut-off point where the scale obtains the maximum sensitivity: 46.7% and specificity: 86.8% is from 7.5 points. Therefore, it obtained a low sensitivity and a high specificity. Studies with a higher SOFA score showed a higher mortality rate, so it is important to know how to identify the early appearance of sepsis diagnostic criteria in time for prompt referral to the ICU and thus avoid fatal complications.
ACKNOWLEDGMENTS
We thank Dr. Jhonny de la Cruz who was advisor and director of the thesis of the research work presented.
Authorship contributions: OSM participated in creating the research idea, methodology, resources, and writing of the final manuscript. KGM participated in the conceptualization and drafting of the final manuscript.
Funding sources: Self financed
Conflicts of interest: The authors declare no conflict of interest.
Received: July 11, 2022
Approved: September 13, 2022
Correspondence: Ottavia Scarsi Mejía.
Address: Av. Alfredo Benavides 5440, Santiago de Surco 15039. Lima - Peru.
Telephone number: +51956013475
E-mail: vosm_23@hotmail.com
Article published by the Journal of the faculty of Human Medicine of the Ricardo Palma University. It is an open access article, distributed under the terms of the Creatvie Commons license: Creative Commons Attribution 4.0 International, CC BY 4.0(https://creativecommons.org/licenses/by/1.0/), that allows non-commercial use, distribution and reproduction in any medium, provided that the original work is duly cited. For commercial use, please contact revista.medicina@urp.edu.pe.
REFERENCES