CASO CLÍNICO
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2022 - Universidad Ricardo Palma10.25176/RFMH.v22i4.5107
CHARCOT NEUROARTHROPATHY: DIFFERENTIAL DIAGNOSIS OF MONOARTHRITIS OF THE KNEE IN PATIENTS WITH TYPE 2 DIABETES MELLITUS
NEUROARTROPATÍA DE CHARCOT: DIAGNÓSTICO DIFERENCIAL DE MONOARTRITIS DE RODILLA EN PACIENTES CON DIABETES MELLITUS 2
Gino Patrón-Ordóñez1,2,a, María Isabel Anticona-Sayánb
1Instituto de investigaciones en ciencias biomédicas, Facultad de medicina Humana. Universidad Ricardo Palma, Lima - Perú.
2Hospital Nacional Dos de Mayo - Sala de Medicina Julián Arce. Lima, Perú.
aPhysician internist.
bEndocrinologist.
ABSTRACT
Clinical case: A 46-year-old man with long-standing, poorly controlled diabetes is hospitalized for right knee monoarthritis after trauma. His clinical evaluation found joint deformity, synovitis in the right knee, and absence of multiple toes due to a history of amputation. With the radiological evaluation that showed bone destruction and the synovial fluid analysis that ruled out infectious causes and microcrystal arthritis, the diagnosis of Charcot neuroarthropathy of the knee was made. Discussion: Conservative management was indicated with the use of a felt insole for unloading and the use of a walker, the case being followed up to define behavior according to evolution. Conclusion: Despite being rare, it is important to consider Charcot neuroarthropathy in all diabetic patients with monoarthritis of the knee, to make an early diagnosis and avoid important complications and sequelae, always ruling out infectious causes and arthritis due to microcrystals.
Keywords: Neurogenic arthropathy, Charcot's joint, Diabetes complications, Diabetic neuropathies, monoarthritis. (Source: MeSH NLM).
RESUMEN
Caso clínicoVarón de 46 años, diabético mal controlado y de larga evolución es hospitalizado por monoartritis de rodilla de derecha posterior a traumatismo. Su evaluación clínica encontró deformidad articular, sinovitis en rodilla derecha y ausencia de múltiples ortejos por antecedentes de amputación. Con la evaluación radiológica que mostró destrucción ósea y el análisis de líquido sinovial que descarto causas infecciosas y artritis por microcristales se hizo el diagnóstico de neuroartropatía de Charcot de rodilla. DiscusiónSe indico manejo conservador con uso de plantilla de fieltro para descarga y uso de andador, quedando el caso en seguimiento para definir conducta según evolución.Conclusión A pesar de ser poco frecuente, es importante el planteamiento de neuroartropatía de Charcot en todo paciente diabético con monoartritis de rodilla, con el fin de hacer un diagnóstico precoz y evitar complicaciones y secuelas importantes, debiendo hacerse siempre el descarte de causas infecciosas y artritis por microcristales.
Palabras Clave: Artropatía neurógena, articulación de Charcot, complicaciones de la diabetes, neuropatías diabéticas, monoartritis. ( Fuente: DeCS - BIREME).
INTRODUCTION
Charcot's neuroarthropathy is a chronic, destructive, and deforming arthropathy that mainly affects diabetic patients and begins with the development of peripheral neuropathy, which, when accompanied by mechanical, vascular, and inflammatory factors, progressively destroys the joint. Its prevalence in diabetic people is variable, registering even 35%, and mainly affects the foot (64%) and ankle (24%), being rare its presentation in the knee (6%), which means that the diagnosis can go unnoticed, delaying treatment and leading to significant sequelae, including increased mortality(1-4).
We present the case of a long-term poorly controlled diabetic patient who presented monoarthritis of the knee and in whom a diagnosis of Charcot's neuroarthropathy was made after clinical and radiological evaluation and the ruling out of other monoarthritis causes. This case report was prepared following the recommendations of the CARE guide.
DESCRIPTION OF THE CLINICAL CASE
We present the case of a 46-year-old man, natural and from Lima-Peru, with type 2 diabetes mellitus for 17 years, in irregular treatment with insulin glargine U100, 20 IU a day, with a history of surgical amputation of multiple toes due to diabetic foot conditions, who went to the hospital for presenting for 2 months and after a fall, progressive increase in the volume of the right knee that It is accompanied by mild to moderate pain that made it difficult for him to walk, for this reason, he was hospitalized with an initial diagnosis of monoarthritis of the knee.
General examination revealed multiple hypochromic macules and loss of hair on the skin of the lower limbs, in addition to a superficial ulcer on the sole of the left forefoot at the level of the fifth metatarsophalangeal joint. Muscular hypotrophy of both legs was found in the locomotor examination, in the right knee an increase in volume and deformation was observed with signs of joint effusion accompanied by an increase in temperature and without erythema, a hard and mobile mass of approximately 2cm in the region was also palpated in the external femoral condyle. The absence of the fourth and fifth toes of the right foot and the second and third toes of the left foot was also evident due to what was already mentioned. (Figure 1).

The vascular examination found pulses present in the pedal, posterior tibial, and popliteal arteries with a normal bilateral ankle-brachial index, while the neurological examination revealed hypoesthesia, apelesthesia, and hyporeflexia of the lower limbs. Fundus evaluation was positive for bilateral non-proliferative diabetic retinopathy. The rest of the physical examination showed no significant alterations. The blood count showed moderate normochromic normocytic anemia, normal leukocytes and platelets, glycemia reached values of 300mg/dL, HbA1C 11%, a glomerular filtration rate was calculated at28mL/min/1.73m2, the urinalysis revealed proteinuria and glycosuria, while serum uric acid and C-reactive protein were normal.
Arthrocentesis of the right knee was performed, obtaining 50 ml of slightly turbid synovial fluid with preserved viscosity, the analysis showed a non-inflammatory fluid with 2 leukocytes/mm3 (100% mononuclear), red blood cells 40/mm3, no crystals were found, while studies microbiological gram stain, Ziehl-Neelsen and cultures were negative for common germs and mycobacteria (Figure 2).

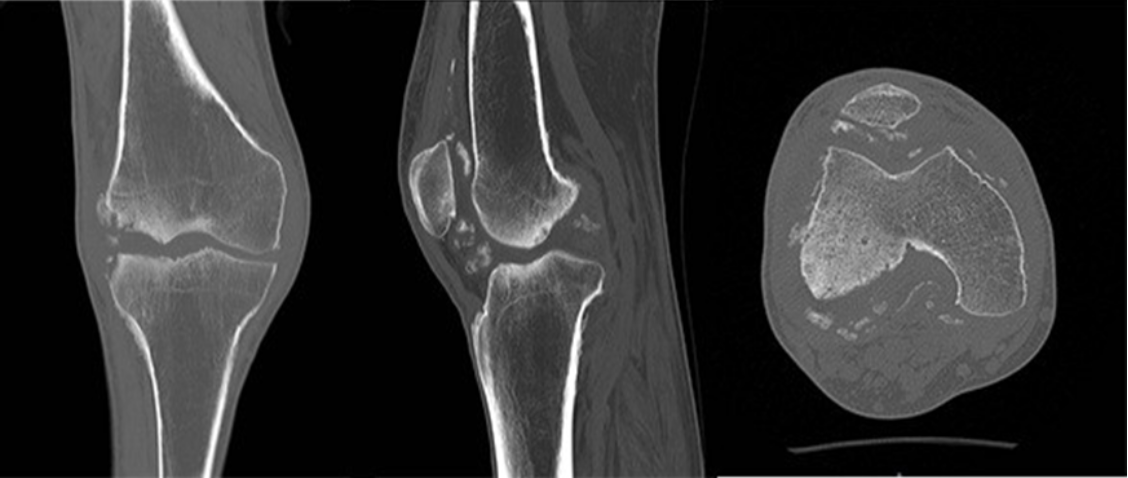
Right knee ultrasound revealed moderate joint effusion without synovial hypertrophy with internal calcifications in the menisci and bone erosions of the external femoral condyle. The X-ray showed signs of bilateral osteoarthritis of the knees and loss of bone continuity in the right external femoral condyle, while the tomography confirmed the findings, also finding destruction of the right external tibial plateau and multiple bone fragments (Figures 3 and 4).

Based on the history of diabetes mellitus 2 with the presence of multiple chronic complications, as well as the findings of a non-inflammatory synovial fluid, the ruling out of diseases such as infectious arthritis and microcrystals, as well as the presence of joint deformation with bone erosions, is that the diagnosis of Charcot neuroarthropathy of the knee is made. Management of glycemia with insulin was optimized in addition to analgesic therapy and conservative management was indicated through the use of a felt insole for weight-bearing and a walker, which reduced pain and improved mobility, managing the case on an outpatient basis by physical medicine. and traumatology to define behavior according to evolution.
DISCUSSION
Charcot's neuroarthropathy is a chronic, destructive, and deforming joint pathology, related to the previous development of neuropathy and initially associated with late neurosyphilis, however, currently diabetic neuropathy is its most associated cause, also being described secondary to syringomyelia, syndrome of Guillain-Barré among others, even describing idiopathic cases(5,1). It affects patients with diabetes mellitus between 50 and 60 years of age and after 10 years of disease, with a variable prevalence in them, with reports ranging from 0.1 to 35%, associating its presence with lower survival.
It compromises the joints usually unilaterally and more frequently at the foot (64%) and ankle (24%), being rare in other locations such as the hand (6%) and knee (6%), the latter location has been more specific in type 1 diabetes (1-3,6).
The following factors intervene in its pathophysiology: a) neuro-traumatic, where sensory loss increases joint overload and leads to undetected microtraumas in the joint, which eventually produces deformity; b) neuro-vascular, where the loss of sympathetic tone due to autonomic neuropathy produces an increase in blood flow causing osteolysis and bone resorption; c) inflammatory, where an increase in IL-1β, IL-6 and TNF-α would lead to increased osteoclast activity due to overexpression of the receptor activator ligand for nuclear factor kappa-B (RANKL) added to a decrease in osteoprotegerin activity (2,4).
Charcot neuroarthropathy of the knee, as well as that of other locations, usually presents after a traumatic trigger, with the subsequent appearance of pain, effusion, and joint deformity, depending on the evolutionary stage. With regard to pain, this may be absent in 50% of cases due to neuropathy and does not usually correspond to the degree of bone and joint destruction, as occurred with our patient (1,7). Despite the neuro-traumatic and neuro-vascular factors being involved in the pathophysiology, when the knee is affected, the former predominates, as could have occurred in the case presented, since the presence of neuropathy causes a progressive alteration in gait, which increases the joint overload and produces repetitive microtraumas, leading to joint deformation(7,8).
Diagnosis is based on the clinical history and physical examination, however, there may be a delay in diagnosis between 25%-79% of cases, on physical examination signs of peripheral neuropathy, joint deformity, and signs of arthritis, where the mere increase in temperature over the joint has been shown to be an important predictor of the development of Charcot's neuroarthropathy. Sometimes the presence of foot ulcers can be found in pressure areas, which was also evidenced in the case presented where the absence of multiple toes due to a history of amputation was also noted, this contributed to the neuro-traumatic factor altering the overload of the affected knee(1,7,9). In addition to the clinic, imaging evaluation is important, where plain radiography is the diagnostic method of choice, allowing evaluation of the evolutionary stage and bone involvement, however, there is a preclinical phase in which radiographic changes could take up to 3 weeks, in these cases magnetic resonance imaging is useful in the search for early signs of Charcot neuroarthropathy. According to the clinical and radiological involvement, Charcot's neuroarthropathy can be classified according to Eichenholtzen into 4 evolutionary phases, which serve to guide treatment (Table 1).
Table 1. Eichenholtz classification.
| Stage | Radiographic findings | Clinical findings |
|---|---|---|
| 0-Prodromal or inflammatory | No bone abnormalities | Edema, erythema, heat |
| I-In development | Osteopenia, bone fragmentation, subluxation, dislocation | Edema, erythema, warmth and ligamentous laxity |
| II-Coalescence | Absorption and fusion of bone fragments, osteosclerosis | Decrease in inflammatory signs |
| III-Reconstruction | Joint deformity and ankylosis | Joint deformity and absence of inflammatory signs |
According to clinical findings, the case presented would correspond to stage II or coalescence, with radiological studies presenting bone fragments in the process of fusion (1,4,6,8,10,11).
It is also important to rule out other pathologies, being necessary in the specific case of knee involvement the differential diagnosis of other causes of monoarthritis, such as infectious arthritis, microcrystal arthritis, and osteomyelitis, as was done in the case presented, where the studies synovial fluid were negative for germs and crystals, and no elevation of acute phase reactants or leukocytosis was found that could suggest another etiology. In cases where there is doubt in ruling out osteomyelitis, magnetic resonance imaging is recommended, which has a sensitivity of 77% and a specificity of 80% to differentiate it from Charcot neuroarthropathy, if it cannot be differentiated by magnetic resonance it is Scintigraphy with labeled leukocytes is useful. For specific cases, a histopathological study may be necessary (1,7,12).
Due to the few reported cases and the multiple etiologies it may have, the management of Charcot neuroarthropathy of the knee is controversial and must be individualized, ranging from conservative management with knee immobilization and the use of orthoses to prevent skeletal destruction and deformity, to total arthroplasty, in the latter case there may be complications derived from bone fragility and ligament laxity such as periprosthetic fractures, instability as well as infections, however, it could be used in selected cases such as coalescence and reconstruction stages. The indication of arthrodesis could be an alternative in cases of arthroplasty failure. In our case, the indication of a felt insole in the left foot to reduce the discharge in the affected area, as well as the use of a walker, reduced pain and improved mobility, with the patient being followed up to define the behavior according to its evolution(1,7,10,11,13).
Other treatment options, based on the proposed pathophysiological mechanisms of increased bone resorption and the presence of inflammatory mediators, are the use of bisphosphonates and monoclonal antibodies, however, they have not shown a strong clinical beneficial effect(2,4).
In conclusion, the presentation of Charcot neuroarthropathy of the knee is rare and should be considered in all patients with diabetes mellitus with monoarthritis of the knee, especially in the presence of peripheral neuropathy, always differentiating it from other causes such as infectious arthritis and microcrystals. Early diagnosis is important to prevent fractures and joint deformation, which are also associated with a higher risk of amputation and mortality. Due to the few reported cases, the treatment is controversial, and the evolutionary stage of the disease must be assessed and can range from conservative management to total arthroplasty.
Authorship contributions: GPO: Conceptualized, reviewed literature, wrote the initial draft, and wrote and revised the final version. MIAS: Conceptualized, reviewed the bibliography, wrote the initial draft, wrote and revised the final version.
Funding sources: Self-financed.
Conflicts of interest: The authors declare that they have no conflicts of interest.
Received: September 16, 2022
Approved: October 13, 2022
Correspondence: Gino Patron-Ordóñez.
Address: Av. Benavides 5440. Universidad Ricardo Palma. Santiago de Surco - Lima 33.
Telephone number: 986621481
E-mail: gino.patron@urp.edu.pe
Article published by the Journal of the faculty of Human Medicine of the Ricardo Palma University. It is an open access article, distributed under the terms of the Creatvie Commons license: Creative Commons Attribution 4.0 International, CC BY 4.0(https://creativecommons.org/licenses/by/1.0/), that allows non-commercial use, distribution and reproduction in any medium, provided that the original work is duly cited. For commercial use, please contact revista.medicina@urp.edu.pe.
REFERENCES
