ARTICULO ORIGINAL
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2022 - Universidad Ricardo Palma10.25176/RFMH.v22i4.5170
FACTORS THAT INTERFERE SCREENING FOR GYNECOLOGICAL CANCERS IN PERUVIAN WOMEN
FACTORES QUE INTERFIEREN LOS CRIBADOS PARA CÁNCERES GINECOLÓGICOS EN MUJERES PERUANAS
Silva-Lopez M1,a, Rodrigo-Alvarado W1,a, Rubén Espinoza-Rojasbc, Manuel Loayza Alarico1,a,c Patricia Segura-Nuñez1,d
1Research Institute in biomedical sciences. Faculty of human medicine. Ricardo Palma University.
aMedical surgeon
bGraduate in statistics
cPh.D. mg
dPulmonologist
ABSTRACT
Objective: To identify the factors associated with the interference of screening for gynecological cancers in Peruvian women aged 25-69 years, according to the Demographic and Family Health Survey (ENDES) of the years 2019 and 2020. Materials and methods: Quantitative, observational study, analytical cross-section. It was an analysis of the secondary database obtained by ENDES for the years 2019 and 2020. Raw and adjusted Poisson family generalized linear models were used to estimate the association. The association measure used was the adjusted prevalence ratio (APR) with a 95% confidence interval (95%CI). Results: We worked with 18,113 Peruvian women aged 25-69 years in the ENDES 2019-2020. In the descriptive analysis, it is observed that 19.3% did not have a Papanicolaou test (PAP), and 53.6% did not undergo "screening for breast cancer." Women with a primary education level have 20% and 58% more opportunities to present interference for taking PAP and screening for breast cancer, respectively (RPa: 1.20, CI95%: 1.09-1.32 and RPa: 1.58, CI95%: 1.52- 1.65). Living in the jungle increases by 57% and 20% more opportunities to present interference for taking PAP and screening for breast cancer, respectively (RPa: 1.57, CI95%: 1.43-1.71 and RPa: 1.20, CI95%: 1.15-1.25 ). The level of knowledge increases the interference for taking PAP tests and screening for breast cancer by 44% and 4%, respectively (RPa: 1.44, CI95%: 1.34-1.54 and RPa: 1.04, CI95%: 1.01-1.07). Conclusion: Sociodemographic, sociocultural and economic factors have a marked influence on screening for gynecological cancers such as cervical and breast cancer, so it is necessary to implement strategies to promote the prevention of these pathologies.
Keywords: Papanicolaou; Clinical Breast Examination; Mammography; screening; Cervical cancer; Breast cancer. (Source: MeSH NLM).
RESUMEN
Objective: To identify the factors associated with the interference of gynecological cancer screening in women aged 25-69 years, according to the Demographic and Family Health Survey (ENDES) for the years 2019 and 2020. Materials and methods: Quantitative, observational, analytical cross- sectional study. It was a secondary database analysis obtained by ENDE for the years 2019 and 2020. Generalized linear Poisson family crude and adjusted models were used to estimate the association. The measure of association. The measure of association used was the adjusted prevalence ratio (Rpa) with 95% confidence interval (95% CI). Results: We worked with a total of 18,113 women aged 25-69 who were interviewed at the ENDES 2019-2020. In the descriptive analysis, it is observed that 19.3% did not take a PAP smear (PAP) and 53.6% did not perform “screening for breast cancer”. Women with a primary education level have 19% and 58% more opportunities to present interference for taking PAP and screening for breast cancer respectively (RPa: 1,19, 95% CI 1.08-1,31 and RPa:1.58, 95% CI 1:51 – 1:64). Living in the jungle increases 56%and 20%more chance of presenting interference for taking PAP and screening for breast cancer respectively (RPa: 1.46, 95% CI 1.42-1.71 and RPa: 1.20, 95% CI: 1.15- 1.25). The level of knowledge increases the interference for taking PAP and screening for breast cancer by 43% and 3% respectively (RPa: 1.43, 95% CI: 1.34- 1.54 and RPa: 1.03, 95% CI:1.00 -1.06) Conclusions: Sociodemographic, sociocultural and economic factors have a marked influence on the performance of gynecological cancers such as cervical cancer and breast cancer, so it is necessary to implement strategies to promote the prevention of these pathologies.
Palabras Clave: Papanicolaou; Clinical Breast Exam; Mammography; Screening; Cervical cancer; Breast cancer. (fuente: DeCS BIREME).
INTRODUCTION
The incidence and mortality of cancer have been increasing; it is estimated that there are 50.9 million people living with cancer according to the report given by the global cancer observatory (GLOBOCAN 2020), the most diagnosed cancer is breast cancer.(1) In Peru, there are various health problems; the most important/critical are gynecological cancers, with greater emphasis on breast and cervical cancer (CC). Currently, these two entities constitute one of the main causes of mortality in Peruvian women.(2)
The World Health Organization (WHO) considers that adequate screening would be related to a reduction in incidence and mortality for the pathologies described.(3) Among the main screening tests for gynecological cancers in our environment are: Taking a Pap smear, performing a clinical breast exam, and performing a mammogram, which is important for the early diagnosis of cervical cancer and cervical cancer. which constitutes one of the main causes of mortality in the female population.(2)
It has been shown that adequate screening reduces the incidence and mortality of gynecological cancers. We define screening as timely care performed before the onset of symptoms or the development and progression of pathologies, for this, there are various prevention methods, such as those previously described, characterized by their high efficacy and low cost for the patient; these include the Pap smear, which evaluates the presence of normal or abnormal cells present on the surface of the cervix; the clinical breast exam, which allows evaluating some anatomical alterations of the breasts; and mammography, which consists of an imaging test performed with X-rays, which allows evaluating structural alterations of the breast tissue.(4)
In Peru, there has been high mortality from cervical cancer and breast cancer; much of this has been related to a weak screening system, which sociodemographic, sociocultural, and economic factors influence.(2) Therefore, an exhaustive analysis of the development of the various strategies adopted is imperative.
This article seeks to determine and analyze the factors that influence the interference of screening for gynecological cancers. To measure the variable "Screening for gynecological cancers," we used the variables Pap smear (PAP) and screening for breast cancer (which contains two variables: clinical breast examination and mammography) in women aged 25-69 years, based on the Demographic and Family Health Survey (ENDES) 2019-2020.
METHODOLOGY
Design and study area
A quantitative, observational, analytical, and cross-sectional study was carried out. The Demographic and Family Health Survey (ENDES) database of 2019 and 2020 is used. The ENDES is an annual survey by the National Institute of Statistics and Informatics (INEI) that aims to obtain information on the demographic and health status of mothers and children under five.
Population and sample
The population is made up of women between the ages of 25 and 69 residing in Peru in the years 2019 and 2020. The sample frame is made up of statistical and cartographic information derived from the interviews developed by ENDES in those years.
As inclusion and exclusion criteria, women between 25 and 69 years of age who fully answered the survey conducted by ENDES and who provide reliable information to define the presence or absence of the variables under study were included; and women who did not correspond within the mentioned ages and who answered the survey incorrectly were excluded.
The sample size was calculated using the ENDES free access survey of the years 2019 and 2020. The initial sample was 18,488 women, of which, considering the inclusion and exclusion criteria, a final sample of 18,113 women aged 25 to 69-year-old residents in private homes and interviewed in the ENDES 2019 and 2020, who were asked if the gynecological screenings were carried out, which are: Pap smear, clinical breast exam and mammography.
Techniques and data collection instrument
For the execution of this study, a secondary data source collected by the National Institute of Statistics and Informatics (INEI)(5)(6) was used, then the page https://www. inei.gob.pe/bases-de-datos/ and the databases corresponding to the Demographic and Family Health Survey of the year 2019 and 2020 were downloaded, which were: CSALUD01, REC0111, RE223132 and RE516171 in SPSS 26 format, whose information it contained the pertinent and necessary variables to carry out the analysis and test the hypotheses proposed.
Ethical aspects
This article had the approval of the ethics committee of the Ricardo Palma University. Likewise, the ENDES 2019-2020 Secondary Database is unnamed, complying with the confidentiality of the information.
RESULTS
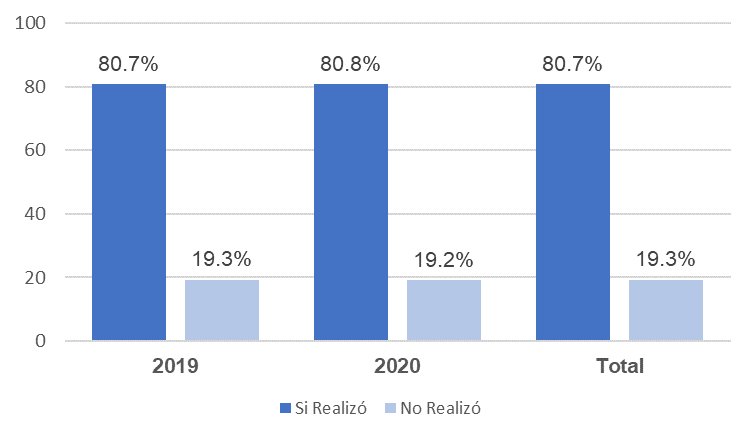
In Figure 1, the databases for the years 2019 and 2020 were joined, where it was found that 19.3% of women between the ages of 25 and 69 did not have a Pap smear, likewise, no significant difference in taking Pap smears between 2019 (19.3%) and 2020 (19.2%).
Regarding the screening for breast cancer for the year 2019-2020, as shown in graph N°2, it was found that 54.9% of women aged 25 to 69 years did not undergo any screening for breast cancer Likewise, in 2019, 53.6% did not undergo any screening for breast cancer and this percentage for 2020 increases to 56.5%.
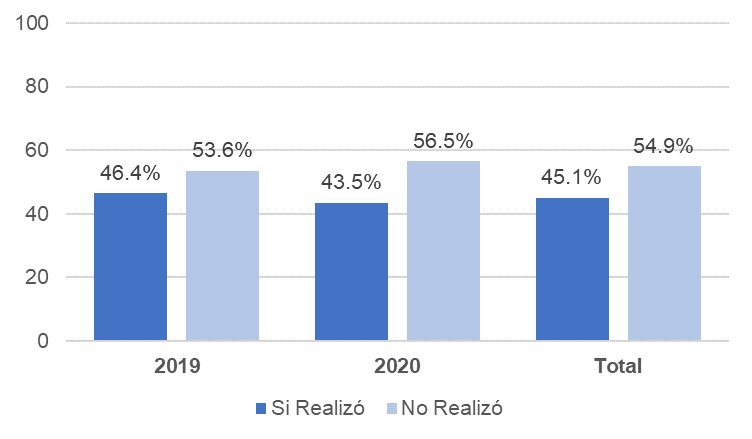
Table 1 presents the general characteristics of our sample, where it is highlighted that in relation to sociodemographic factors, 66% are under 40 years of age, 40.6% have secondary education, 67.1% are married, 60.8% live on the coast, 80.5% live in urban areas and 77.2% have health insurance; With respect to sociocultural factors, 55.1% have the age of beginning sexual relations to have been greater than or equal to 18 years, 60.5% use some contraceptive method and 81.4% have some level of knowledge about screening for gynecological cancers; As an economic factor, we find that 59% do not belong to the poverty level. Regarding the size of the sample for the present analysis, the coefficient of variation was obtained and, as can be seen in Table 1, all are less than 15%, therefore, the sample size is adequate for our study and provides us with results. reliable.
Table 1. General characteristics of women aged 25 to 69 in Peru, ENDES 2019-2020.
| Count | % | Coefficient of Variation (%) | ||
|---|---|---|---|---|
| Total | 18,113 | 100.0 | 8.9 | |
| Sociodemographic Factors | ||||
| Age | ≥ 40 years | 6,163 | 34.0 | 9.4 |
| < 40 years | 11,950 | 66.0 | 8.8 | |
| Grade of Education | Primary | 3,562 | 19.7 | 8.7 |
| Secondary | 7,354 | 40.6 | 9.4 | |
| Superior | 7,198 | 39.7 | 12 | |
| Marital Status | Married | 12,153 | 67.1 | 8.7 |
| Not married | 5960 | 32.9 | 9.7 | |
| region | Coastal | 11008 | 60.8 | 13.9 |
| Sierra | 4661 | 25.7 | 7.8 | |
| Jungle | 2445 | 13.5 | 8.6 | |
| Place of residence | Urban | 14575 | 80.5 | 10.6 |
| Rural | 3538 | 19.5 | 12.7 | |
| Health insurance | Yes | 13978 | Level | knowledge |
| _ | of | _ | _ | |
| _ | ||||
| _ | _ | _ | _ | _ |
| _ | _ | _ | _ | |
| _ | _ | _ | _ | _ |
| _ | _ | _ | _ | |
| _ on Gynecological Screenings | Knows | 14746 | 81.4 | 8.9 |
| Does not know | 3368 | 18.6 | 10.5 | |
| Economic Factor | ||||
| Poverty | No | 10727 | 59.2 | 12.3 |
| Yes | 7386 | 40.8 | 7.5 | |
In Table 2 it is evident that being under 40 years of age increases the interference for taking pap smears by 1.74 (RPa: 1.74, 95% CI: 1.61-1.87); women with primary education have 1.2 more times of presenting interference for taking pap smears (RPa: 1.20, 95% CI: 1.09-1.32); being unmarried is 1.62 more likely to have interference in taking a pap smear (RPa: 1.62, 95% CI: 1.52-1.74); living in the mountains and jungle increases the interference for taking pap smears by 1.33 and 1.57, respectively (RPa: 1.33, CI95%: 1.23-1.44 and PR: 1.57, CI95%: 1.43-1.71); residing in a rural area presents a prevalence ratio of 1.19 of presenting interference for taking pap smears (PRa 1.19, 95% CI: 1.09-1.29); not having health insurance increases the prevalence of interference for taking pap smears by 1.58 (RPa 1.58, 95% CI: 1.48-1.68); not using a contraceptive method increases the interference for taking pap smears by 1.23 (RPa 1.23, 95% CI: 1.15-1.31); women who do not have any knowledge about pap smears have 1.44 more times of presenting interference for taking pap smears (RPa 1.44, 95% CI: 1.34-1.54); and belonging to the poverty level increases the interference for taking pap smears by 1.21 (RPa 1.21, 95% CI: 1.11-1.31), adjusting for the other variables.
On the other hand, women with a secondary education level and who began sexual relations before the age of 18 did not have a significant association with interference in taking Pap smears, with a p-value >0.05.
Table 2. Analysis of multiple variables on the factors associated with interference in taking Pap smears in women aged 25-69 years according to ENDES 2019-2020.
| Pap | ||||||
|---|---|---|---|---|---|---|
| Test Associated Factors | Adjusted PR (Pap Test) | Confidence Interval Adjusted PR (95%) | P Value | |||
| Lower | Upper | |||||
| Sociodemographic factors | ||||||
| Age | < 40 years | 1.74 | 1.61 | 1.87 | 0.00 | * |
| ≥ 40 years | 1 | Reference | ||||
| Level of Education | Primary | 1.20 | 1.09 | 1.32 | 0.00 | * |
| Secondary | 0.94 | 0.86 | 1.02 | .067 | ||
| Higher | 1 | Reference | ||||
| Marital Status | Not married | 1.62 | 1.52 | 1.74 | 0.00 | * |
| married | 1 | Reference | ||||
| Region | Sierra | 1.33 | 1.23 | 1.44 | 0.00 | * |
| Jungle | 1.57 | 1.43 | 1.71 | 0.00 | * | |
| Coast | 1 | Reference | ||||
| Place of | Rural | 1.19 | 1.09 | 1.29 | 0.00 | * |
| urban | 1 | Reference | ||||
| Health Insurance | No | 1.58 | 1.48 | 1.68 | 0.00 | * |
| Yes | 1 | Reference | ||||
| Sociocultural Factors | ||||||
| Beginning of Sexual Relations | < 18 years | 1.00 | 0.94 | 1.07 | 0.99 | |
| ≥ 18 years | 1 | Reference | ||||
| Contraceptive Method | Does not use | 1.23 | 1.15 | 1.31 | 0.00 | * |
| Uses | 1 | Reference | ||||
| Level of Knowledge | Does not know | 1.44 | 1.34 | 1.54 | 0.00 | * |
| Knows | 1 | Reference | ||||
| Economic Factors | ||||||
| Poverty | Yes | 1.21 | 1.12 | 1.31 | 0.00 | * |
| No | 1 | Reference | ||||
Table 3 in the results obtained in factors that interfere with screening for breast cancer it is evident that women with primary and secondary education have 1.58 and 1.42 more times of presenting interference for performing breast screening (RPa: 1.58, CI95%: 1.52-1.65 and RPa: 1.42, CI95%: 1.37-1.47) ; living in the mountains and jungle increase the interference to carry out breast screening in a similar way by 1.21 and 1.20 (RPa: 1.21, CI95%: 1.17-1.25 and RPa: 1.20, CI95%: 1.15-1.25); not having health insurance increases the prevalence of interference for performing breast screening by 1.06 (RPa 1.06, 95% CI: 1.03-1.09); women who do not have any knowledge about gynecological screenings have 1.04 more times to present interference for breast screening (APR 1.04, 95% CI: 1.01-1.07); and belonging to the poverty level increases the interference for breast screening by 1.06 (RPa 1.06, 95% CI: 1.03-1.10). On the other hand, being unmarried, living in a rural area and not using a contraceptive method were not significantly associated with interference in performing breast screening, with a p-value >0.05.
It was also found for the age variable in the analyzed data that in women aged 25-69 years, the proportion of women under 40 years of age not undergoing breast cancer screening is reduced by 41% with respect to the group of women who are older than 40 years.
Table 3. Analysis of multiple variables on the factors associated with screening interference for breast cancer in women aged 25-69 years according to ENDES 2019-2020.
| Screening for breast cancer | ||||||
|---|---|---|---|---|---|---|
| Sociodemographic factors | Adjusted PR (Screening for breast cancer) | Confidence interval Adjusted PR (95%) | P Value | |||
| Lower | Upper | |||||
| Sociodemographic Factors | ||||||
| Age | < 40 years | 0.58 | 0.57 | 0.59 | 0.00 | |
| ≥ 40 years | 1 | Reference | ||||
| Level of Education | Primary | 1.58 | 1.52 | 1.65 | 0.00 | * |
| Secondary | 1.42 | 1.37 | 1.47 | 0.00 | * | |
| Top | 1 | Reference | ||||
| Marital Status | Not married | 0.97 | 0.94 | 1.00 | 0.06 | |
| Married | 1 | Reference | ||||
| Region | Sierra | 1.21 | 1.17 | 1.25 | 0.00 | * |
| Jungle | 1.20 | 1.15 | 1.25 | 0.00 | * | |
| Coast | 1 | Reference | ||||
| Place of Residence | Rural | 0.97 | 0.94 | 1.01 | 0.09 | |
| Urban | 1 | Reference | ||||
| Health Insurance | No | 1.06 | 1.03 | 1.09 | 0.00 | * |
| Yes | 1 | Reference | ||||
| Sociocultural Factors | ||||||
| Beginning of Sexual Intercourse | < 18 years | 0.90 | 0.87 | 0.92 | 0.00 | |
| ≥ 18 years | 1 | Reference | ||||
| Contraceptive Method | Does not use | 1.01 | 0.98 | 1.04 | 0.50 | * |
| Uses | 1 | Reference | ||||
| Level of Knowledge | Does not know | 1.04 | 1.01 | 1.07 | 0.01 | * |
| Knows | 1 | Reference | ||||
| Economic Factors | ||||||
| Poverty | Yes | 1.06 | 1.03 | 1.10 | 0.00 | * |
| No | 1 | Reference | ||||
DISCUSSION
In this research study it is shown that the prevalence of women aged 25 to 69 years interviewed in the ENDES 2019 and 2020 who are not screened for gynecological cancers is 19.3% in cervical cancer and 54.9% in breast cancer.
Regarding the analysis of the factors associated with the interference of screening for cervical cancer, we find that the sociodemographic factors that are significantly associated are: age, level of education, marital status, religion, place of residence and health insurance. In the sociocultural factors, an association was found with: the age of beginning of sexual relations, the contraceptive method and the level of knowledge. Being also significant at the level of wealth in economic factors.
On the other hand, the following sociocultural factors that are significantly associated with the interference of screening for breast cancer: the level of education, the region and the place of residence. Among the sociocultural factors, it was found associated with the variables: contraceptive method and level of knowledge. Wealth level also showed a significant association.
In the last "Health Directive for the prevention of cervical cancer through early detection and treatment of pre-malignant lesions including carcinoma in situ" of 2019, it standardized that screening for cervical cancer (PAP, VIA and Molecular Test for HPV) It should be performed free of charge on all women aged 25-64 years nationwide. Of all these methods, the one that is most widely available for use by health personnel is the Pap smear. Despite the above, there is 19.3% of Peruvian women who do not undergo any screening, which makes us think about the following question: what factors are interfering with taking Pap smears in this percentage of women? After carrying out a detailed analysis, we found that all the study variables constituted a significant relationship in the interference of taking pap smears, becoming risk factors. Comparing with previously carried out studies, we found similar results.(3)(4)
Factors with statistically significant results such as: being under 40 years of age, low level of knowledge, living in a rural area and only having a primary education level and belonging to the non-poor classification; they have also been described in previous studies carried out in Peru. Olaza Maguiña (2017) reports that 50% of the population that did not accept the PAP test have a primary education level and 70.4% are under 38 years of age.(3) In a study carried out in Mexico, it was identified that 43.5% of women who did not undergo PAP only had primary education as their level of education.(5)
Guido Bendezu Quispe (2020) found that there is a 27% higher prevalence of performing a PAP in women who had answered the question Have you heard about cervical cancer? of ENDES 2015-2017 compared to those who did not respond, showing that the level of knowledge was a determining factor for taking PAP.(4) These results are shared by studies carried out in South America, where the factors associated with lack of knowledge, education, marital status, beginning of sexual relations before the age of 18 and not having health insurance are reported, increase the incidence in their population.(5)(6)(7)
Then the need for an intervention in primary prevention based on disseminating tools for the prevention and timely detection of cervical cancer would be evident. According to the analyzed data, in women 25-69 years old, the proportion of not taking a PAP in those who reside in the jungle and sierra regions is 1.56, 1.33 times respectively with respect to those who reside in the coastal region. , the information would be corroborated by various international studies where it is also evident that women who live in areas not belonging to the capital would present a lower percentage of taking PAP.(7)
Other variables described above were found, such as: use of contraceptive methods, where not using any method has a raw PR of 1.23, which would indicate that women who do not use a contraceptive method have a 23% higher probability of not having a PAP with respect to women who do use it, as reported in the study by Mamani Sánchez with the ENDES 2018 database.(8) This could be explained because women who do not use any method They do not have access to the information provided by health personnel in family planning consultations.
In recent years it has been shown that screening for breast cancer in Peru is lower than in other countries. In the study carried out, it was found that the incidence of women who did not perform any preventive screening for breast cancer was 53.6% and 56.5%. % in the last two years.
Regarding the factors associated with the interference of screening for breast cancer, the following variables were found to be statistically significant: having studied only up to primary or secondary school, belonging to the jungle or mountains, not having health insurance, not using some contraceptive method, not having some level of knowledge about gynecological screenings and belonging to the non-poor classification. The results found can be justified because in developing countries there is still a wide gap in access to cancer services, as reported in international studies. In studies carried out in Spain, it was shown that a low human development index and belonging to a low economic level have a direct association with screening.(9)(10)
In the analyzed data, we found the age variable as a protective factor, since in women aged 25-69 years, the proportion of women under 40 years of age not undergoing screening for breast cancer is reduced by 41% with respect to the group of women who are older than 40 years, in other countries studies show that having an advanced age has a greater coverage in carrying out screening for breast cancer.(10) What is described above is relevant because the average age of diagnosis for breast cancer is 62.6 years and it has been shown that screening before the age of 50 has better results in preventing this disease.
In the present study, it was found that age, marital status, place of residence and the beginning of sexual intercourse did not show an association with interference for breast cancer screening. One likely explanation is that very few women in our sample answered these questions.
Likewise, within the limitations of this study, it must be taken into account that the data was taken from the Demographic and Family Health Survey (ENDES) of the years 2019 and 2020, where no more variables can be added than those described by the survey. . The type of cross-sectional study, which allows determining association but not causality between the variables of interest.
The Demographic and Family Health Survey is a population-based survey that has quality control procedures and is designed to study health issues under the format of demographic and health surveys, constituting the main strength of the study. Currently, it is the only official source of population information that collects data on cancer prevention measures for Peruvian women.
CONCLUSIONS
The factors significantly associated with the interference of screening for gynecological cancers in women aged 25-69 in Peru, interviewed in the ENDES 2019-2020, for taking PAP are: age, level of education, marital status, region, Place of residence, health insurance, start of sexual relations, contraceptive method, level of knowledge and economic level. In Breast Cancer Screening, the associated factors are: level of education, region, health insurance, level of knowledge and economic level. Due to the fact that statistically significant factors were found with the interference of screening for gynecological cancers, it is recommended that future studies delve into the variables raised, in order to locate the population that is vulnerable to not undergoing screening for gynecological cancers.
Authorship contributions: CSL, WRA, RER and JDLCV, have participated in the conception of the article, the collection and analysis of data, its writing and approval of the final version.
Funding sources: Self-financed.
Conflicts of interest: The authors report no conflict of interest.
Received: March 03, 2022
Approved: July 07, 2022
Correspondence: Carmen Miluska Silva Lopez.
Address: Monte Abeto 304, Santiago de Surco.
E-mail: Carmen.silva@urp.edu.pe
Article published by the Journal of the faculty of Human Medicine of the Ricardo Palma University. It is an open access article, distributed under the terms of the Creatvie Commons license: Creative Commons Attribution 4.0 International, CC BY 4.0(https://creativecommons.org/licenses/by/1.0/), that allows non-commercial use, distribution and reproduction in any medium, provided that the original work is duly cited. For commercial use, please contact revista.medicina@urp.edu.pe.
REFERENCES
1. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71(3):209–49. doi:10.3322/caac.21660
2. Revilla T. L. Situación del Cáncer en Perú, 2021 [Internet]. Centro Nacional de Epidemiología, Prevención y Control de Enfermedades; 2021. Available at: http://www.dge.gob.pe/portal/docs/tools/teleconferencia/2021/SE252021/03.pdf
3. World Health Organization: Regional Office for Europe. World Cancer Report: Cancer Research for Cancer Development. Place of publication not identified: IARC; 2020.
4. Bravo Polanco E, Águila Rodríguez N, Guerra Villarpanda D, Blanco Vázquez Y, Rodríguez González O. Cáncer cérvico uterino: prevención y tratamiento. Medisur. 2020;18(4):9.
5. Encuesta demográfica y de salud familiar - ENDES 2019 [Internet]. Instituto Nacional de Estadística e Informática; 2019. Available at: http://iinei.inei.gob.pe/microdatos/Consulta_por_Encuesta.asp
6. Encuesta demográfica y de salud familiar - ENDES 2020 [Internet]. Instituto Nacional de Estadística e Informática; 2020. Available at: http://iinei.inei.gob.pe/microdatos/Consulta_por_Encuesta.asp
7. Resolución Ministerial N° 576-2019/MINSA [Internet]. [cited April 24, 2022]. Available at: https://www.gob.pe/institucion/minsa/normas-legales/282080-576-2019-minsa
8. Olaza Maguiña AF. Factores asociados a la no aceptación del examen de papanicolaou en mujeres en edad fértil, puesto de Salud Marián, 2017. Huarás, Perú: Universidad Nacional “Santiago Antúnez de Mayolo”; 2018.
9. Bendezú Quispe G, Soriano Moreno A, Urrunaga Pastor D, Venegas Rodríguez GG, Benites Zapata V. Asociación entre conocimientos acerca del cáncer de cuello uterino y realizarse una prueba de papanicolaou en mujeres peruanas. Rev Peru Med Exp Salud Publica. 2020;37(1):17–24. doi:https://doi. org/10.17843/rpmesp.2020.371.4730
10. Zapata FV, Cruz AM de la, Magaña-Olán L, Hernández JMG, Madrigal JDC. Factores Socioculturales Que Interfieren En La Realización Del Papanicolaou En Mujeres Indígenas Mexicanas. Eur Sci J ESJ. 2018;14(6):69–69. doi:10.19044/esj.2018.v14n6p69
11. Lee F-H, Wang H-H, Yang Y-M, Huang J-J, Tsai H-M. Influencing Factors of Intention to Receive Pap Tests in Vietnamese Women who Immigrated to Taiwan for Marriage. Asian Nurs Res. 2016;10(3):189–94. doi:10.1016/j.anr.2016.05.004
12. Artola Carballo FJ. actores y causas que influyen en la no realización del Papanicolaou en mujeres con vida sexual activa que asisten a las unidades de salud del departamento de Matagalpa, año 2015. Matagalpa: Universidad Nacional Autónoma de Nicaragua; 2015.
13. Alegría-Delgado D, Huamani-Navarro M. Factores asociados a la toma de mamografía en mujeres peruanas: análisis de la Encuesta Demográfica de Salud Familiar, 2015. An Fac Med. 2019;80(3):327–31. doi:10.15381/anales.803.16204
14. Lamiaa L, Ameijide A, Saladié F, Espinás JA, Galceran J. Participación de la población inmigrante en el cribado de cáncer de mama de Tarragona, España. Gac Sanit [Internet]. 2020 [cited October 5, 2021];5(33). doi:https://doi.org/10.1016/j.gaceta.2018.05.010
15. Puigpinós-Riera R, Castillo Gómez A, Romero Morales A, Aller M, Castells X, Sala M. Determinantes sociales y clínicos del uso de servicios sanitarios en mujeres con cáncer de mama (Cohorte DAMA) Determinantes sociales y clínicos del uso de servicios sanitarios en mujeres con cáncer de mama (Cohorte DAMA). 5. 2019;33:434–41. doi:https://doi.org/10.1016/j.gaceta.2018.04.014
