ARTICULO ORIGINAL
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2022 - Universidad Ricardo Palma10.25176/RFMH.v22i4.5172
LIMITED PERIAURICULAR FACELIFT HOW TO DEAL WITH SHORT SCAR: A TECHNICAL CONTRIBUTION
LIFTING FACIAL PERIAURICULAR LIMITADO: CÓMO TRATAR UNA CICATRIZ CORTA: UNA CONTRIBUCIÓN TÉCNICA
Patricio Centurion-Rivas1,a, Cynthia Montenegro Mirez2,b, Gerardo Ramos Masson4,c, Gonzalo Caballero calixto3,a
1Instituto de Investigaciones en Ciencias Biomédicas. Universidad Ricardo Palma. Lima, Perú
2Servicio de Cirugía Plástica, Estética y Reconstructiva, Profesor Ivo Pitanguy. Brasil.
3GC Cirugía Plástica y Estética
4Universidad Privada de ciencias aplicadas, UPC. Lima, Perú
aPlastic Surgeon
bResident of Plastic surgery
cMedical.
ABSTRACT
Facelift, currently, is one of the most demanded aesthetic procedures and considered as the Ultimate Facial Rejuvenation Surgery. The purpose of this present technique is to offer an alternative surgical procedure of reduced scars, lim-ited to the peri-auricular area, easily reproducible, without the need of extended incisions far beyond the retro-auricular sulcus neither the need of flaps for the temporal region. Our technique is based on a block reposition of the pre auricular area, cervical flaps movilization and rotation of a retro auricular flap, avoiding flaps and incisions in the temporal and occipital region; there-fore, minimizing visible scars (occipital pre-pilose scar), wide-tissue undermining, and in addition reducing the risk of damaging nerve structures with less recovery time for our patients, achieving natural and long lasting results.
RESUMEN
El lifting facial, en la actualidad, es uno de los procedimientos estéticos más demandados y considerado como la Cirugía de Rejuvenecimiento Facial por excelencia. El propósito de la presente técnica es ofrecer un procedimiento quirúrgico alternativo de cicatrices reducidas, limitadas a la zona peri-auricular, fácilmente reproducible, sin incisiones extendidas mucho más allá del surco retro-auricular ni necesidad de colgajos para la región temporal. Nuestra técnica se basa en una reposición en bloque de la zona preauricular, movilización de colgajos cervicales y rotación de un colgajo retroauricular, evitando colgajos e incisiones en la región temporal y occipital; por lo tanto, minimizando las cicatrices visibles (cicatriz prepilosa occipital), socavación de tejidos anchos, y además reduciendo el riesgo de dañar las estructuras nerviosas con menor tiempo de recuperación para nuestros pacientes, logrando resultados naturales y duraderos.
INTRODUCTION
Currently, Facelift constitutes one of the most demanded cosmetic surgical procedures, ranking seventh in popularity among all procedures according to the statistics published by ASAPS 2019. This procedure is considered the gold standard for Surgical Facial Rejuvenation. A point in common between the differ-ent surgical techniques described in text books is how the superficial muscular aponeurotic system (SMAS) is treated, which vary from plication, excision, splitting and division into one or multiple vectors of SMAS, among other variants (1) (2).
As described by Prof. F. Nahai, patients, who are looking for facial rejuvenation procedures, desire those who offer reduced or invisible scars; short recovery periods of time; and long-lasting natural results. Therefore, our surgical procedures must imply less dissection of tissues and fewer raised flaps whenever we can apply this principle in our patients. This also requires the use of complementary procedures such as facial fat grafting to replace facial volume lost (3) (4).
In 2001 Baker, and later Tonnard in 2002, drew worldwide attention by introducing new approaches in rhytidectomy with reduced incisions through a technique that offered a short scar facelift; nevertheless, these procedures left a marked and visible incision in the temporal area by creating a temporal flap (5) (6). From our perspective, the MACS technique creates more a rotational flap in the temporal area rather than a real temporal flap lift risking injury to the frontal branch of the facial nerve (7).
Technically, a surgical scar is reduced when the incision remains in the retro-auricular groove (8). We agree with this concept but with our technique, we avoid making a temporal incision and dissecting the temporal flap, which consequently minimizes visible scars and tissue dissection. Our incision and rotation of the retro-auricular flap achieves the excess of cervical skin without visible occipital hair-line scarring.
Surgical technique:
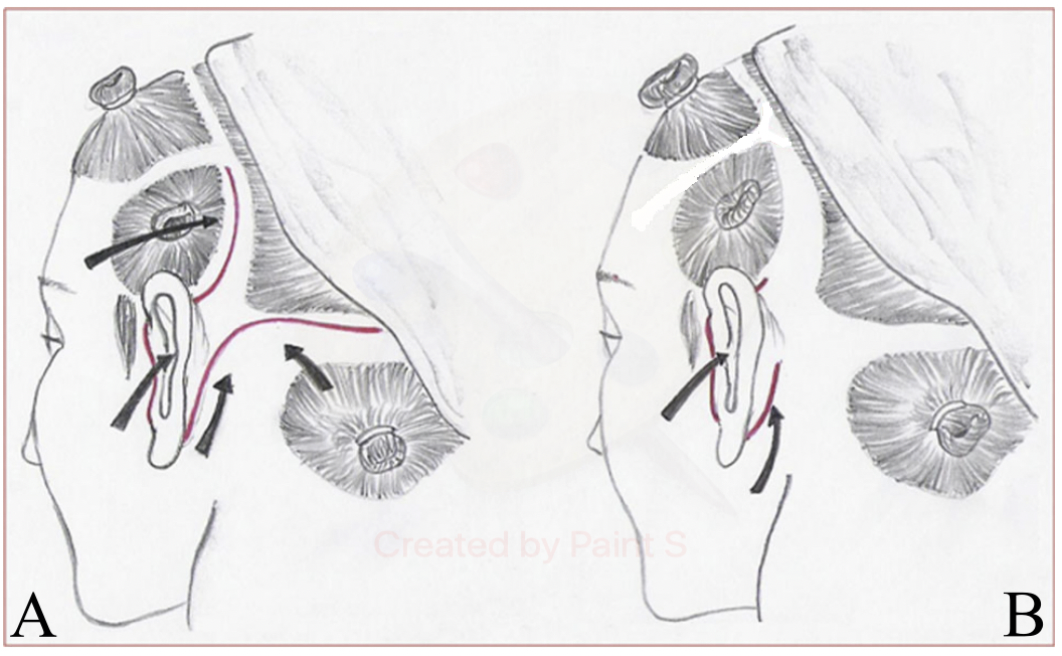
Our technique is based on the Short Scar Facelift without temporal flap procedure, in which limited pre-auricular and retro-auricular incisions are used for treating the whole face area and cervical flap in one block avoiding a temporal and occipital flaps (2). Figure 1.
This procedure is performed in an operating room under sedation guided by an anesthesiologist and local anesthesia. A 2% lidocaine solution (40cc) is used along with 1ml of Epinephrine 1/1000 and a cold sa-line solution (0.9% 160cc) with 4cc of bicarbonate at 8.4%, which is injected with 10 cc syringes and a large 2" needle of an 18G EV-catheter. The infiltration volume is 50 to 60cc by each side of the face and 30 a 40cc in the cervical area.
The pre-auricular incision is made from the root of the helix and progresses in a retro-tragal fashion until it reaches the vertex of the earlobe. Subsequently, following the retro-auricular area, the incision contin-ues along convex surface of the auricular conchae where the upper limit is the mid-point of the auricular conchae.
The upper limit of dissection of the pre-auricular flap is a parallel line of the zygomatic arch, 2cm above the same and lateral to the orbital rim. The retro-auricular dissection begins at the mid-point of the auric-ular conchae and continues 4 cm below the earlobe in a cervical direction before it moves upward 3 cm from the earlobe toward the mandibular edge. The plane of disection along the pre-auricular flap is sub-dermal and the medial limit is set between 6 to 7 cm from the point of the incision (Figure 2).
Once the pre and retro-auricular flaps are dissected, hemostasis is conducted and we begin to make the SMAS-plication or smastectomy, using inverted horizontal mattress sutures with a 4/0 Nylon suture; the approach (number of plication sutures) of the SMAS and of the platysma depends on personal prefer-ences.
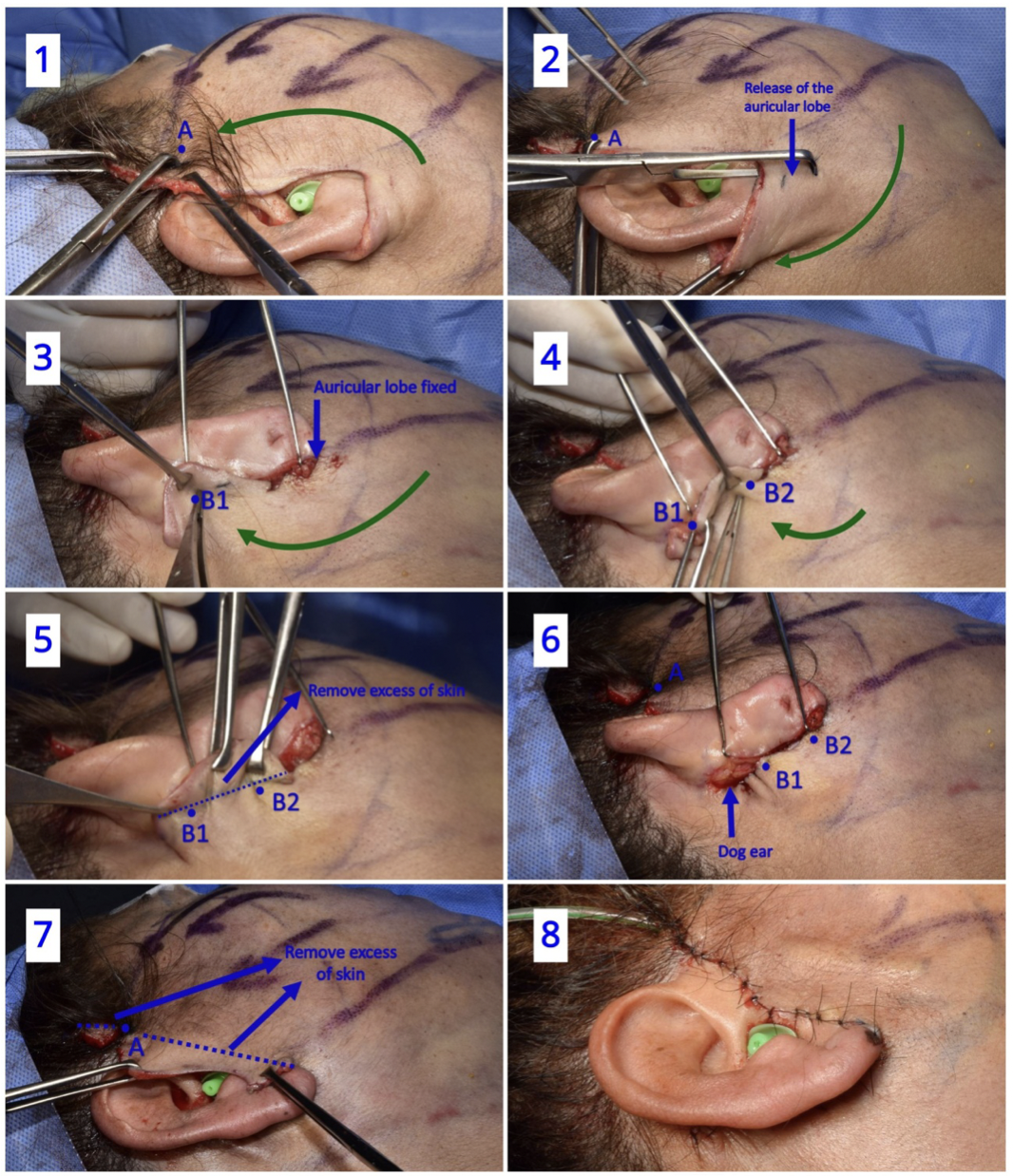
The traction of the pre and retro-auricular flaps follows the direction described on the Round Block tech-nique developed by Prof. Ivo Pitanguy (9). While the pre-auricular flap is held by two Allies forceps and applying counter-traction; with a Pitanguy flap forceps we mark at the root of the helix the excess of skin to be removed and with a 4/0 Nylon knot we delimited our A point landmark (Figure 3.1).
The earlobe is then released through oblique traction of the flap and with one Allis forceps we mark the new position of the earlobe (without excess of traction); then, the flap is fixed with a 4/0 Vicryl sub-dermic suture and with a 5/0 Nylon for the skin (Figure 3.2 and 3.3).
The cervical flap is pulled and the point that better match with the most cephalic point of our incision is marked and subsequently sutured sub-dermally with 4/0 Vicryl at the most cephalic point of the auricu-lar conchae, which is marked as point landmark B1. Point B2 is the mid-distance between the fixed lobe and point B1. The flap is fixed with sub-dermic 4/0 vicryl suture which is placed in the dermis that is going to be repositioned (Figure 3.4).
Finally, excess of skin in the pre and retro auricular areas is eliminated through light-moderate traction and flap adjustment (Figure 3.5). The ears dog of both sides, above point A and outside of point B1, are cut and residual tissue is compensated (Figure 3.6 and Figure 3.7.
At the end of the procedure, 5/0 nylon sutures are used for the pre-auricular skin whereas for the retro-auricular skin we prefer nylon 4/0 sutures. A drainage tube with negative pressure is left in place for 1 or 2 days at the most (Figure 3.8).
We usually performed a complementary procedure with facial fat grafting using micro cannulas in the non-dissected areas to restore the volume lost in those tissues. Scars are pretty much unseen and well accepted by our patients and usually at 3 months settled down (Figure 4).
Discussion
The Limited Periauricular Facelift technique allows for a reproducible method of treating lower 2/3 of the face and cervical flaccidity included including, with less scars and less traumatic manipulation of face flaps. This translates significally in less edema, ecchymosis and short recovery time as we can see in the Figure 5 and Figure 6 in which we present a post 24hrs result.

The main indication perhaps for this technique is the presence of a low or medium grade of flaccidity as we can see in patients between 45 - 60 years old, or in secondary facelift. This type of patients often seek for optimal and long-standing results in the middle-third and lower-third of the face but have some hesi-tates about conventional facelift procedures.
Despite of benefits and positive effects about treating the face with minimal incisions and less traumatic dissection, this technique have some inconveniences. In some patients with flaccidity of the upper-third of the face we must treat this area for optimal complementary results; we found many techniques suita-ble as a better option over the temporal flap in the standard facelift, which is a rotation flap rather than a desire vertical vector. We use for this a minimal approach of lateral brow lift described in by senior au-thor in 2010 (10).
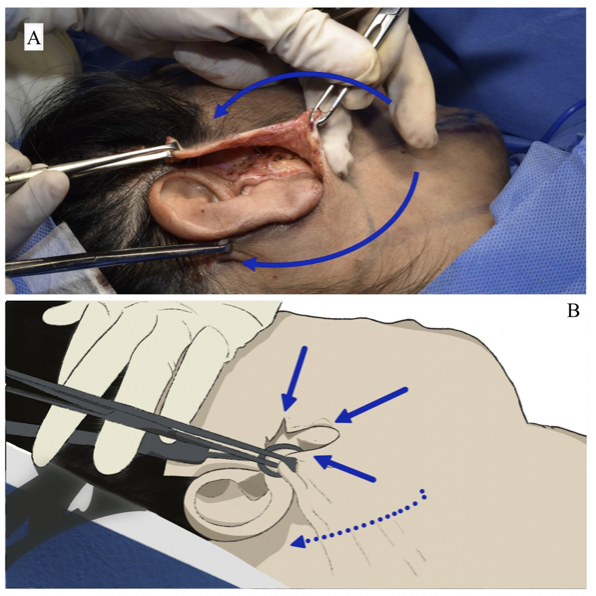
The vector used in the retro-auricular scar in our proposed technique offer a better coaptation between skin edges, different to the Short Scar Rhytidectomy Technique by Vincent, et al. In Figure 7 we can see where the retro-auricular flap cut remains in the posterior scar, this is where, sometimes, surgeons would find difficult to compensate and might translate in some patients with an initially folded scar. This re-solves over a period of 3-6 months without need of revisions though.
Conclusions
The objective of this technique is to offer a simplified surgical procedure that implies less visible scarring that can be easily performed without making incisions beyond 1-2 cm above the root of the helix, major incisions in the retro-auricular area, and eliminating the need of an occipital hair-line flap.
Authorship contributions: The authors participated in the genesis of the idea, project design, data collection and interpretation, and preparation of the manuscript of this research work.
Funding sources: Self-financed.
Conflicts of interest: The authors declare to have no conflict of interest in the publication of this article.
Received: May 23, 2021
Approved: September 12, 2022
Correspondence: Gonzalo Caballero Calixto.
Address: Jr. Costa Rica 140 Dpto 301 Jesús María. Lima Perú.
Telephone number: 940244113
E-mail: g.caballero.c2@gmail.com
Article published by the Journal of the faculty of Human Medicine of the Ricardo Palma University. It is an open access article, distributed under the terms of the Creatvie Commons license: Creative Commons Attribution 4.0 International, CC BY 4.0(https://creativecommons.org/licenses/by/1.0/), that allows non-commercial use, distribution and reproduction in any medium, provided that the original work is duly cited. For commercial use, please contact revista.medicina@urp.edu.pe.
REFERENCES



