CASO CLÍNICO
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2021 - Universidad Ricardo PalmaAquí iría el DOI
XANTHOGRANULOMATOUS APPENDICITIS A DIAGNOSTIC CHALLENGE: CLINICAL CASE
APENDICITIS XANTOGRANULOMATOSA UN DESAFÍO DIAGNÓSTICO: CASO CLÍNICO
Alan Alexis Hernández-Morán1,a, Gisela Alonso-Torres2,b, Claudia Teresita Gutiérrez-Quiroz1,c,Álvaro José Montiel-Jarquín1,d,Nancy Rosalía Bertado-Ramírez1,e,Arturo García-Galicia1,f,Sandra Maldonado-Castañeda3,g
1Unidad Médica de Alta Especialidad Hospital de Especialidades de Puebla Centro Médico Nacional General de División Manuel Ávila Camacho del Instituto Mexicano del Seguro Social, Puebla, Mexico.
2Unidad Médica de Alta Especialidad Hospital de Especialidades de Puebla Centro Médico Nacional General de División Manuel Ávila Camacho del Instituto Mexicano del Seguro Social. Facultad de Medicina, Benemérita Universidad Autónoma de Puebla, Puebla, Mexico.
3Postgrado del área de la Salud, Universidad Popular Autónoma del Estado de Puebla, Puebla, Mexico.
aGeneral Practitioner. Resident of Pathological Anatomy.
bMedical Social Service Intern.
cSpecialist in Anatomic Pathology.
dMedical specialist in General Surgery. Master in Medical Sciences and Research.
e Physician specializing in Neurology.
fMedical specialist in Pediatrics. Master in Medical Sciences and Research.
gPhysician specializing in General Surgery.
ABSTRACT
Introduction:Xanthogranulomatous inflammation is a chronic inflammatory process, rarely located in the appendix. A case of xanthogranulomatous appendicitis is presented. Clinical case: A 77-year-old male presents with intermittent pain in the right hemiabdomen and hyperthermia of one month's evolution. Physical examination showed a tumor in the iliac fossa and right abdomen. He underwent surgery for a probable incarcerated right inguinal hernia, acute perforated appendicitis was found, with inflammation and adhesions, purulent fluid in the right hemiabdomen, and abdominal wall dissection. The histopathological result was xanthogranulomatous appendicitis. The evolution of the patient was favorable. Conclusion: Xanthogranulomatous appendicitis simulates a typical picture of acute appendicitis. Histopathologically, pathologies such as Crohn's disease, malacoplakia, and tuberculous appendicitis were ruled out.
Keywords: Xanthogranulomatous appendicitis; Appendicitis; Foam cells; Michaelis-Gutmann bodies (Sourse: MeSH NLM).
RESUMEN
Introducción: La inflamación xantogranulomatosa es un proceso inflamatorio crónico, rara vez se localiza en apéndice. Se presenta un caso de apendicitis xantogranulomatosa. Caso clínico: Masculino de 77 años, presenta con dolor intermitente en hemiabdomen derecho e hipertermia de un mes de evolución. La exploración física mostró tumoración en fosa iliaca y abdomen derecho. Se sometió a cirugía por probable hernia inguinal derecha incarcerada, se encontró apendicitis aguda perforada, con inflamación y adherencias, líquido purulento en hemiabdomen derecho y disección en pared abdominal. El resultado histopatológico fue apendicitis xantogranulomatosa. La evolución del paciente fue favorable. Conclusión: La apendicitis xantogranulomatosa simula un cuadro típico de apendicitis aguda. Histopatológicamente se descartan patologías como enfermedad de Crohn, malacoplaquia y apendicitis tuberculosa.
Palabras Clave: Apendicitis xantogranulomatosa, Apendicitis, Células espumosas, Cuerpos de Michaelis-Gutmann (fuente: DeCS BIREME).
INTRODUCTION
Acute appendicitis is one of the most common surgical problems in clinical practice. Pathologic evaluation is the gold standard for diagnosing acute appendicitis. Routine histopathologic evaluation is performed to confirm the diagnosis of acute appendicitis and may reveal other important pathologic details.(1)
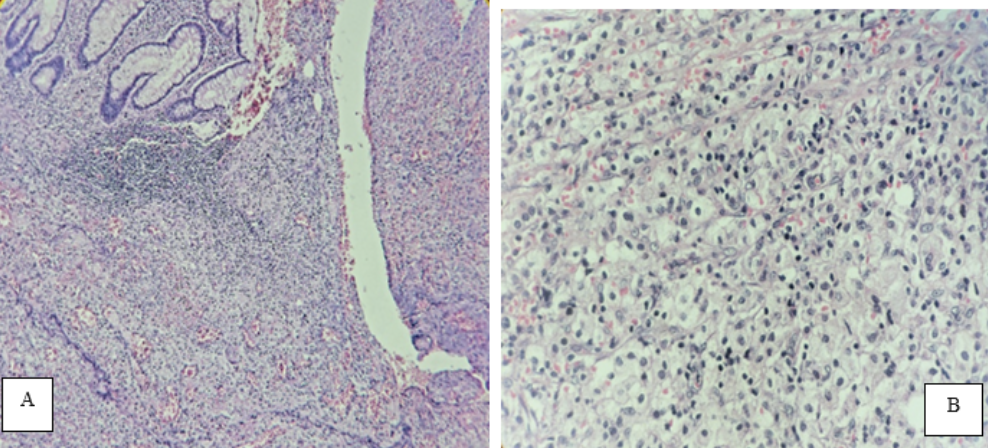
Xanthogranulomatous inflammation (XGI) is a chronic inflammatory process observed in other sites such as gall bladder, kidney, ovaries, prostate, epididymis, etc. Appendiceal involvement is quite rare and has been observed more frequently in interval appendicitis. It is characterized by a cluster of xanthoma-like cells, with a prominent histiocytic component. (2)Microscopically there is ulceration along with numerous inflammatory cells, mostly neutrophils located in the muscularis propria, necrosis, and congestion.
DESCRIPTION OF THE CLINICAL CASE
We present a 77-year-old male patient with a personal pathological history of type 2 diabetes, without specifying the time of evolution or treatment; he referred to a clinical picture of four weeks of evolution with mild abdominal pain predominantly right, unquantified hyperthermia of two days of evolution with antibiotic and symptomatic management. There was a frank improvement for three weeks; but eight days before surgery the symptoms increased, she had an increase in volume at the level of the right iliac fossa with increased local temperature. Physical examination showed a soft abdomen, depressible, painful at the site of the tumor, measuring 15x15cm, of solid consistency, with hyperemic and hyperthermic skin surface and no evidence of peritoneal alarm. The rest of the physical examination was normal with the following vital signs: BP 110/75, HR 78 bpm, RR 19 rpm, axillary temperature 37°C, and O2 saturation 93%. Preoperative laboratory studies showed leukocytosis at the expense of neutrophils, the rest of the blood biometry and coagulation times were normal (Table 1). Ultrasonography (USG) of the abdominal and inguinal wall showed the presence of right inguinal hernia Figure 1.
Table 1. Preoperative clinical studies.
| BLOOD BIOMETRY | |
|---|---|
| RED FORMULA | |
| Hemoglobin(Hb) | 35.1% |
| Platelets | 400x103/uL |
| WHITE FORMULA | |
| Total leukocytes | 15.0x103/uL |
| Total neutrophils | 12,900/uL |
| PARTIAL BLOOD CHEMISTRY | |
| Serum glucose | 185 mg/dl |
| COAGULATION PROFILE | |
| Prothrombin time | 14.5 sec. |
| Control plasma(TP) | 12.2 |
| INR | 1.21 |
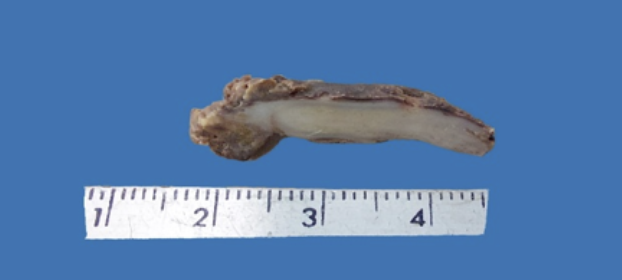
The patient underwent exploratory laparotomy and 500ml of fetid purulent material was found in the abdominal wall at the tumor site, in the abdominal cavity intestinal loops adhered to the cecum where plastron and inflamed cecal appendix were found in the distal third with perforation in the middle third. The blood biometry at 72 hours reported a decrease in leukocytes, the result of the culture of the abdominal wall exudate was positive for Streptococcus viridans sensitive to imipinem and clindamycin (Table 2), the histopathological diagnosis was xanthogranulomatous appendicitis Figure 3. The evolution was stable, with improvement and in eight days he was discharged home without any apparent complication.
Tabla 2. Postoperative clinical studies.
| CULTURE OF ABDOMINAL WALL EXUDATE | |
|---|---|
| Bacteriological examination | Streptococcus viridans |
| ANTIBIOGRAM BY DISK DIFUSSION | |
| Imipinem | Sensible |
| Clindamycin | Sensible |
| BLOOD BIOMETRY | |
| RED FORMULA | |
| Hemoglobin(Hb) | 10.7 g/dL |
| Hematocrit | 32.8% |
| Platelets | 407x103/uL |
| WHITE FORMULA | |
| Total leukocytes | 13.5x103/uL |
| Total neutrophils | 89% |
| PARTIAL BLOOD CHEMISTRY | |
| Serum glucose | 152.0 mg/dl |
| Serum urea nitrogen | 15 mg/dl |
| Serum urea | 32.1 mg/dl |
| Serum creatinine | 0.7 mg/dl |
| SERUM ELECTROLYTES | |
| Serum sodium | 139.0 mmol/L |
| Serum potassium | 4.1 mmol/L |
| Serum chlorine | 110.0 mmol/L |
DISCUSSION
XGI is a chronic inflammatory process that leads to local destruction of the tissues of the affected organ or those located in its vicinity. This type of inflammation has been described in kidney, gallbladder, prostate, epididymis, ovary and rarely in the cecal appendix. Histologically it has macrophages in which lipids are deposited with lymphocytes that give it a "foamy" appearance, plasma cells, neutrophils and cells.
In this case, the histopathological study reported macroscopically perforated appendix in the middle third and tip, with fibrinous-purulent adhesions and thickened wall with subserous light yellow foci Figure 2.
Proposed theories of the etiopathogenesis of this entity include abnormal lipid transport, immunological disorders of leukocyte and macrophage chemotaxis, infection by Proteus and Escherichia species that are of low virulence or by obstruction at the lymphatic level. However, in a study by Cozzuto et al. found that the xanthogranulomatous process is mainly associated with inflammation, hemorrhage and necrosis. (3-5).
It has also been frequently observed in interval appendicitis, suggesting that late appendectomy often has a granulomatous inflammatory pattern with fibrosis, mural thickening and chronic transmural inflammation. (4,5).
Its clinical presentation usually presents with pain in the right lower quadrant of the abdomen, fever, nausea and vomiting; other authors associate prolonged inflammation of the appendix with the formation of an appendiceal mass. Pathologies affecting the appendix catalogued in the atypical spectrum can simulate and cause a typical picture of acute appendicitis. (3).
Sometimes it is not possible to differentiate XGI from an infiltrative cancer because it may present as a tumor-like lesion with an extension of fibrosis and inflammation into the surrounding tissues. 6. Other inflammatory processes that cause granulomatous lesions and contain foam cells should be distinguished from XGI are Crohn's disease which is distinguished by the presence of transmural granulomas, and malakoplakia which is characterized by an inflammatory and destructive xanthomatous proliferation with the presence of Michaelis-Gutmann bodies or calcospherites (intracytoplasmic inclusion in concentric layers). Small localized xanthoma deposits without parenchymal destruction or xanthomas with prominent foam cell features found in tuberculous appendicitis should also be considered in the differential diagnosis. (3,6,7)
Another entity to rule out due to the chronicity of symptoms and the presence of a mass in the abdominal region is Spiegel's hernia, in which the appendix is rarely contained. Imaging studies are useful for diagnosis (8); However, with exploratory laparotomy it could be ruled out when purulent liquid was obtained in the area where it was believed to be a hernia, a plastron was observed in the cecum and the cecal appendix was inflamed.
It is concluded from this case report that XGI does not have a specific clinical picture, the definitive diagnosis is obtained when the appendix is analyzed histologically and the treatment is surgical supplemented with broad-spectrum antibiotics.
Authorship contributions: All authors participated in the preparation of this case report.
Funding sources: The authors received no financial support or funding for this work.
Conflicts of interest: The authors declare that they have no conflicts of interest.
Received: August 27, 2022
Approved: September 18, 2022
Correspondence: Álvaro José Montiel-Jarquín.
Address: Calle 2 norte # 2004. Colonia Centro. CP 72000. Puebla, Mexico.
Telephone number: +52 (222) 2424520 extension 61315.
E-mail: dralmoja@hotmail.com
Article published by the Journal of the faculty of Human Medicine of the Ricardo Palma University. It is an open access article, distributed under the terms of the Creatvie Commons license: Creative Commons Attribution 4.0 International, CC BY 4.0(https://creativecommons.org/licenses/by/1.0/), that allows non-commercial use, distribution and reproduction in any medium, provided that the original work is duly cited. For commercial use, please contact revista.medicina@urp.edu.pe.
REFERENCES

