CLINICAL CASE
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2023 - Universidad Ricardo Palma10.25176/RFMH.v23i2.5656
ULTRARARE DISEASE FREQUENT IN PERU:
CASE REPORTS OF FATCO SYNDROME
ENFERMEDAD ULTRARARA FRECUENTE EN PERÚ: REPORTE DE CASOS DEL SÍNDROME FATCO
Wendy Gutierrez-Baca
 1,2,
D'Karlo Dongo-Cornejo
1,2,
D'Karlo Dongo-Cornejo
 1,
1,
Hugo H. Abarca Barriga
 1,3
1,3
1 Carrera Profesional de Medicina Humana, Universidad Científica del Sur. Lima, Perú.
2 CHANGE Research Working Group, Facultad de Ciencias de la Salud, Carrera de Medicina Humana, Universidad Científica del Sur. Lima, Perú.
3 Servicio de Genética & Errores Innatos del Metabolismo. Instituto Nacional de Salud del Niño-Breña. Lima, Perú.
ABSTRACT
The fibular aplasia, tibial campomelia, oligosyndactyly (FATCO) syndrome is characterized by the variable leg anomalies. The genetic etiology of this disease has not been determined to date; however, it has been suggested that the genetic inheritance is autosomal dominant. The frequency of presentation globally is infrequent and this is the main reason for the low number of patient reports.
There’s a report of the unusually high presentation of 14 Peruvian patients diagnosed at a single center with the clinical features of FATCO syndrome over a 13-year period. We compare and discuss the clinical and radiological data of our patients with those of the 14 cases described worldwide. In addition, the demographic characteristics, family history, sex, age, and concomitant anomalies are analyzed.
Keywords: Fibular aplasia, tibial campomelia, oligosyndactyly, FATCO syndrome. (Source: MeSH – NLM).
RESUMEN
El síndrome FATCO (fibular aplasia, tibial camptomelia, oligosyndactyly) está caracterizado por la presencia de anomalías en miembros inferiores. Es una enfermedad, de la cual no se ha precisado la etiología genética hasta la actualidad; sin embargo, se ha planteado que el tipo de herencia es dominante autosómica. La frecuencia de presentación a nivel global es muy rara y esta es la razón principal de los pocos pacientes publicados hasta la fecha.
Existe un reporte de la presentación inusual de catorce pacientes peruanos, diagnosticados en un solo centro, con las características clínicas del síndrome FATCO en un período de 13 años. A la fecha, se han publicado catorce pacientes a nivel mundial, con los cuales se comparó y discutió los datos clínicos y radiológicos. Además, se analizaron las características demográficas, antecedentes familiares, sexo, edad y anomalías concomitantes.
Palabras Clave: Aplasia de fíbula, campomelia de tibia, oligodactilia, síndrome FATCO. (Fuente: DeCS – BIREME).
INTRODUCCIÓN
FATCO syndrome (Fibular Aplasia, Tibial Camptomelia, Oligosyndactyly) is characterized by the presence of aplasia or hypoplasia of the fibula, campomelia of the tibia and oligosyndactyly (1). The clinical manifestations are highly variable, ranging from deficiencies in all four limbs, accompanied by cardiac malformations to anomalies in only the lower limb with the three basic minimal features (2,3,4). Regarding the campomelia sign in long bones, it can also present in different entities such as Roberts syndrome, skeletal dysplasias, fetal constriction, pseudarthrosis and limb pterygium (6).
FATCO syndrome (coded in Mendelian Inheritance in Man with #246570) is a genetic and congenital disease of unknown etiology. However, it has been suggested that it has an autosomal dominant inheritance, with an ultra-rare frequency of presentation, and that it has an autosomal dominant inheritance, with an ultra-rare frequency of presentation.s i.e. it has a prevalence of less than 1 in a million people (7,8). It was first described by Hecht and Scott in 1981, in two brothers with transverse limb deficiencies (9). It was Courtens et al. in 2005, who coined the term FATCO, compiling the two patients studied by Hecht and specifying that there are three more cases, which were previously described as other syndromes (1). To date, worldwide, there is only information on twenty-two patients (10-24), of which five cases have been previously reported in Peru; however, there is no clinical description (25).
We will describe the clinical characteristics of fourteen Peruvian patients diagnosed with FATCO syndrome, which we will compare with previously reported patients, and also, be able to provide more clinical information about this disease, which greatly impacts the quality of life of those affected. For this reason, having a greater and better clinical description would allow us to understand a better understanding the pathologya. Re skip that most of the cases reported worldwide are found in South America, almost all of them in Peru.
METHODS
Due to the absence of genetic diagnostic tests, established clinical criteria and because it is a rare pathology, it was decided to include all patients who presented at least two of the three minimum clinical and radiological phenotypic characteristics, which are the presence of aplasia/hypoplasia of the fibula, campomelia of the tibia and oligosyndactyly; allowing us to find a greater number of children evaluated. The patients registered were from 2008 to 2021 attended at the Genetics & Inborn Errors of Metabolism Service of the Instituto Nacional de Salud del Niño Breña, which is one of the few Peruvian national reference centers for pediatrics and especially for pediatric genetics.
For data collection, approval was obtained from two local ethics committees (Universidad Científica del Sur and Instituto Nacional de Salud del Niño-Breña), which maintained the privacy and confidentiality of the clinical histories. The information collected was prenatal, natal and family history, anthropometry at birth, origin of parents and grandparents, as well as the phenotype of each patient
RESULTS
There were 14 patients who met the clinical and radiological diagnostic criteria for FATCO syndrome . (Figure 1)
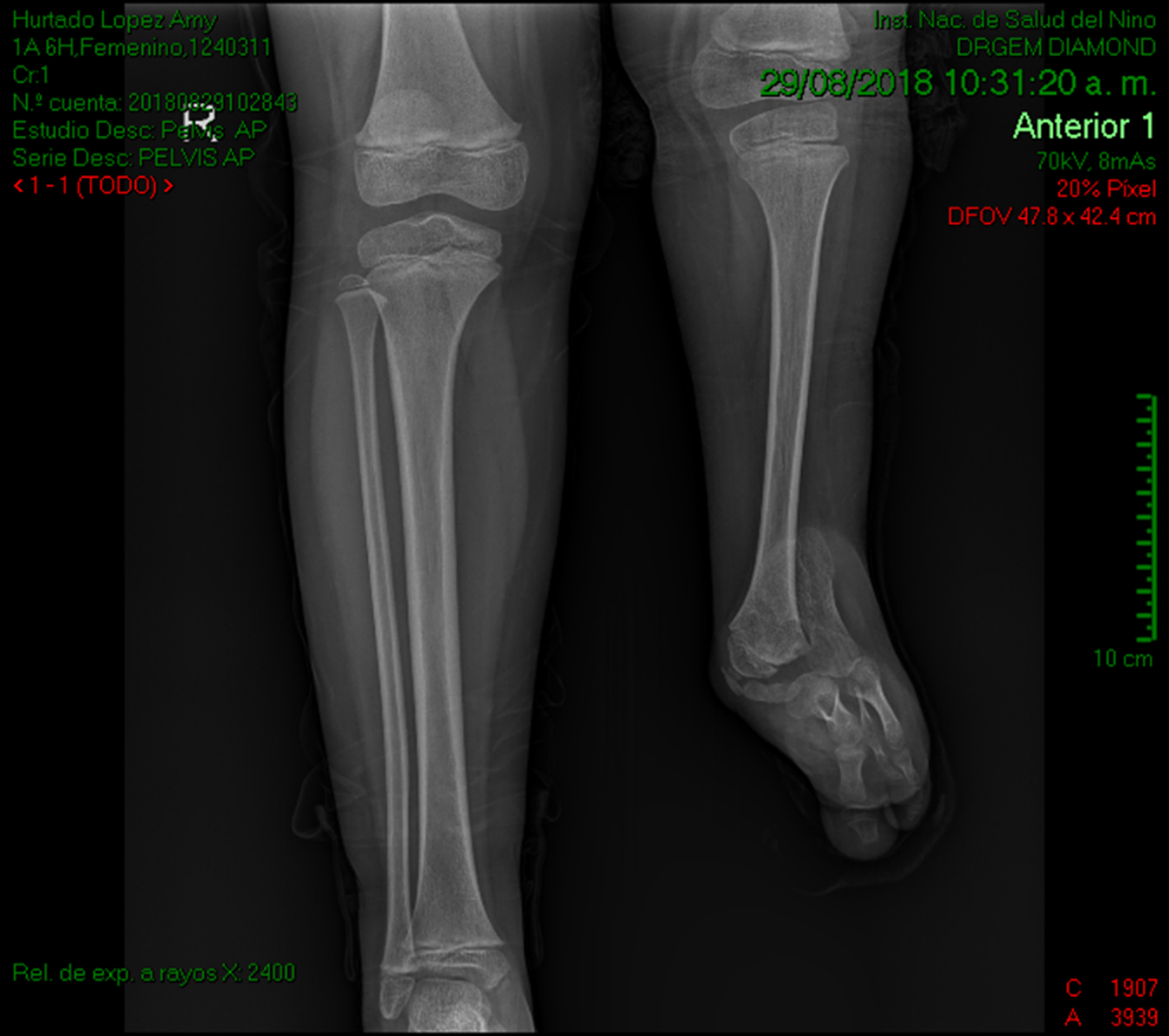
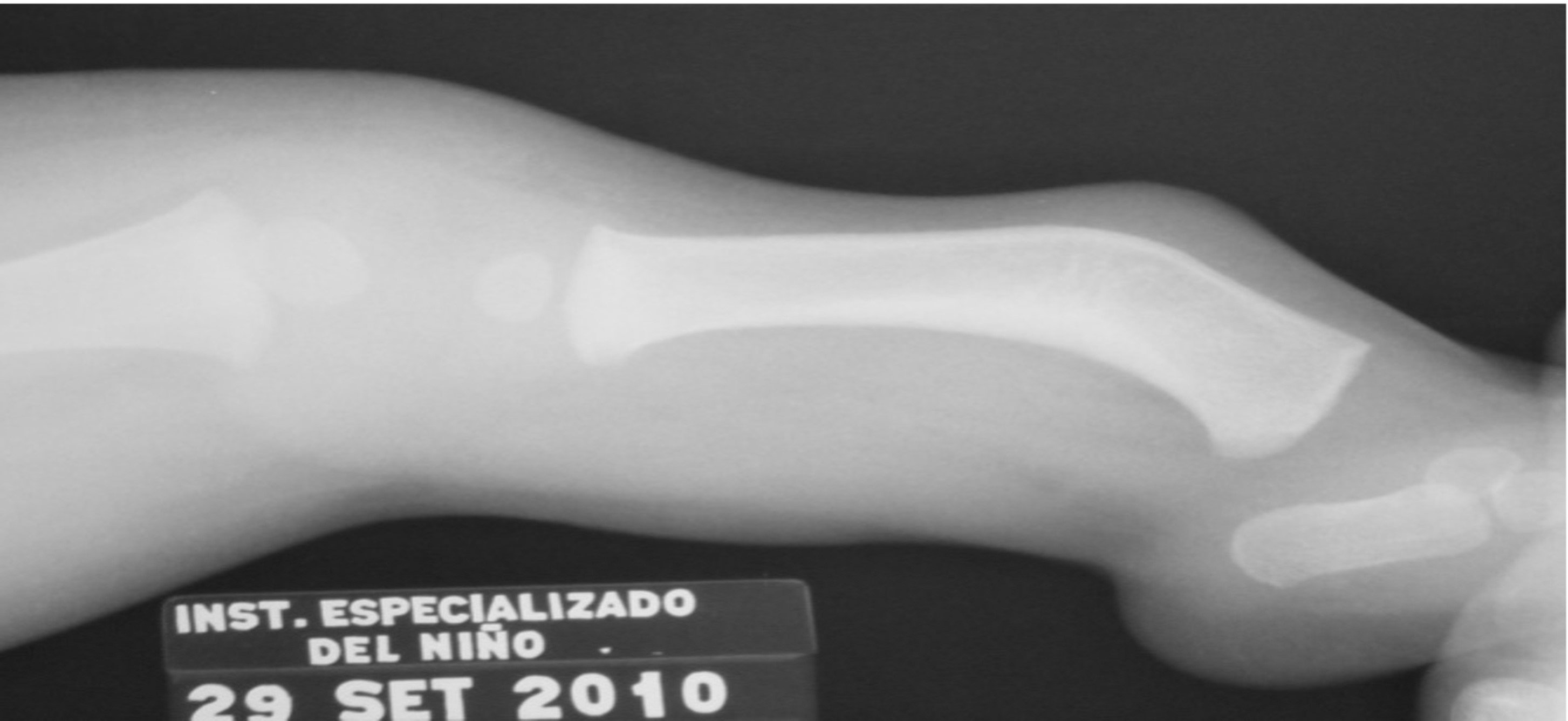
Figure 1. Clinical and radiological characteristics of the patients. (A) X-ray of the lower extremities showing tibial hypoplasia, fibular aplasia and oligosyndactyly in the left leg.
Regarding age, patients had a median age of 14 months (RIC=82.5), mothers with a mean of 29 years (σ =8.04), and in fathers with a mean of 30 years (σ =7.22). Sixty- four percent were male. No intercurrences were reported during pregnancy. The place of origin of the grandparents was very variable (Ayacucho, Cusco, Cajamarca, Puno, La Libertad, Lima, Ica, Cerro de Pasco and Huancavelica), with no specific region having a higher number of patients reported. family history of musculoskeletal anomalies or parental consanguinity was observed. The birth history included measures of central tendency and dispersion of weight, height and head circumference of 3262 g (σ = 391 g), 50 cm (σ =1.21 cm) and 34.4 cm (σ =1.77 cm), respectively. The reported Apgar was found to be in normal ranges (Table 1).
Table 1. Demographic characteristics of patients at the National Institute of Child Health with FATCO syndrome in Peru (2008-2021).
|
Clinical features |
Average results |
|---|---|
|
Patient Data |
|
|
Patient age (months) |
14 (RIC= 82.5) |
|
Sex |
9/ 14 Male |
|
Birth weight (g) |
3268,10 (σ=391,88) |
|
Height at birth (cm) |
50.69 (σ=1.21) |
|
Head circumference |
34,43 (σ=1.77) |
|
Apgar |
8/8 Normal |
|
Family history |
|
|
Mother's age (years) |
29,3(σ=7,66) |
|
Father's age (years) |
30,4(σ=6,89) |
|
Brothers |
6/ 14 Positives |
|
Abortions |
4/ 14 Positives |
|
Family history of limb malformations |
0 / 14 Positives |
|
Prenatal history |
S/P |
|
Consanguinity |
0/ 14 Positives |
S/P: not particular; ND: not described; NR: not performed; NE: not specified; Positive: presence of anomaly;
Negative: no presence of anomaly; IQR: interquartile range; SD: deviation; SD: deviation from standard deviation
The presence of campomelia and tibial hypoplasia was found with similar frequency in both lower limbs (See Figure 1 and Figure 2, Table 2).
|
Clinical features Upper extremity anomalies |
POSITIVES |
NEGATIVES |
NOT SPECIFIED |
% |
|---|---|---|---|---|
|
Complete syndactyly of left hand 1st- 2nd and 4th-5th |
1 |
12 |
1 |
7,14 |
|
3rd-5th cutaneous syndactyly |
0 |
13 |
1 |
0 |
|
Absence of fourth metacarpal of hand |
1 |
12 |
1 |
7,14 |
|
Hand anomaly |
3 |
10 |
1 |
21,42 |
|
Abnormalities in lower extremities |
|
|
|
|
|
Dimple in leg |
8 |
2 |
4 |
57,14 |
|
Absence of the 5th toe |
12 |
1 |
1 |
85,71 |
|
Absence of 4th-5th toe |
7 |
6 |
1 |
50 |
|
Absence of 3rd-5th toes |
3 |
10 |
1 |
21,42 |
|
Syndactyly of the 1st-2nd orthocylinder |
3 |
10 |
1 |
21,42 |
|
Absence of fibula |
13 |
0 |
1 |
92,85 |
|
Campomelia of tibia |
14 |
0 |
0 |
100 |
|
Tibial hypoplasia |
14 |
0 |
1 |
100 |
|
Other anomalies |
|
|
|
|
|
Nails |
0 |
11 |
3 |
0 |
|
Psychomotor development |
0 |
10 |
4 |
0 |
|
Screening for bone anomalies in other regions |
0 |
8 |
6 |
0 |
|
Congenital heart disease |
0 |
11 |
3 |
0 |
|
Brain MRI |
0 |
0 |
14 |
0 |
|
Fundus |
0 |
0 |
14 |
0 |
|
Renal ultrasonography |
0 |
5 |
9 |
0 |
|
Auditory evoked potentials |
0 |
0 |
14 |
0 |
|
Karyotype |
0 |
0 |
14 |
0 |
Y/N: not particular; ND: not described; NR: not performed; NS: not specified; Positive: presence of anomaly; Negative: no presence of anomaly
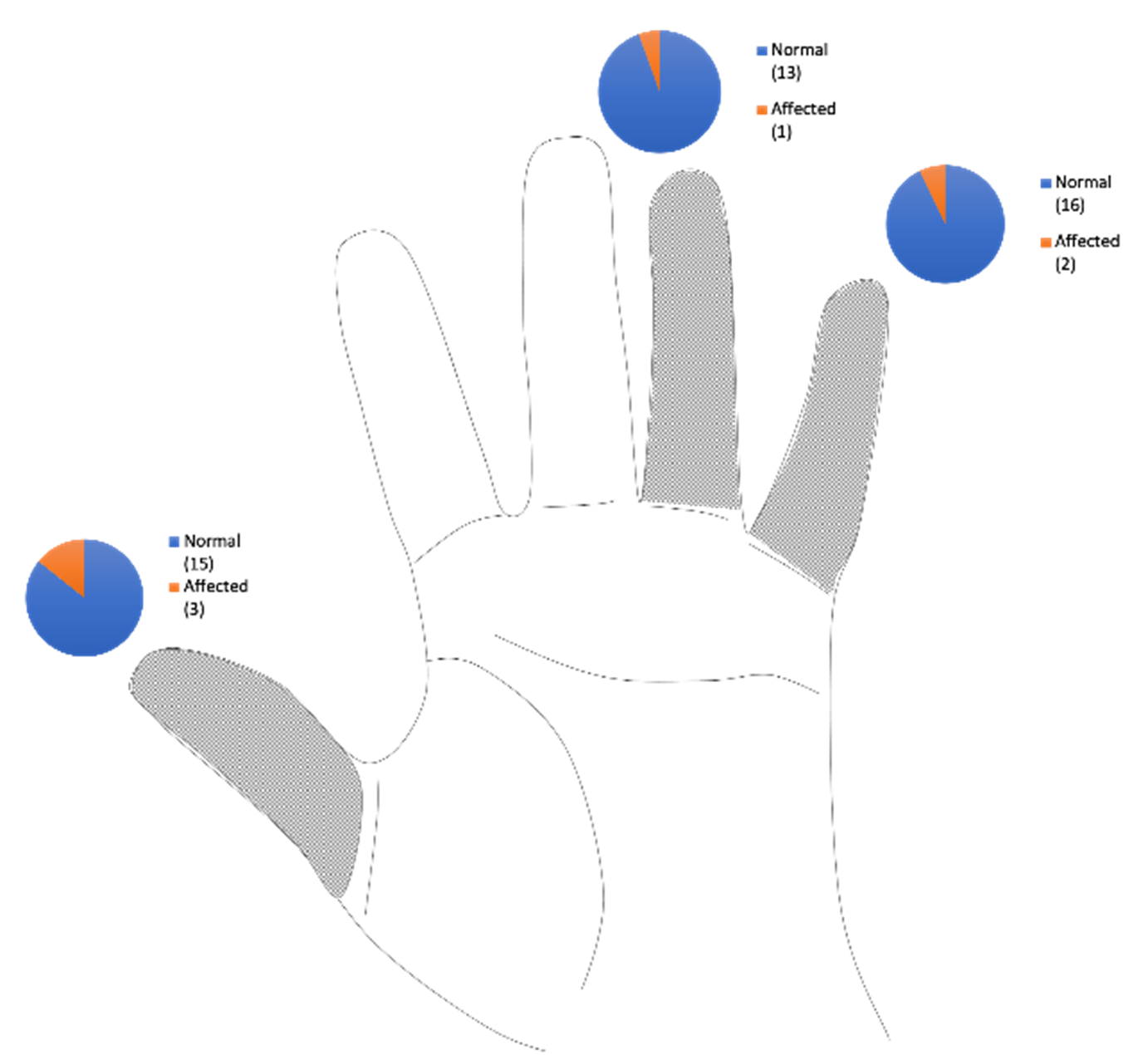
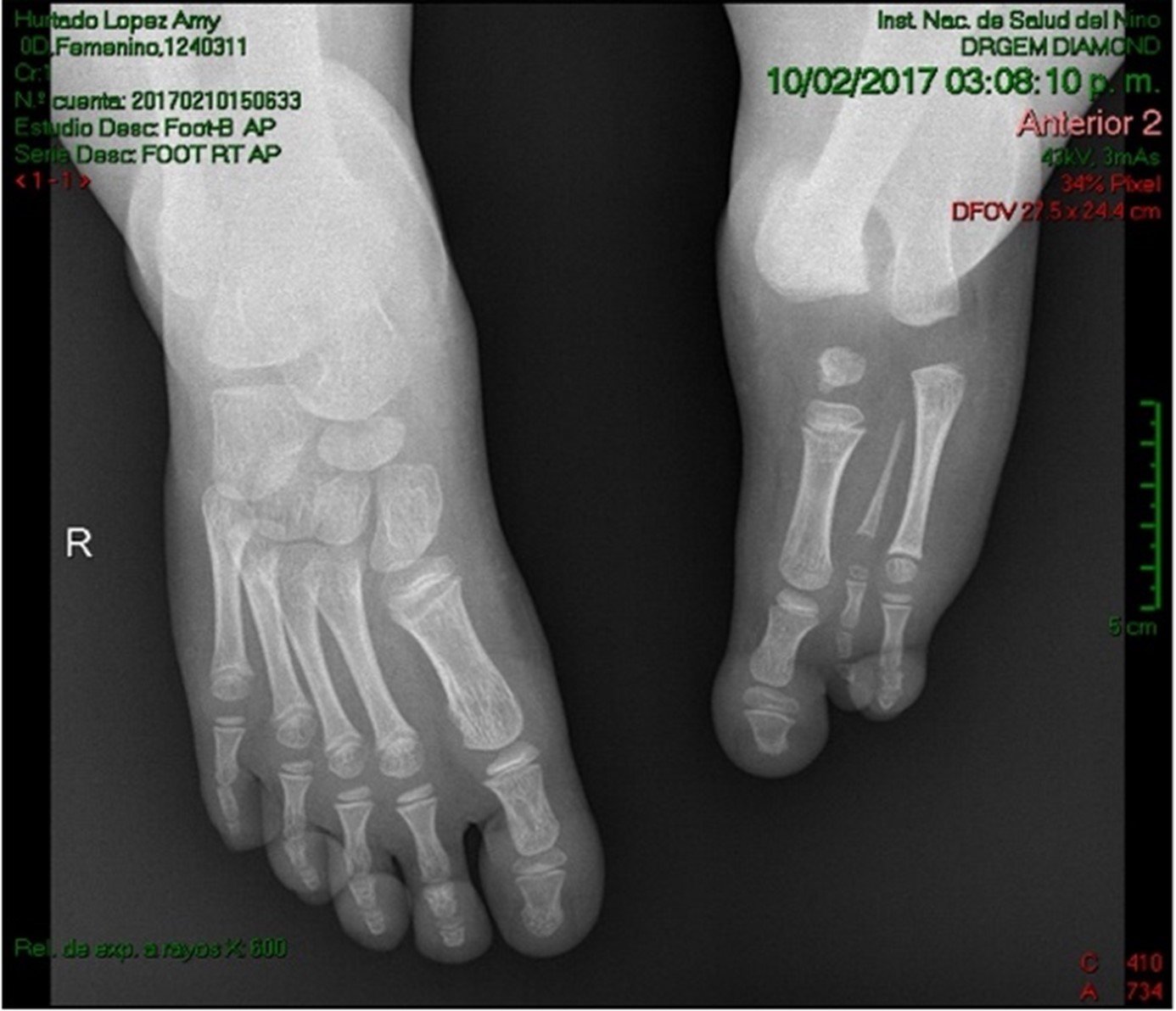
Fibular aplasia of the left limb was observed in six patients, and on the right side in five patients, and fibular hypoplasia in two patients and not specified in one. In one patient the presence of oligodactyly was descr ibed, without specifying the number or side; oligodactyly that included metatarsals, was observed from the 3rd to the 5th toe in three patients (21.4%); only from the 5th toe in two (14.3%) and from the 4th-5th toe oligodactyly in seven patients (50%) (Figure 3 - a and b).
 separacion
separacion
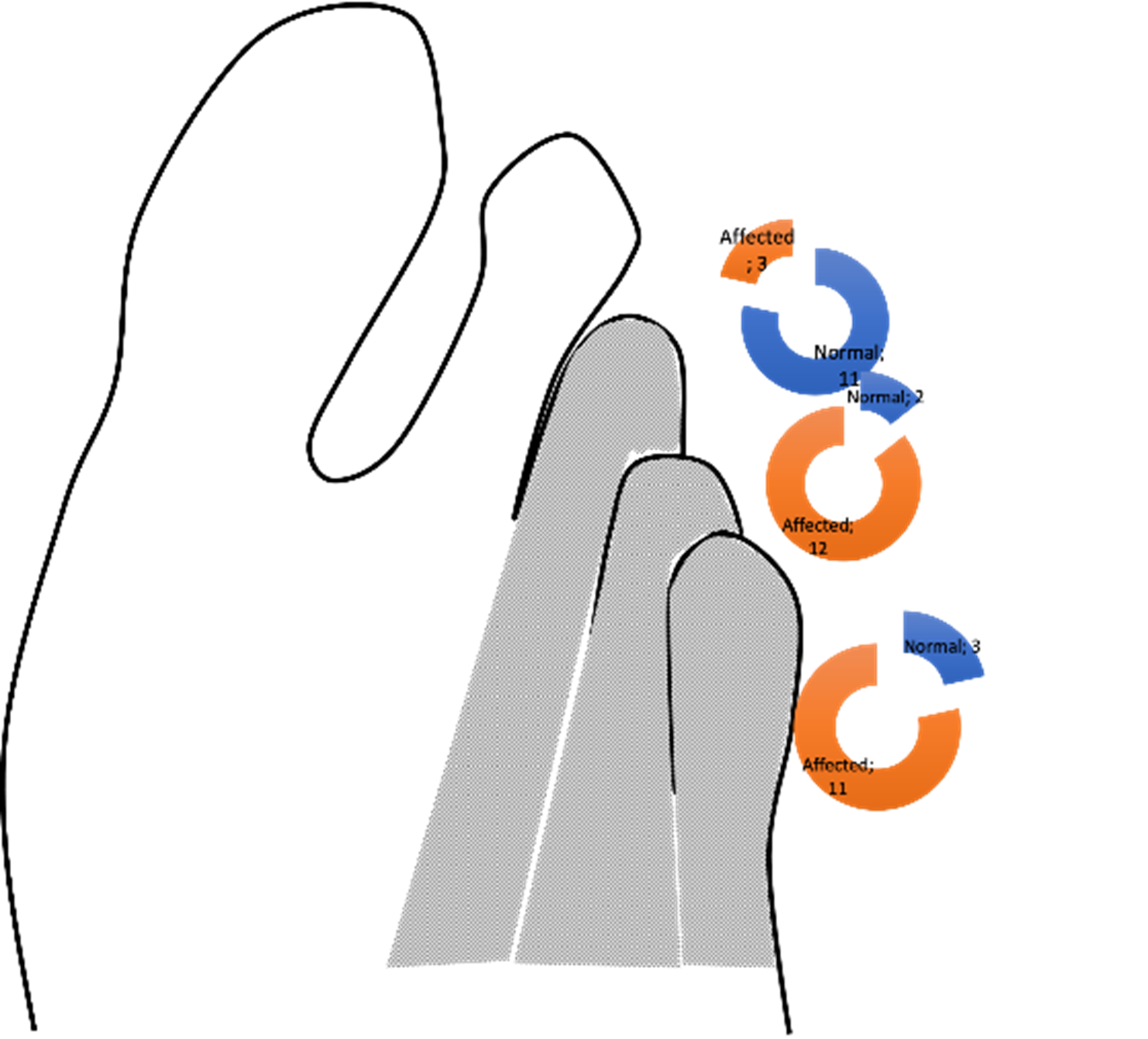
Figura 3. a) X-ray of both feet showing oligosyndactyly in the left foot. b) Frequency of affected toes in the patients described.
Syndactyly of the first and second toe was evidenced in three patients (21.4%). The presence of leg dimpling was present on the right side in five patients (35.7%) and on the left in three patients (21.4%) (Figura 4). Psychomotor development was normal in all patients.
In the hand, anomalies were evidenced in three patients (21.4%), such as the presence of thumb agenesis in two patients (14.2%) and of the fifth finger in one (7.1%), syndactyly of the left hand between the 1st and 2nd fingers, as well as between the 4th-5th fingers in one patient (7.1%) and absence of the fourth metacarpal in one (7.1%) (Figure 5 y Table 2).
DISCUSSIN
The fourteen Peruvian patients represent 50% of all patients reported worldwide to date. (10-24). Upper extremity anomalies were observed in 21.4% of the national cases, while in previous cases it was evident in 2 out of 3 patients reported so far (64.2%).
Early reports on this investigation state that the frequency of the total number of anomalies was the same in both legs. The presence of leg dimpling in this review prevailed in the right lower limb (35.7% vs. 21.4%) and a similar frequency is observed in previous case reports.
Regarding oligodactyly, at the national level, involvement of the 4th-5th toe was more frequently observed, while at the international level, the frequency was higher in the fifth toe (Table 3) (7-22). Syndactyly of the first and second toe was rarely described in patients, but the affected side was only the right in this report and previous manuscripts.
Table 3. Consolidated of all clinical characteristics of patients with FATCO syndrome at the international level (2008 - 2021).
|
Clinical features Upper extremity anomalies |
POSITIVES |
NEGATIVES |
NOT SPECIFIED |
% |
|---|---|---|---|---|
|
Complete syndactyly of left hand 1st-2nd and 4th-5th |
3 |
9 |
3 |
21,4 |
|
3rd-5th cutaneous syndactyly |
2 |
10 |
2 |
14,3 |
|
Absence of fourth metacarpal of hand |
4 |
8 |
2 |
28,6 |
|
Alteration in Hands |
5 |
6 |
3 |
35,7 |
|
Abnormalities in lower extremities |
|
|
|
|
|
Dimple in leg |
11 |
1 |
2 |
78,6 |
|
Absence of 5th ortho |
13 |
1 |
0 |
92,9 |
|
Absence of 4th-5th toes |
6 |
8 |
0 |
42,9 |
|
Absence of 3rd-5th orthotics |
1 |
13 |
0 |
7,1 |
|
Syndactyly of the 1st-2nd orthocylinder |
3 |
11 |
0 |
21,4 |
|
Absence of fibula |
14 |
0 |
0 |
100 |
|
Campomelia of tibia |
14 |
0 |
0 |
100 |
|
Tibial hypoplasia |
12 |
2 |
0 |
85,7 |
|
Other anomalies |
|
|
|
|
|
Nails |
1 |
7 |
6 |
7,1 |
|
Psychomotor development |
0 |
9 |
5 |
0 |
|
Screening for bone anomalies in other regions |
3 |
5 |
6 |
21,4 |
|
Congenital heart disease |
1 |
9 |
4 |
7,1 |
|
Brain MRI |
1 |
5 |
8 |
7,1 |
|
Fundus |
0 |
4 |
10 |
0 |
|
Renal ultrasonography |
0 |
7 |
7 |
0 |
|
Auditory evoked potentials |
0 |
4 |
10 |
0 |
|
Karyotype |
1 |
3 |
10 |
7,1 |
Y/N: not particular; ND: not described; NR: not performed; NS: not specified; Positive: presence of anomaly; Negative: no presence of anomaly
The absence of the fifth metatarsal and its respective phalanges prevailed in the right foot in the Peruvian patients, compared to previous reports, in which it predominated on the left side. Regarding the absence of the fourth metatarsal, this characteristic predominates in this report, presenting in 85.7%. However, in previous descriptions, this characteristic appears in 42.8% of the patients and the absence of the third metatarsal was not a significant finding in the reported cases.
Previous reports, as well as in Peru, described the presence of fibular aplasia predominating in the right leg, which was associated in all patients with tibial campomelia. Previous research shows that tibial hypoplasia was described in 85.7% of the reported cases, with bilateral involvement in 28.6%, also in this study it was observed in all patients without predominance of a lower limb. Previously, a patient with hypoplastic nails was shown, but this anomaly was not observed in any Peruvian patient. Likewise, the screening for bone anomalies in other regions was only present in international patients and was not prevalent in our environment. Regarding psychomotor development, only gait delay was found to be affected, while in Peruvian patients it was not observed (26).
FATCO syndrome is an ultra rare genetic disease, where one of its limitations is the lack of information about this pathology, such as etiology; A recently published study comments on the possible etiology of this syndrome, commenting it as a challenge since it would not be just a monogenic alteration but possibly something more complex as a vascular development disorder, somatic variants or a low level mosaicism in the blood, for which it would be necessary an advance in the technological tools for diagnosis, being for now inaccurate (27). The other limitation found is based on the absence of molecular studies for the diagnosis of FATCO syndrome, and in addition there are genetic diseases that have some of the clinical characteristics, but that could be differentiated through the use of diagnostic tools, such as the use of portals like OMIM (On line Mendelian Inheritance in Man-www.omim.org-) or search programs like Face2Gene, Phenomizer or Possum (28-29).
However, this limitation does not affect the study, as it led us to incorporate the phenotypic detail of each patient. And finally, FATCO syndrome does not have a gold-standard test for diagnosis, which, if there were, would facilitate diagnosis at any stage (prenatal and postnatal); however, it is necessary to consider differential diagnoses that many of them have a genetic etiology identified through massive sequencing tests (30-31).
We have not been able to establish, according to what has been reported so far, the reason why in Peru there would be a greater number of patients; however, there is a legend in the Peruvian jungle about the existence of a being who is called Chullachaqui, who has unequal lower limbs, the right one large and the left one small; so we would deduce that this condition has been seen for a long time in this population (32).
In this sense, it is necessary to perform genomic studies such as massive sequencing or the use of microarrays with a greater number of markers in order to detect variants in a single nucleotide, multiple nucleotides or variants in the number of copies, which will serve not only to establish the etiological molecular diagnosis, but also to recognize the processes of embryonic differentiation of the limbs, to establish the risk of family and individual recurrence and to propose future therapeutic improvements. On the other hand, if these studies were not conclusive, epigenetic studies would have to be carried out, as well as expression studies (transcriptome), among others (31-32).
Authorship contribution:
The authors participated in the genesis of the idea, project design, development, data collection and interpretation, analysis of results, and preparation of the manuscript.
Financing:
Self-financed.
Conflict of Interest:
The authors declare that they have no conflict of interest in the publication of this article.
Received:
February 10, 2023.
Accepted:
April 27, 2023.
Correspondence:
Hugo Abarca Barriga.
Address:
CP Medicina Humana. Universidad Científica del Sur.
Telephone number:
979 301 132
E-mail:
habarca@cientifica.edu.pe
Article published by the Journal of the Faculty of Human Medicine of the Ricardo Palma University. It is an open access article, distributed under the terms of the Creative Commons License: Creative Commons Attribution 4.0 International, CC BY 4.0(https://creativecommons.org/licenses/by/1.0/), which allows non-commercial use, distribution and reproduction in any medium, provided that the original work is duly cited. For commercial use, please contact revista.medicina@urp.edu.pe.
BIBLIOGRAPHIC REFERENCES