REVIEW ARTICLE
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2023 - Universidad Ricardo Palma10.25176/RFMH.v23i4.5727
EFFECT OF BARIATRIC SURGERY ON QUALITY OF LIFE IN OBESE PATIENTS: A GLOBAL SYSTEMATIC REVIEW
EFECTO DE LA CIRUGÍA BARIÁTRICA SOBRE CALIDAD DE VIDA EN OBESOS: UNA REVISIÓN SISTEMÁTICA GLOBAL
Nayaret Vega-Albornoz
 1,a
1,a
Ornela Navarro-Mora
 1,a
1,a
Miguel Ángel López-Espinoza
 1,2,b
1,2,b
1 Faculty of Health, Universidad Santo Tomás, campus Talca, Chile
2 Nutrition and Dietetics Degree, Faculty of Health Sciences, Universidad Adventista de Chile. Chillán, Chile.
a Bachelor in Nutrition and Dietetics
b Nutritionist, Master in Public Health, PhD student in Health Sciences.
ABSTRACT
In a situation of obesity and when treatment goals are not met, bariatric surgery can be a promising alternative; with effects at the physical level as well as at the psychological level of the quality of life. This study aims to determine the effect of bariatric surgery on the quality of life in obese men and women between 20 and 60 years of age. A systematic review (SR) was carried out with meta-analysis of randomized systematic reviews, which compare the quality of life in patients after bariatric surgery. Electronic databases were consulted: Ebsco, Scopus, Pubmed and Cochrane Library. The response variables were: physical, social, mental and emotional function. They were submitted to meta-analysis, with R 4.2.2. Three SR were included, of which 25 clinical trials were combined with 3-6 and 12-month follow-up after bariatric surgery, finding statistically significant changes in physical function scores (1.20; 95% CI: 0.80-1 .61), social (0.95; 95% CI: 0.66-1.25), mental (0.35; 95% CI: -0.21- +0.90) and emotional (0.54; 95% CI: 0.03-1.06). The surroundings of the quality of life improve post bariatric surgery in obese patients.
Keywords: Bariatric surgery, quality of life, obesity, systematic review, meta-analysis (source: MeSH – NLM)RESUMEN
En situación de obesidad y cuando no se logra cumplir las metas del tratamiento, la cirugía bariátrica puede ser una alternativa prometedora, con efectos, a nivel físico y en el plano psicológico de la calidad de vida (CV). Este estudio tuvo como objetivo determinar el efecto de la cirugía bariátrica sobre la CV en hombres y mujeres obesas entre 20 y 60 años. Se realizó una revisión sistemática (RS) con metanálisis de RS aleatorizadas, que comparan la CV en los pacientes poscirugía bariátrica. Fueron consultadas las bases de datos electrónicas Ebsco, Scopus, Pubmed y Cochrane Library. Las variables de respuesta fueron las dimensiones función física, social, mental y emocional de la CV. Se sometieron a metanálisis con R 4.2.2. Se incluyeron tres RS, de las cuales se combinaron 25 ensayos clínicos con 3-6 y 12 meses de seguimiento poscirugía bariátrica. Se encontraron cambios estadísticamente significativos de los puntajes en función física (1,20; IC 95%: 0,80-1,61), social (0,95; IC 95%: 0,66-1,25), mental (0,35; IC 95%: -0,21- +0,90) y emocional (0,54; IC 95%: 0,03-1,06). Los ámbitos de la CV mejoran poscirugía bariátrica en pacientes obesos.
Palabras clave: Cirugía Bariátrica, calidad de vida, obesidad, revisión sistemática, metanálisis (fuente: DeCS – BIREME)Bariatric surgery is an alternative aimed at patients who are morbidly obese or have failed many times with the recommended conventional treatments, such as changes in lifestyle and eating habits (1). This problem implies a chronic and progressive clinical condition, characterized by an excessive or abnormal accumulation of body fat that negatively affects cardiovascular health, high blood pressure, type 2 diabetes mellitus, alterations in the lipid profile and musculoskeletal disorders (2, 3). The selection criteria to carry out bariatric surgeries are: having a body mass index (BMI) >40 kg/m2 or BMI >35 kg/m2 with comorbidities (among the most common: type 2 diabetes mellitus, hypertension, dyslipidemia , obstructive sleep apnea, reflux, venous thrombosis), obesity sustained over time for more than five years, without a history of alcoholism, drugs or serious psychiatric illnesses, patients who are in the age range between 20 and 60 years and, Lastly, they must be aware of the alterations that this intervention produces (4). There are different types of bariatric surgery: absorptive, malabsorptive and mixed. These types also have a classification level according to the surgical resection performed; This is how, in turn, they were also classified into: gastric sleeve, biliopancreatic diversion and gastric bypass. (5).
Health-related quality of life (HRQoL) is used interchangeably as health status, functional status, QoL or needs assessment. In relation to the QoL of patients undergoing bariatric surgery, the literature expresses that it is necessary to continuously assess both short and long term (6). The impact of bariatric surgery on QoL is fundamental, since this type of intervention can not only improve mobility and reduce comorbidities related to obesity; Additionally, it may influence mental and social function, which may aid adherence to postoperative treatment.
To date, there is a large volume of SRs that have evaluated different dimensions of QoL, according to prominent schools of thought. For example, in the last five years, seven publications have been found (7, 8, 9, 10, 11, 12, 13); however, this evidence is scattered in multiple databases with discrepancies in the results provided by some SRs; some point out that post-bariatric surgery depression in patients decreases in the number of patients who undergo bariatric surgery and that the number of patients who undergo bariatric surgery decreases in the number of patients who undergo bariatric surgery. (7) and others conclude that this is maintained over time, so psychological treatment requires more time to achieve improvement. (8). Therefore, our study is linked to generating a global systematic review, which covers in a single text an important sample of SRs that allow the clinician to access the information in a single document.
In this study, we aimed to determine the effect of bariatric surgery on QoL based on the dimensions of social, mental, physical and emotional function in obese patients.
Review design
This study corresponds to a global systematic review (14) that subscribes to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) screening guideline (15).
Eligibility criteria
SRs with meta-analysis were included, which studied patients of both gender; between 20 and 60 years old; who underwent bariatric surgery with the purpose of demonstrating an improvement in postoperative QoL validated with the Short Form Health Survey (SF-36) instrument.
Search strategy
The search period was between March and October 2022. Keywords extracted from medical subject headings (MeSH) and free text terms extracted from the specific language of the subject were used (Table 1). In their entirety, the keywords addressed all elements of the PICO question format (patients, intervention, comparison, and outcome). The databases were used: Scopus, Ebsco, PubMed and Cochrane Library. Inclusion was not limited by the language of the studies evaluated.
|
Strategy |
Free keywords |
MeSH |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
Patient |
Adult |
Obesity (ID: D009765) |
|||||||||
|
Intervention |
Bariatric Surgery |
Bariatric Surgery (ID: D050110) |
|||||||||
|
Intervention |
Biliopancreatic Diversion |
||||||||||
|
Control |
Control |
Control |
|||||||||
|
Outcome |
Quality of life |
Quality of Life (ID: D011788) |
Selection of studies
Two previously trained independent researchers (ON and NV) selected SRs, based on their titles and abstracts, according to the defined eligibility criteria. SRs were subsequently classified as “included,” “excluded,” and “uncertain.” With respect to the cases evaluated as “uncertain”, their methodologies were read to make a decision within “included” or “excluded”. Afterwards, the evaluators compared their classifications and in cases of disagreement, a third reviewer (ML) was used, who acted as a mediator and, based on the eligibility criteria, decided to include or exclude the SR in question. Likewise, those SRs that were duplicated were discarded. The second stage consisted of reviewing the full text of the included studies to thoroughly analyze their relevance to the topic under study. This review, too, was carried out independently by the two reviewers, who decided whether the studies would finally be included in this SR, according to the aforementioned eligibility criteria. Any disagreement between both parties was resolved once again, with the guidance of a third methodological expert (ML).
Data extraction
The same two researchers mentioned above independently extracted the study characteristics, population, intervention, and main results from the published articles. PRISMA guidelines were applied (15) to facilitate the critical reading and interpretation of the SR.
Data synthesis
The weighted mean differences (WMD) were calculated with a random effect, assuming that the studies that entered these meta-analyses are a sample and, therefore, have intra- and inter-study variability. Heterogeneity of studies included in all meta-analyses was assessed with I2. The potential publication bias was studied with Kendall's tau coefficient and with regression models on the solution of the meta-analysis (linear model). The metafor package was applied(16) in R, version 4.2.2 (17).
Search results
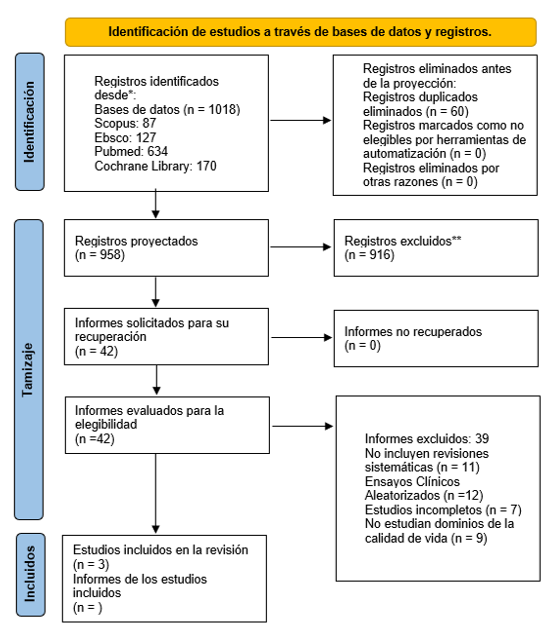
The search process for the included articles is presented in Figure 1. Three SRs published in 2022 or earlier were included and were used for the description in the qualitative phase. A meta-analysis was performed on the three studies included in this systematic review. (18, 19, 20).
Characteristics of the included studies
The main characteristics of the included studies are available in Table 2. One study was found in the United Kingdom (SR with meta-analysis). (18), one in the Netherlands (SR) (19) and one in Poland (SR) (20). The mean ages of the patients ranged between 30 and 46 years. Postintervention follow-ups lasted from three months to 10 years.
|
First author, year |
Design |
Study population |
Intervention |
Control |
Duration |
||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Herring, 201618 |
Systematic review with meta-analysis |
Sample of 1845 patients, including men and women. |
Bariatric Surgeries: |
Pre- and post-operative evaluation was performed using the SF-36 questionnaire to determine the physical function of the patients. |
Follow-up ranged from 3-6 months and 12 months |
||||||||||||||||||
|
Raaijmakers, 201619 |
Systematic review |
Sample of 7720 patients, including men and women. |
Bariatric surgeries: |
Sleeve gastrectomy Pre and postoperative evaluation was performed using the SF-36 questionnaire to determine the physical, emotional, social and mental function of the patients. |
Follow-up ranged from 6 months to 10 years. |
||||||||||||||||||
|
Sierzantowicz, 202220 |
Systematic review |
Sample of 11708 patients, including men and women. |
Bariatric surgeries: |
Pre and postoperative evaluation was performed using the SF-36 questionnaire to determine physical, mental, social and emotional function. |
Follow-up varied between 0, 1, 2, 3, 4, 6, 8 and 10 years. |
One study included gastric bypass and gastric banding interventions and addressed pre- and postoperative physical function of patients with 3-6 months and 12 months follow-up. (18). One study included gastric bypass, biliopancreatic diversion, gastric banding and sleeve gastrectomy surgeries and addressed physical function, mental function, social function and emotional function pre- and postoperatively with a 12-month follow-up (19). One study included the bariatric surgeries laparoscopic gastric banding, laparoscopic adjustable gastric banding, Roux-en-Y gastric bypass, biliopancreatic diversion with duodenal switch and sleeve gastrectomy, and analyzed physical function, mental function, social function and emotional function pre- and postoperatively with a 10-year follow-up (20). These three studies used the SF-36 measurement instrument to measure QoL domains in patients before and after surgery.
Meta-analysis calculation
Meta-analyses were obtained to calculate weighted mean differences (WMD) from the original studies rescued from the three SRs. (18, 19, 20). Studies with a follow-up time of 3-6 and 12 months were selected for further analysis (Table 3). It was observed that after bariatric surgery, QoL dimensions increased (WMD = 1,00; CI del 95%= 0,69-1,30; I2=96,78%, Q=678,17; p<0,001). Kendall's tau coefficient with all studies involved was 0.02, with p=0.8485. The funnel plot asymmetry test shows a z value=0.36; with p=0.7223 (beta=0.89; 95% CI: 0.25-1.54).
Regarding the variable of physical function after bariatric surgery, all the studies of one SR (18) plus studies from the other two SRs were rescued (19, 20). It was observed that after bariatric surgery, physical function had a significant change (WMD= 1,20; CI del 95%= 0,80-1,61; I2=94,9%; Q=315,1; p<0,001). Kendall's tau ordinal correlation coefficient was -0,02 (p=0,8700). The asymmetry test presented a z value = -0.99; with p=0.3209 (beta=1.71; 95% CI: 0.63-2.78).
With respect to mental function, studies of two SR were obtained19,20 and it was obtained that after bariatric surgery mental function had a significant change (WMD= 0,35; CI del 95%= −0,21- +0,90; I2=96,45; Q=119,37; p<0,001). Kendall's tau coefficient was -0,67 (p=0,1172). The funnel plot asymmetry test had a value z=-1,31; with p=0,1918 (beta=2,90; CI95%: -0,97- +6,77).
For the social function, studies were rescued from the same two SRs for the previous case (19, 20) and a significant change was found (WMD = 0.95; 95% CI= 0.66-1.25; I2= 81.67%; Q=11.67; p=0.0029). Its Kendal tau coefficient had a value of -0.33 (p=1.000). The funnel plot asymmetry test had a z value = -0.65; with p=0.5170 (beta=2.12; 95% CI: -1.42- +5.65).
Regarding emotional function, there were also studies of the same two SRs mentioned above (19, 20), where it was noted that after bariatric surgery, emotional function showed a significant change (WMD= 0.54; CI of 95%= 0.03-1.06; I2=94.35%; Q=39.63; p<0.001). Kendal's tau coefficient presented the same value and statistical significance as the previous case. The funnel plot asymmetry test had a z value = -0.54; with p=0.5886 (beta=2.35; 95% CI: -4.22- +8.93).
The effect of the moderating variable time of the intervention (in two groups: 3-6 months, compared to the time of 6-12 months) was evaluated with respect to the relationship between the evaluated intervention and QoL score (without stratifying by dimension, considering all studies: k=36); it was found that it did not have a significant influence (beta=-0.45; SE=0.33; 95% CI: -1.09- +0.19; p=0.1641 ).
The results of our systematic review and meta-analysis aimed to determine the effect of bariatric surgery on QOL in obese men and women, in an age range of 20 to 60 years. In this context, we found that physical, social, mental and emotional function had favorable changes in terms of QoL in a period of 3 to 12 months after surgery. This implies a very short-term improvement in health indicators related to obesity-associated diseases, a decrease in anxiety and body image distortion, and a better social adaptation.
In addition, the time that passes after the intervention is crucial, as studies have shown that scores in each area can be affected over time. (21), Since patients tend to adhere to post-surgical treatment during the first year, such as the diet and lifestyle recommendations. After this time, this adherence decreases (20).
In this context, we found inconsistent evidence of long-term QoL after bariatric surgery, since some studies suggest that HRQoL improves up to the first year and then stabilizes or decreases its values (22), while others suggest that HRQoL continues to improve over time two or four years (23).
Also, we found evidence that the changes depend on the QoL dimension being studied, as shown by Youssef et al (24), who followed up physical and mental functions for three years after bariatric surgery, and found initial improvements at one year in physical function, while mental function decreased within the first six months at one year of follow-up, and then observed improvements after two years post-surgery. This may be due to the lack of nutritionists, psychologists, kinesiologists, among others, who continue the post-surgical treatment from their areas of expertise, due to the absence of controls with them, lack of adherence to their treatments (due to the perception that the problem is solved with bariatric surgery), lack of attention to previous psychiatric pathologies and their postoperative surveillance. This is why it is recommended to promote multidisciplinary and coordinated work according to the patient's needs, since surgery does not treat obesity in itself, but reduces dietary intake, and should not be understood as a replacement for treatment linked to promoting long-term protective factors, which will be the acquisition of healthy lifestyles, including a healthy diet and physical exercise, as well as implementing a permanent surveillance as a result of surgical treatment (e.g. supplementation) and psychiatric treatment; it is considered that, of this type of patients, between 8.8 and 37.5% commit suicide (25).
The above implies that although the physical well-being of patients after bariatric treatment may show persistent improvement, the same would not occur with mental well-being. Some individuals may even show some mental health disorders such as an increased tendency toward suicidal ideation (as the most extreme case), anxiety, depression, and decreased sense of control(20). However, Szmulewicz et al. (26) published a study of mental health QoL with a follow-up that varied from 12 to 36 months, which demonstrated that improvements in mental health QoL tended to be small and variable, so that the Surgery was not associated with an improvement in mental health QoL compared to non-surgical intervention. For this reason, intensive psychiatric observation of patients with preexisting mental conditions after bariatric surgery should be considered. Therefore, it cannot be ruled out that, due to these existing problems, these patients comply less with postoperative recommendations, which would lead them to regain weight more quickly, which would lead to a deterioration in their HRQoL in the long term.
As for the social environment, there was an increase at 12 months, after the postoperative period, which means that this would also improve the QoL of patients with obesity. However, the role of the family environment in postoperative outcomes is a topic that is often complex to evaluate. Some studies and reviews evaluating the social environment suggest that previous research is limited by poorly validated instruments (27, 28) or small samples of participants (29,30), which would make it difficult to analyze.
For the emotional variable, this variable showed improvements after 12 months postoperatively. A study reveals that this would be possible thanks to the work carried out together with the psychology team, in which the patient is evaluated to ensure that he/she is able to manage his/her affective problems and emotional suffering. In this, the learning of new skills that are easy to manage for the patient is promoted and, in turn, to establish changes in patterns, both at the level of thought and behavior. In addition, these patients should be monitored for the new behaviors they adopt with themselves and with others, so that, in this way, they can opt for wellbeing. (31). However, Wong LY et al. (32), in a study, proposed that the improvement in this area is due to the change that occurs in emotional eating, which would significantly improve in the first 12 months after bariatric surgery. Emotional eating, generally, occurs due to an inclination towards foods that are usually tasty, so, after the surgical intervention, it happens that these patients usually avoid these types of foods, and thus, the emotional environment has improved. postoperative.
This study has not been free of limitations. The first has to do with the small number of SR that we were able to compile, which could have resulted in the external validity of the study, even though some inclusion criteria were open, such as the age range, the language of the studies or any surgical technique used. However, we were able to extract a significant number of studies to analyze the effectiveness of the intervention (for example, the physical function dimension included 25 studies). A second limitation has to do with the high heterogeneity of the studies that participated in the meta-analyses performed; therefore, the interpretation of these results should be taken very cautiously. We worked with meta-regressions thinking that the time variable could have influenced the inter-study variability, since the longer the time after surgery, the lower the scores for the physical domain of QoL tend to be (33) and, thereby, reduce I2, but this objective was not achieved. Other moderating variables (e.g., clinical, treatment, and design characteristics) were not considered, because they were not available in all the original studies. According to the asymmetry tests performed in the meta-analyses, the evidence shows an absence of publication bias, so the variability of the results is only more linked to heterogeneity.
We found, for the most part, studies of short and moderate duration, so the results that could occur in the long term, once patients undergo bariatric surgery, are unknown. However, short-term studies had a positive impact on the variables and based on this context it was possible to verify that QOL increases.
With this systematic review, the current state of research is evidenced regarding the effectiveness of bariatric surgery on QoL in obese patients.
In conclusion, there is evidence that suggests a favorable relationship between bariatric surgery and HRQoL with adequate follow-up for patients, which generates changes in different variables such as physical, mental, social and emotional function. However, the meta-analyzed evidence should be considered with caution, due to the high degree of heterogeneity of the studies.
The increase in the number of post-bariatric surgery settings helps to improve the QoL of the intervened groups, during an established time; in studies with an intervention time of 3-6 months and one year, it presented significant changes. However, it is important to follow up the intervened patients in order to ensure their improvement over a long period of time and to evaluate with validated tools to detect possible complications in the future.
Authorship contributions:
ON-M participated in the conception of the article, data collection, writing and approval of the final version. NV-A participated in the conception of the article, data collection, writing, and approval of the final version ML-E participated in the conception of the article, the statistical analysis of data, its writing, and approval of the final version.
Financing:
Self-financed
Declaration of conflict of interest:
The authors declare that they have no conflicts of interest.
Recevied:
June 2, 2023
Approved:
October 8, 2023
Correspondence author:
Prof. Miguel López-Espinoza
Address:
Campus Centro de Alto Rendimiento (CAR), Avenida Circunvalación Poniente #1855, Talca, Chile
Phone:
+56942629804
E-mail:
mlopez34@santotomas.cl
Article published by the Journal of the faculty of Human Medicine of the Ricardo Palma University. It is an open access article, distributed under the terms of the Creatvie Commons license: Creative Commons Attribution 4.0 International, CC BY 4.0 (https://creativecommons.org/licenses/by/1.0/), that allows non-commercial use, distribution and reproduction in any medium, provided that the original work is duly cited. For commercial use, please contact revista.medicina@urp.edu.pe.
BIBLIOGRAPHIC REFERENCES