CLINICAL CASE
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2024 - Universidad Ricardo Palma10.25176/RFMH.v24i1.5905
LYMPH NODE TUBERCULOSIS WITH GENITAL INVOLVEMENT: CASE REPORT
TUBERCULOSIS GANGLIONAR CON COMPROMISO GENITAL: REPORTE DE CASO
Joel Isaac Atencio Paulino
 1,a
1,a
Waldir Paucar Huaman
 2,a
2,a
Deivi Nick Galarza Caceres
 2,b
2,b
Jeampier Bendezu Meza
 2,b
2,b
Jhonatan Mauricio Crispin Ayala
 2,b
2,b
1 Universidad de San Martín de Porres, Lima, Peru.
2 Faculty of Human Medicine, Universidad Nacional del Centro del Perú, Huancayo, Peru.
a General Physician
b Medical Student
ABSTRACT
The case of a 44-year-old male patient with a family history of lymphoma and hyperthyroidism is
presented. His disease started three months prior to hospital admission with pain in the right leg and
abdomen, weight loss, and night sweats. Upon admission, he was diagnosed with pelvic ascites of
undetermined etiology and multiple polygastric and right iliac fossa lymph nodes. Six months later, his
symptoms persisted, and a nodule appeared on his penis, along with left testicular edema and purulent
discharge from the right inguinal lymph node; orchioepididymitis was diagnosed. Initially, tuberculosis
(TB) markers were negative; however, a lymph node biopsy and analysis with Xpert MTB/RIF were performed,
yielding a positive result. The patient showed significant improvement with anti-TB treatment and
antibiotics for the purulent discharge.
Keywords: Extrapulmonary tuberculosis, lymph node tuberculosis, late diagnosis. (Source: MeSH).
RESUMEN
Se presenta el caso de un paciente varón de 44 años con antecedentes familiares de linfoma e
hipertiroidismo. Él inició la enfermedad tres meses antes del ingreso hospitalario con dolor en la
pierna derecha y abdominal, pérdida de peso y sudoración nocturna. Fue diagnosticado en su internamiento
con ascitis en cavidad pélvica de etiología indeterminada, y múltiples adenomegalias poligástricas y en
fosa iliaca derecha. A los seis meses, los síntomas persistieron y se agregó un nódulo en el pene, edema
testicular izquierdo y secreción purulenta del ganglio inguinal derecho; se diagnosticó
orquiepididimitis. Inicialmente, tuvo marcadores negativos para tuberculosis (TBC), sin embargó, se
realizó biopsia del ganglio y el análisis con Xpert MTB/RIF, lo que resultó positivo. El paciente mejoró
considerablemente con tratamiento anti TB y antibióticos para la secreción purulenta.
Palabras clave: Tuberculosis extrapulmonar, tuberculosis ganglionar, diagnóstico tardío. (Fuente:
DeCS).
INTRODUCTION
A 44-year-old male patient presented with nonspecific initial symptoms such as intermittent pain in the
right leg and epigastrium radiating toward the flanks; subsequently, weight loss, night sweats, nausea,
headache, and general discomfort were added. The Centers for Disease Control and Prevention (CDC)
reported that, in the U.S., 20.6% of tuberculosis (TB) cases were extrapulmonary, with the most frequent
being the ganglionar at 38.2% of all forms(1). Ganglionar tuberculosis or
tuberculous lymphadenitis, is
one of the most common forms of extrapulmonary tuberculosis(2); its most
common location is the cervical
region, known as scrofula (3). In Peru, around 27,000 cases of active
disease are reported, and we are
one of the countries with the highest number of extrapulmonary tuberculosis cases in the Americas
(4).
Cervical infection would occur through direct contact of the bacilli with Waldeyer's ring, and in the
peripheral ganglionar form, the pathogenic mechanism would be the reactivation of an infection by
primary pulmonary TB disseminated hematogenously (5). The most common
presentation of peripheral
ganglionar TB is the appearance of painless unilateral cervical lymphadenopathy (83%); other less
affected lymph node groups are axillary and mediastinal (3). Bilateral
involvement occurs in 26% and is
frequent in HIV-positive patients; most patients present with lymph nodes between 1-3 cm in diameter
(6). The definitive diagnosis is made by positive culture for M.
tuberculosis, confirmed by lymph node
bacilloscopy, but its sensitivity is low, so the Xpert MTB/RIF molecular method by polymerase chain
reaction (PCR) is useful due to its high sensitivity (6, 7). According to the Ministry of Health of Peru
(MINSA), therapy is based on rifampicin, isoniazid, ethambutol, and pyrazinamide daily for two months,
followed by rifampicin and isoniazid three times a week for four more months, to complete six months
(7). A case is presented of a patient treated in Huancayo, then referred to
the city of Lima for
molecular laboratory analysis, where ganglionar TB was found with a good outcome, in order to highlight
the rarity of the case and its interest and study potential, since extrapulmonary tuberculosis, in
general, represents a smaller proportion of cases compared to pulmonary tuberculosis. We sought to
understand the factors that contributed to the late diagnosis of ganglionar tuberculosis with genital
involvement in this patient and evaluate the impact of such delay on his health and the course of the
disease.
CASE REPORT
The patient was a 44-year-old male, of Christian religion, and employed as a car painter, residing in
the city of Concepción-Junín, Peru. He reported a family history on his sister's side: hyperthyroidism,
and his maternal grandmother with non-Hodgkin lymphoma. He reported no addictions or adverse drug
reactions. The patient began with nonspecific symptoms: intermittent pain in the right leg and
epigastrium radiating towards the flanks over the course of three months; progressively, weight loss,
night sweats, nausea, headache, and general discomfort were added. In early July 2022, he visited a
private clinic where physical examination revealed stable vital signs, absence of lymphadenopathy, and
no abnormalities in the respiratory or cardiovascular examination. Hemogram, complete urine examination,
tests for HIV, hepatitis B, C, and venereal diseases were negative. Upper abdominal ultrasound described
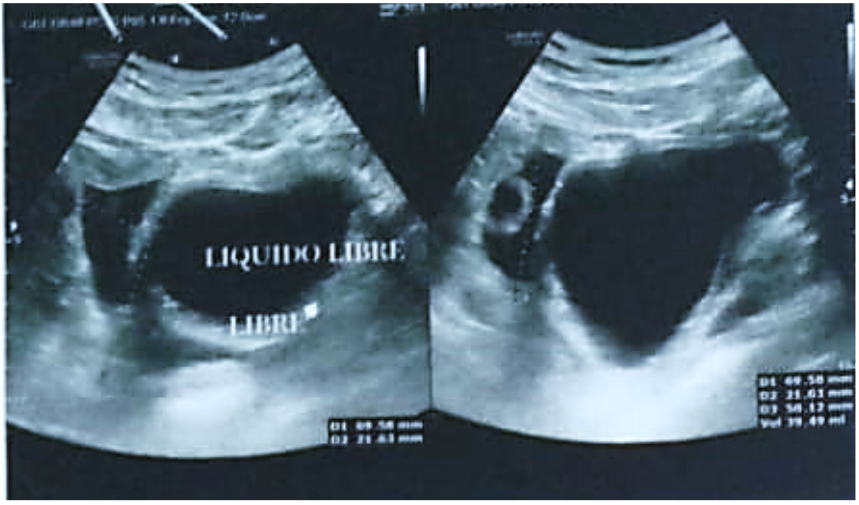
hepatomegaly associated with ultrasound signs of hepatic steatosis, nonspecific pelvic collection,
lithiasic cholecystopathy without acuteness, and uncomplicated fatty umbilical hernia. Contrast-enhanced
chest and abdomen computed tomography (CT) showed marked streaking of the fat planes diffusely
throughout the abdomen associated with multiple epigastric and right iliac fossa lymph nodes, with the
largest reaching a caliber of 10 mm, with a probable inflammatory aspect. Later that same month, in the
Gastroenterology department, bilateral inguinal lymph nodes < 1cm were described, with a positive
wave sign and displaceable dullness (+); pathological anatomy following endoscopy revealed abundant
lymphocytes without atypia, making it impossible to rule out MALT lymphoma, suggesting post-treatment
follow-up. In mid-August, the patient was admitted to Huancayo Hospital for further studies; he
underwent laboratory tests (serological, biochemical, urinary, immunological, and tumor markers), which
returned normal results with slight anisocytosis, as seen in Table 1. Sequenced chest X-ray showed no
abnormalities. Tests for brucellosis, bartonellosis, sputum bacilloscopy culture for BK, and purified
protein derivative (PPD) skin test were negative; additionally, Rheumatology ruled out autoimmune
processes. Ultimately, no definitive diagnosis was made; only symptomatic treatment was provided, and
the patient was discharged. After five months of hospitalization, in January 2023, the patient continued
to experience symptoms and reported a painless 1 cm nodule on the penile shaft initially without signs
of inflammation. He sought care at the Urology department of Hospital de Huancayo, where he was
diagnosed with penile nodules, orchitis, and epididymitis; complete urine examination was normal, and
Doppler ultrasound showed no significant changes; he was prescribed antibiotics and tramadol for
conditional pain relief. One month into the clinical presentation, the patient developed right flank
ascites and increased testicular volume with purulent discharge from the penile nodule and right
inguinal region, prompting serum alpha-fetoprotein, chorionic gonadotropin, and another Doppler
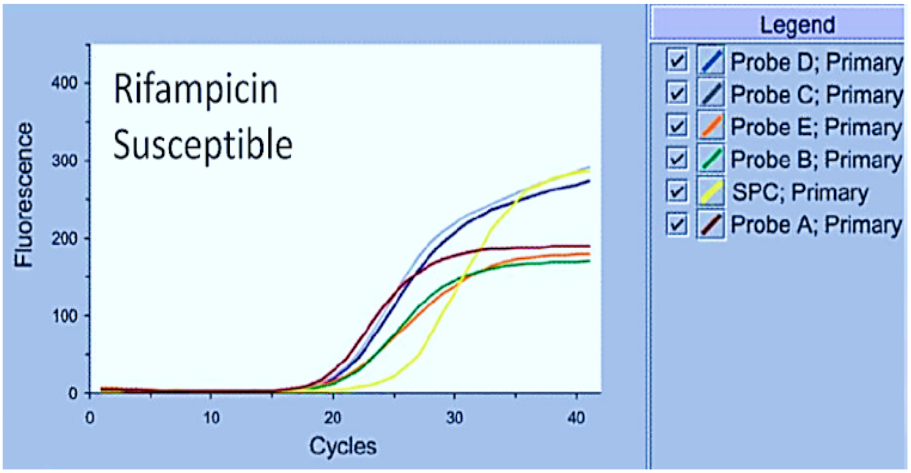
ultrasound, all of which returned normal. At the end of February 2023, prompted by a family member and
another physician, he visited a private laboratory in Lima, where inguinal lymph node biopsy was
performed and GeneXpert molecular profiling for TB by PCR was positive, as shown in Figure 1;
simultaneously, gram staining, leukocytes, bacterial flora, and culture were negative. With these
results, the diagnosis of extrapulmonary ganglionar TB was confirmed, and he was referred to the
Infectious Diseases department of his local hospital, where he was started on antituberculous treatment
with H, R, E, Z, and pyridoxine. The patient improved regarding his symptoms, and the genital and
inguinal lesions resolved; he is currently on a high-protein diet and is being monitored by the nearest
health center to his residence.
|
Exams |
Result |
Normal Value |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
ESR |
12 mm/h |
0-15 mm/h |
|||||||||
|
C-reactive protein |
71.41 mg/dl |
< 1 mg/L |
|||||||||
|
Leukocytes |
12 210 |
4,500-11,000 cells/mL |
|||||||||
|
Hemoglobin |
13,3 g/dl |
13,4-17,5 g/dL |
|||||||||
|
Hematocrit |
43 |
38-54 % |
|||||||||
|
Platelets |
431,000 |
150,000-450,000 platelets x mL |
|||||||||
|
Neutrophils |
73.3 % |
40-60 % |
|||||||||
|
Lymphocytes |
15.6 % |
20-40 % |
|||||||||
|
Brucellosis Rose Bengal Test |
Negative agglutination |
||||||||||
ESR: Erythrocyte Sedimentation Rate
DISCUSSION
The diagnosis of extrapulmonary tuberculosis represents a challenge due to its nonspecific symptoms and
varied presentation. Most infections occur in the cervicofacial region, and those diagnosed in the
inguinal region are rare. A systematic review reported only 15 cases of inguinal tuberculous
lymphadenitis from 2003 to 2021 (8), underscoring the importance of this
case. Tuberculosis accounts for
up to 43% of peripheral lymphadenopathies and is endemic in resource-limited settings (9).
Extrapulmonary tuberculosis occurs in up to 60% of HIV-infected patients and often presents with signs
of pulmonary involvement (10). Most reported cases, including inguinal
locations, are associated with
tuberculous involvement elsewhere in the body (11). The pathogenesis of
inguinal tuberculosis is
unclear; two hypotheses are possible: hematogenous spread from a primary pulmonary focus and secondary
isolated involvement of inguinal lymph nodes, or lymphatic spread from male genital ducts preceding
infection from the upper urinary tract (11). In the present case, CT and
chest X-ray did not show
imaging signs suggestive of primary pulmonary TB such as fibrosis, pulmonary infiltrates, or mediastinal
lymphadenopathies. Late inguinal lymphadenopathies were evident on clinical examination; regarding the
literature, inguinal tuberculous lymphadenitis presentation is more commonly unilateral (12). There was
a nonspecific pelvic collection on abdominal ultrasound; CT described polygastric and right iliac fossa
lymph nodes, and a positive wave sign and displaceable dullness, which is not frequent in the literature
(13). On the other hand, in this report, BK cultures in sputum and PPD for
tuberculosis were negative.
The diagnosis of tuberculous infection should be considered in the differential diagnosis when the
etiology of lymphadenitis is not easily explained. The initial manifestations of inguinal tuberculous
lymphadenitis are characterized by chronicity and lack of response to standard antibacterial treatment
(14). PPD testing at this stage may be negative; lymph nodes are usually
firm, painless, and rarely
inflamed and may remain so for weeks, months, or even years until the condition becomes aggressive and
may present with local inflammatory symptoms such as fistulization and/or drainage, similar to the
present case; draining of necrotic glands over time is also reported, and this evolution usually does
not accompany symptoms such as fever. The diagnosis of tuberculous lymphadenitis is established by
microbiological analysis of aspirated pus via fine needle or fistula secretion; and if necessary, biopsy
of the lymphadenopathy; although biopsy may suggest tuberculosis due to the presence of granulomatous
lesions, cultures are positive in 70-80% of cases, with molecular techniques Dot-ELISA and PCR currently
being much more sensitive (93.2%) and specific, as well as rapid (15). In
this case, treatment
initiation was based on GeneXpert profiling for TB; not on culture, staining, and microscopy, which were
negative. Therefore, the World Health Organization (WHO) recommends PCR and/or NAAT tests for the
analysis of respiratory and non-respiratory samples. Singh P, in their review, found that 17 of 19 cases
of inguinal tuberculous lymphadenitis were diagnosed using the Xpert MTB/RIF method, and the other tests
yielded contradictory results (14). It is concluded that tuberculosis
should be considered in the
differential diagnosis of any disease affecting a peripheral lymph node, especially in the context of
endemic regions and/or active disease; furthermore, it is necessary to determine on a larger scale the
sensitivity and specificity of molecular tests to agree on the method for the diagnosis of
extrapulmonary tuberculosis.
The case underscores the need to maintain a high index of suspicion for extrapulmonary tuberculosis,
even in the absence of obvious pulmonary signs. Similarly, the importance of using advanced molecular
techniques, such as GeneXpert, in the diagnosis of tuberculous lymphadenitis when conventional tests are
inconclusive, is highlighted. Additional, large-scale studies are essential to validate the sensitivity
and specificity of these tests in similar contexts and, ultimately, to establish clearer guidelines for
the diagnosis of extrapulmonary tuberculosis; therefore, it seeks to raise awareness of the
understanding of an uncommon presentation of tuberculosis, highlighting the need for a multidisciplinary
approach and early and effective clinical management to improve outcomes in patients with this
condition.
ACKNOWLEDGMENTS
We would like to express our sincere gratitude to the individuals and institutions that contributed
invaluable assistance to the completion of this study on the case of ganglionar tuberculosis with
genital involvement. Additionally, we extend our appreciation to the patient and their family, whose
cooperation and valuable information made this research possible.
Authorship contributions:
JIAP participated in the conception and design of the work, analysis and interpretation of data, critical revision, final approval, provision of study material, and acquisition of funding; WPH, in the conception and design of the work, collection and obtaining of results, analysis and interpretation of data, critical revision, final approval, study supervision and technical advice; DNGC, in the obtaining and collection of results, critical revision, final approval, provision of study material, acquisition of funding and statistical advice; JBM, in the analysis and interpretation of data, writing, final approval, acquisition of funding, statistical advice and technical advice; JMCA, in the analysis and interpretation of data, final review, final approval, provision of study material and acquisition of funding.
Financing:
Self-funded.
Declaration of conflict of interest:
The authors declare no conflict of interest.
Recevied:
September 11, 2023
Approved:
March 31, 2024
Correspondence author:
Isaac Atencio Paulino
Address:
Av. Manantial 4817, Sapallanga- Huancayo
Phone:
(+51) 930427558
E-mail:
yoel_005@yahoo.com
Article published by the Journal of the faculty of Human Medicine of the Ricardo Palma University. It is an open access article, distributed under the terms of the Creatvie Commons license: Creative Commons Attribution 4.0 International, CC BY 4.0 (https://creativecommons.org/licenses/by/1.0/), that allows non-commercial use, distribution and reproduction in any medium, provided that the original work is duly cited. For commercial use, please contact revista.medicina@urp.edu.pe.